The adaptive immune system, also known as the specific immune system, is composed of highly-specialized systemic cells and processes that eliminate or prevent pathogenic growth. The adaptive immune system works to protect and heal the body when the innate immune system fails. It provides the body with the ability to recognize and remember specific pathogens through their antigens. This mechanism allows the immune system to mount stronger attacks each time the pathogen is encountered, thus preparing itself for future challenges and preventing reinfection by the same pathogen.
Functions of the Adaptive Immune System
The adaptive immune system starts to work after the innate immune system is activated. If an infection progresses despite the inflammation, fever, natural killer (NK) cell and phagocyte activity of the innate immune system, a more coordinated response is required in order to destroy the pathogen. The adaptive immune response occurs a few days after the innate immune response is initiated. The major functions of the adaptive immune system include:
- The recognition of specific "non-self" antigens in the presence of "self" during the process of antigen presentation
- The generation of responses that are tailored to maximally eliminate specific pathogens or pathogen-infected cells
- The development of immunological memory in which each pathogen is "remembered" by a signature antibody , which can then be called upon to quickly eliminate a pathogen should subsequent infections occur.
Formation of Adaptive Immunity
Adaptive immunity is triggered when a pathogen evades the innate immune system for long enough to generate a threshold level of an antigen. An antigen is any molecule that induces an immune response, such as a toxin or molecular component of a pathogen cell membrane, and is unique to each species of pathogen. A typical adaptive immune response includes several steps:
- The antigen for the pathogen is taken up by an antigen-presenting cell (APC), such as a dendritic cell or macrophage, through phagocytosis.
- The APC travels to a part of the body that contains immature T and B cells, such as a lymph node.
- The antigen is processed by the APC and bound to MHC class II receptors and MHC class I receptors on the cell membrane of the APC.
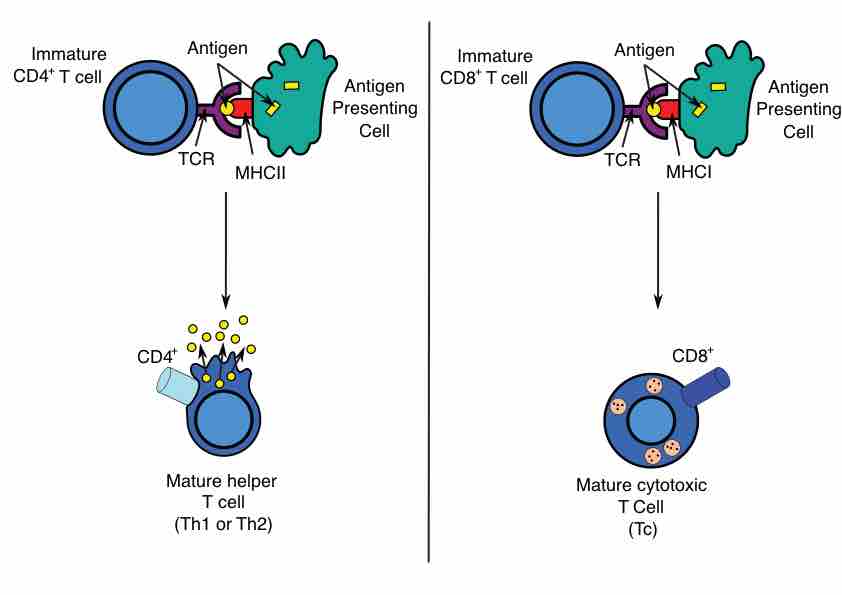
- The antigen is presented to immature helper T cells and cytotoxic T cells through binding the MHC II (helper T) or MHC I (cytotoxic T) to T-cell receptors.
- These T lymphocytes mature and proliferate. Helper T cells activate B cells, which proliferate and produce antibodies specific to the antigen, while cytotoxic T cells destroy pathogens that bear the antigen that was presented to them by the APCs.
- Memory B and T cells are formed after the infection ends.
Antigen Presentation
Antigen presentation stimulates T cells to become either "cytotoxic" CD8+ cells or "helper" CD4+ cells. Cytotoxic cells directly attack cells carrying certain foreign or abnormal molecules on their surfaces. Helper T cells, or Th cells, coordinate immune responses by communicating with other cells. In most cases, T cells only recognize an antigen if it is carried on the surface of a cell by one of the body's own MHC, or major histocompatibility complex, molecules.
Immunological Memory
When B cells and T cells are activated, some become memory cells. Throughout the lifetime of an animal, these memory cells form a database of effective B and T lymphocytes. Upon interaction with a previously-encountered antigen, the appropriate memory cells are selected and activated. In this manner, the second and subsequent exposures to an antigen produce a stronger and faster immune response. This is "adaptive" because the body's immune system prepares itself for future challenges, which can stop an infection by the same pathogen before it can even cause symptoms.
Immunological memory can either be in the form of passive short-term memory or active long-term memory. Passive memory is usually short-term, lasting between a few days and several months, and is particularly important for newborn infants, who are given passive memory from maternal antibodies and immune cells before birth. Active immunity is generally long-term and can be acquired by infection followed by B cells and T cells activation, or artificially acquired by vaccines in a process called immunization.
The memory system does have a few flaws. Pathogens that undergo mutation often have different antigens than those known by memory B and T cells, meaning that different strains of the same pathogen can avoid the memory-enhanced immune response. Additionally, the memory cell function enables the development of hypersensitivity disorders, such as allergies and many chronic diseases (like multiple sclerosis or myasthenia gravis). In these cases, memory cells form for an antigen that elicits an immune response without actually being caused by a pathogen, which leads to immune system mediated-damage to the body from mast cell, antibody, or T-cell mediated activities and inflammation.

Antibody
An antibody is made up of two heavy chains and two light chains. The unique variable region allows an antibody to recognize its matching antigen