Immunological Memory
The adaptive immune system has a memory component that allows for a rapid and large response upon re-invasion of the same pathogen. During the adaptive immune response to a pathogen that has not been encountered before, known as the primary immune response, plasma cells secreting antibodies and differentiated T cells increase, then plateau over time. As B cells and T cells mature into effector cells, a subset of the naïve populations differentiates into B and T memory cells with the same antigen specificities . A memory cell is an antigen-specific B or T lymphocyte that does not differentiate into an effector cell during the primary immune response, but that can immediately become an effector cell on re-exposure to the same pathogen. As the infection is cleared and pathogenic stimuli subside, the effector cells are no longer needed; they undergo apoptosis. In contrast, the memory cells persist in circulation.
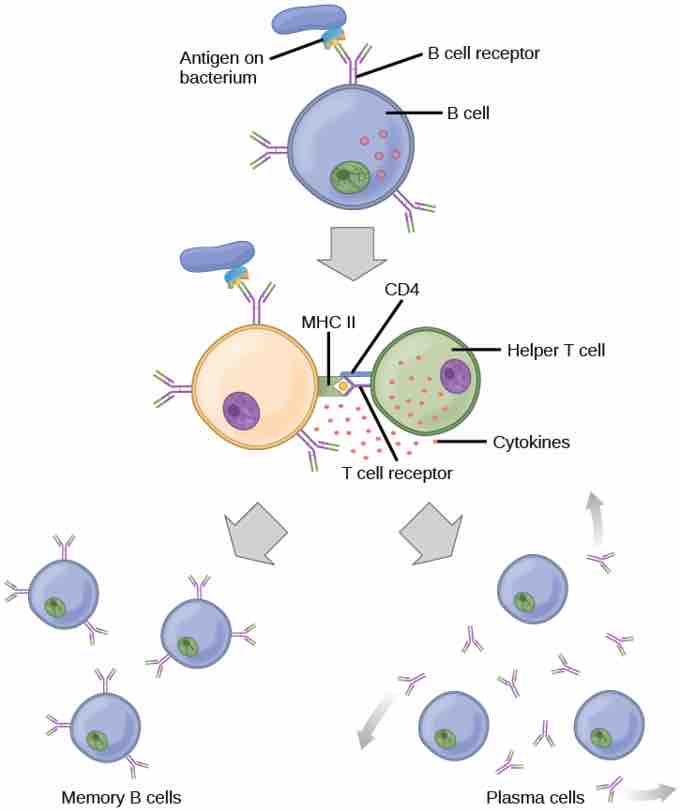
Formation of memory B cells and plasma cells
After initially binding an antigen to the B cell receptor (BCR), a B cell internalizes the antigen and presents it on MHC II. A helper T cell recognizes the MHC II–antigen complex and activates the B cell. As a result, memory B cells and plasma cells are made.
If the pathogen is not encountered again during the individual's lifetime, B and T memory cells will circulate for a few years or even several decades, gradually dying off, having never functioned as effector cells. However, if the host is re-exposed to the same pathogen type, circulating memory cells will immediately differentiate into plasma cells and TC cells without input from APCs or TH cells. This is known as the secondary immune response. One reason why the adaptive immune response is delayed is that it takes time for naïve B and T cells with the appropriate antigen specificities to be identified, activated, and proliferate. On reinfection, this step is skipped. The result is a more rapid production of immune defenses. Memory B cells that differentiate into plasma cells output ten to hundred-fold greater antibody amounts than were secreted during the primary response . This rapid and dramatic antibody response may stop the infection before it can even become established. Individuals may not realize they had been exposed.
Primary versus secondary immune response
In the primary response to infection, antibodies are secreted first from plasma cells. Upon re-exposure to the same pathogen, memory cells differentiate into antibody-secreting plasma cells that output a greater amount of antibody for a longer period of time.
Vaccination is based on the knowledge that exposure to noninfectious antigens, derived from known pathogens, generates a mild primary immune response . The immune response to vaccination may not be perceived by the host as illness, but still confers immune memory. When exposed to the corresponding pathogen to which an individual was vaccinated, the reaction is similar to a secondary exposure. Because each reinfection generates more memory cells and increased resistance to the pathogen, some vaccine courses involve one or more booster vaccinations to mimic repeat exposures.
Vaccination
Vaccines, often delivered by injection into the arm, result in a secondary immune response if the vaccinated individual is later exposed to that pathogen.