Airway Resistance
Airway resistance is the resistance to flow of air caused by friction with the airways, which includes the conducting zone for air, such as the trachea, bronchi and bronchioles. The main determinants of airway resistance are the size of the airway and the properties of the flow of air itself.
Size of the Airway
Resistance in an airway is inversely proportional to the radius of the airway. However the ratio for this relationship is not 1:1. Below is the equation for calculating airway resistance (R).
The most important part of this formula is radius of the airway (r). A common example is that if one were to double the diameter of an airway (thus doubling the radius as well) the resistance of the airway would drop by a factor of 16. This mathematical property between radius and resistance is consistent for all tubes, and is often applied to the blood vessels in the cardiovascular system.
The radius of the airways of the conducting zone become smaller as air goes deeper into the lungs. Therefore the resistance to air in the bronchi is greater than the resistance to air in the trachea. The number of airways also plays a large role in the resistance to air, with more airways reducing resistance because there are more paths for the air to flow into. Therfore, despite the fact that the terminal bronchioles are the smallest airway in terms of radius, their high number compared to the larger airways means that the bronchi actually have greater resistance because there are less of them compared to the terminal bronchioles. Another important fact is that airway resistance is inversely related to lung volumes because the airways expand a bit as they inflate, so the airways in a fully inflated lung will have lower resistance than a lung after exhalation.
Airway resistance can be indirectly measured with body plethysmography, which is an instrument used for measuring changes in volume within a structure, such as the airways. The resistance of the airways is an important indicator of lung health and function and can be used to diagnose lung diseases.
The size of the airways, and thus the resistance can change based on the health and conditions of the lungs. Most lung diseases increase airway resistance in many different ways. For example, in asthma attacks the bronchioles spasm and constrict, which increases resistance. Emphysema also increases airway resistance because the lung tissue becomes too pliable and it the airways become more difficult to hold open by the flow of air.
Flow of Air
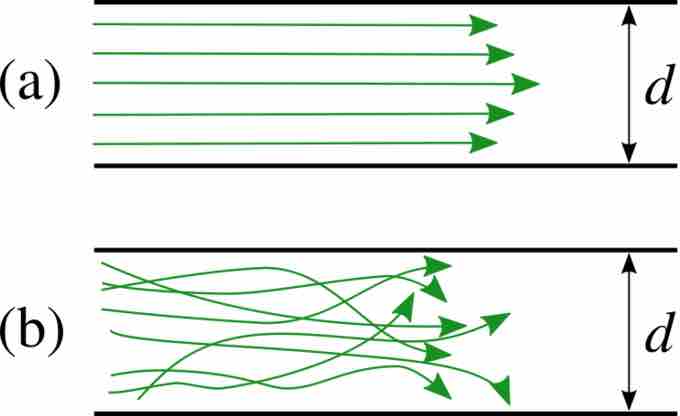
The air that flows through the lungs varies considerably in the properties of the flow of air. The air flow can either be turbulant, transitional or laminar based on the airway. Laminar flow involves an orderly and concentric distribution of layers of air particles and tends to occur in smaller airways, and has lower resistance. Turbulent flow is disorganized distribution of the layers of air and tends to occur in larger airways and places where the airways branch, and has a higher resistance. Transitional flow occurs in places that branch within smaller airways, in which the air flow becomes in between laminar and turbulent flow and has moderate resistance. The relationship between resistance and type of airflow is difficult to measure and apply, but some mathematical models (such as the Reynold's number) can provide a rough estimate.
Laminar and Turbulent Flow
Laminar flow (a) has orderly layers and low resistance. Turbulent flow (b) has disorganized layers and high resistance.