Circulatory health can be measured in a variety of ways as follows.
Pulse
While a simple pulse rate measurement can be achieved by anyone, trained medical staff are capable of much more accurate measurements. Radial pulse is commonly measured using three fingers: the finger closest to the heart is used to occlude the pulse pressure, the middle finger is used to get a crude estimate of blood pressure, and the finger most distal to the heart is used to nullify the effect of the ulnar pulse as the two arteries are connected via the palmar arches.
Where more accurate or long-term measurements are required, pulse rate, pulse deficits, and much more physiologic data are readily visualized by the use of one or more arterial catheters connected to a transducer and oscilloscope. This invasive technique has been commonly used in intensive care since the 1970's. The rate of the pulse is observed and measured by tactile or visual means on the outside of an artery and recorded as beats per minute (BPM). The pulse may be further indirectly observed under light absorbencies of varying wavelengths with assigned and inexpensively-reproduced mathematical ratios. Applied capture of variances of light signal from the blood component hemoglobin under oxygenated vs. deoxygenated conditions allows the technology of pulse oximetry.
Heart Rate
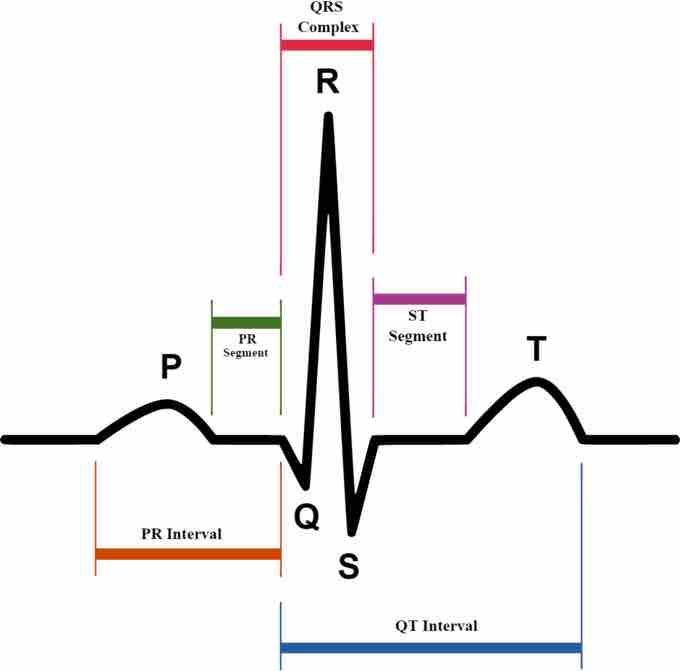
Heart rate can be measured by listening to the heart directly though the chest, traditionally using a stethoscope. For more accurate or long-term measurements, electrocardiography may be used. During each heartbeat, a healthy heart has an orderly progression of depolarization that starts with pacemaker cells in the sinoatrial (SA) node, spreads out through the atrium, passes through the atrioventricular node down into the bundle of His and into the Purkinje fibers, and down and to the left throughout the ventricles. This organized pattern of depolarization can be detected through electrodes placed on the skin and recorded as the commonly seen ECG tracing. ECG provides a very accurate means to measure heart rate, rhythm, and other factors such as chamber sizing, as well as identifying possible regions of damage.
ECG Graph
ECG graph of a normal heartbeat.
Blood Pressure
Arterial pressure is most commonly measured via a sphygmomanometer, which historically used the height of a column of mercury to reflect the circulating pressure. Blood pressure values are generally reported in millimeters of mercury (mmHg), though aneroid and electronic devices do not use mercury. For each heartbeat, blood pressure varies between systolic and diastolic pressures. Systolic pressure is peak pressure in the arteries, which occurs near the end of the cardiac cycle when the ventricles are contracting. Diastolic pressure is minimum pressure in the arteries, which occurs near the beginning of the cardiac cycle when the ventricles are filled with blood. An example of normal measured values for a resting, healthy adult human is 120 mmHg systolic and 80 mmHg diastolic.
Hypertension refers to abnormally high arterial pressure, as opposed to hypotension, when it is abnormally low. Along with body temperature, respiratory rate, and pulse rate, blood pressure is one of the four main vital signs routinely monitored by medical professionals and healthcare providers.
Measuring pressure invasively by penetrating the arterial wall to take the measurement is much less common and usually restricted to a hospital setting. The noninvasive auscultatory and oscillometric measurements are simpler and faster than invasive measurements, require less expertise, have virtually no complications, are less unpleasant and painful for the patient. However, noninvasive methods may yield somewhat lower accuracy and small systematic differences in numerical results. Noninvasive measurement methods are more commonly used for routine examinations and monitoring.
The Auscultatory Method
The auscultatory method uses a stethoscope and a sphygmomanometer . This comprises an inflatable cuff placed around the upper arm at roughly the same vertical height as the heart, attached to a mercury or aneroid manometer. The mercury manometer, considered the gold standard, measures the height of a column of mercury, giving an absolute result without need for calibration.

Typical Tools of Auscultatory Measurement
Shown here are a stethoscope and a sphygmomanometer, which are used for ascultatory measurement.
A cuff of appropriate size is fitted smoothly and snugly, then inflated manually by repeatedly squeezing a rubber bulb until the artery is completely occluded. Listening with the stethoscope to the brachial artery at the elbow, the examiner slowly releases the pressure in the cuff. When blood just starts to flow in the artery, the turbulent flow creates a "whooshing" or pounding (first Korotkoff sound). The pressure at which this sound is first heard is the systolic blood pressure. The cuff pressure is further released until no sound can be heard (fifth Korotkoff sound), at the diastolic arterial pressure. The auscultatory method is the predominant method of clinical measurement.