Extracellular Immune Avoidance
A pathogen's success depends on its ability to evade the host's immune responses. Thus, pathogens have evolved several methods that allow them to successfully infect a host by evading the immune system's detection and destruction. Bacteria usually overcome physical barriers by secreting enzymes that digest the barrier in the manner of a type II secretion system. They also use a type III secretion system that allows bacteria to insert a hallow tube, which provides proteins a direct route to enter the host cell. These proteins often shutdown the defenses of the host.
Some pathogens avoid the immune system by hiding within the cells of the host, a process referred to as intracellular pathogenesis. The pathogen hides inside the host cell where it is protected from direct contact with the complement, antibodies, and immune cells. A lot of pathogens release compounds that misdirect or diminish the host's immune response. Some bacteria even form biofilms which protect them from the proteins and cells of the immune system. Many successful infections often involve biofilms. Some bacteria create surface proteins, such as Streptococcus, that will bind to antibodies making them ineffective.
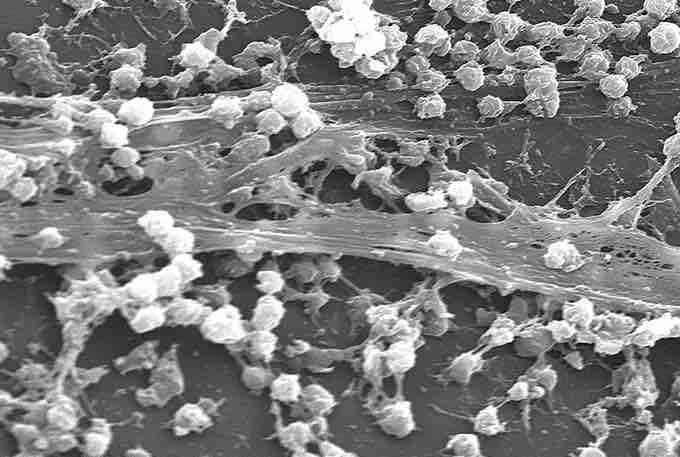
Staphylococcus aureus biofilm
Staphylococcus aureus forming a biofilm on a catheter.
Other pathogens invade the body by changing the non-essential epitopes on their surface rapidly while keeping the essential epitopes hidden. This is referred to as antigenic variation. HIV rapidly mutates so the proteins that are on its viral envelope, which are essential for its entry into the host's target cell, are consistently changing. The constant change of these antigens is why vaccines have not been created. Another common strategy that is used is to mask antigens with host molecules in order to evade detection by the immune system. With HIV, the envelope covering the viron is created from the host cell's outermost membrane making it difficult for the immune system to identify as a non-self structure.