Rheumatic fever is an inflammatory disease that occurs following a Streptococcus pyogenes infection, such as streptococcal pharyngitis (strep throat) or scarlet fever, that affects the peri-arteriolar connective tissue. Believed to be caused by antibody cross-reactivity that can involve the heart, joints, skin, and brain; the illness typically develops two to three weeks after a streptococcal infection.
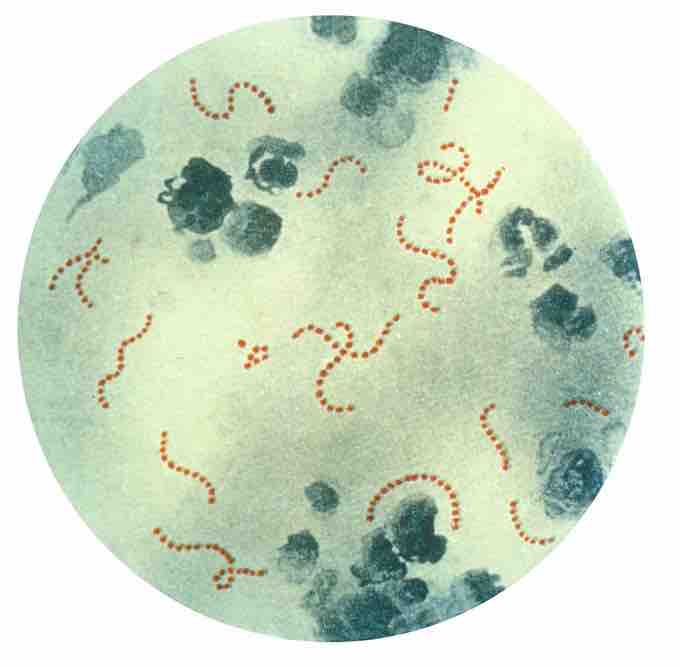
Streptococcus pyogenes bacteria
Photomicrograph of Streptococcus pyogenes bacteria, 900x Mag. A pus specimen, viewed using Pappenheim's stain. Last century, infections by S. pyogenes claimed many lives especially since the organism was the most important cause of puerperal fever and scarlet fever.
Acute rheumatic fever commonly appears in children between the ages of six and 15, with only 20% of first-time attacks occurring in adults. The illness is so named because of its similarity in presentation to rheumatism.
This cross-reactivity is a Type II hypersensitivity reaction and is termed molecular mimicry. During a Streptococcus infection, mature antigen-presenting cells, such as B cells, present the bacterial antigen to CD4-T cells which differentiate into helper T2 cells. In turn, Helper T2 cells activate the B cells to become plasma cells and induce the production of antibodies against the cell wall of Streptococcus. However the antibodies may also react against the myocardium and joints, producing the symptoms of rheumatic fever.
Diagnosis of rheumatic fever can be made when two of the major criteria, or one major plus two minor criteria, are present along with evidence of streptococcal infection.
The major criteria for diagnosis include:
- Arthritis in several large joints (polyarthritis)
- Heart inflammation (carditis)
- Nodules under the skin (subcutaneous skin nodules)
- Rapid, jerky movements (chorea, Sydenham chorea)
- Skin rash (erythema marginatum)
Minor Criteria:
- Fever of 38.2–38.9 °C (101–102 F)
- Arthralgia: Joint pain without swelling (Cannot be included if polyarthritis is present as a major symptom)
- Raised erythrocyte sedimentation rate or C reactive protein
- Leukocytosis
- ECG showing features of heart block, such as a prolonged PR interval (Cannot be included if carditis is present as a major symptom)
- Previous episode of rheumatic fever or inactive heart disease.
Acute rheumatic fever is treated with antibiotics and anti-inflammatory medications such as aspirin and corticosteroids.