A transient ischemic attack (abbreviated as TIA, often referred to as mini stroke) is a transient episode of neurologic dysfunction caused by ischemia—either focal brain, spinal cord, or retinal—without acute infarction (tissue death).
TIAs share the same underlying etiology (cause) as strokes: a disruption of cerebral blood flow (CBF). TIAs and strokes cause the same symptoms. Unlike a stroke, the symptoms of a TIA can resolve within a few minutes or 24 hours. Brain injury may still occur in a TIA lasting only a few minutes. Having a TIA is a risk factor for eventually having a stroke or a silent stroke.
Symptoms
Symptoms vary widely from person to person, depending on the area of the brain involved. The most frequent symptoms include:
- temporary loss of vision (typically amaurosis fugax)
- difficulty speaking (aphasia)
- weakness on one side of the body (hemiparesis)
- numbness or tingling (paresthesia), usually on one side of the body.
There have also been cases of temporary and partial paralysis affecting the face and tongue of the afflicted. The symptoms of a TIA are short-lived and usually last a few seconds to a few minutes, and most symptoms disappear within 60 minutes. Some individuals may have a lingering feeling that something odd happened to the body. Dizziness, lack of coordination, or poor balance are also symptoms related to TIA. Symptoms vary in severity.
Causes
The most common cause of a TIA is an embolus that occludes an artery in the brain. This usually arises from a dislodged atherosclerotic plaque in one of the carotid arteries or from a thrombus (i.e., a blood clot) in the heart because of atrial fibrillation. In a TIA, the blockage period is very short-lived and hence there is no permanent damage.
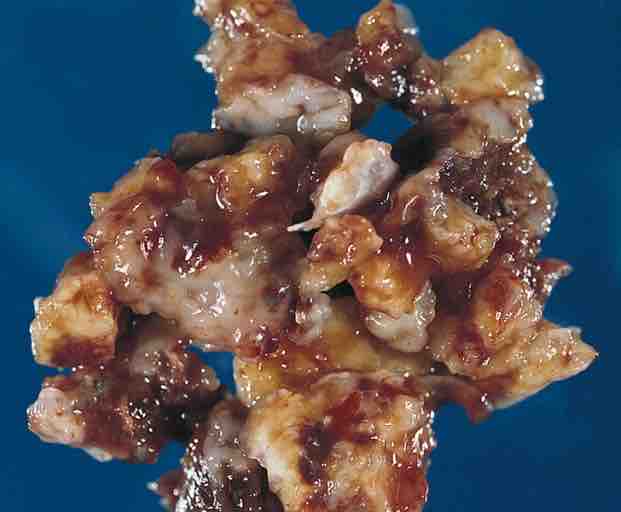
Heart-Great Vessels: Cardiac Myxoma
This image is the left atrial mass of a 71 year old man who had TIAs.
Other reasons include excessive narrowing of large vessels resulting from an atherosclerotic plaque and increased blood viscosity caused by some blood diseases. TIA is related to other medical conditions such as hypertension, heart disease (especially atrial fibrillation), migraine, cigarette smoking, hypercholesterolemia, and diabetes mellitus.
Risk Factors
Risk factors include:
- Family history of stroke or TIA
- People 55 years or older
- Males have a slightly higher risk of TIA than females, but females are more likely to die from a stroke.
- African Americans generally tend to have a high risk of dying from a stroke, chiefly due to high blood pressure and uncontrolled diabetes.
Prevention and Treatment
A TIA may be prevented by changes in lifestyle. Although most of these recommendations have no solid empirical data, most medical professionals believe them to be so. These include:
- Avoiding smoking
- Cutting down on fats and cholesterol to help reduce plaque build up
- Eating a healthy diet including plenty of fruits and vegetables
- Limiting sodium in the diet, thereby reducing blood pressure
- Exercising regularly
- Moderating alcohol intake
- Maintaining a normal weight
- Controlling blood pressure and keeping blood sugars under control
The mainstay of treatment following acute recovery from a TIA should be to diagnose and treat the underlying cause. It is not always immediately possible to tell the difference between a CVA (stroke) and a TIA. Most patients who are diagnosed at a hospital's emergency department as having suffered from a TIA will be discharged home and advised to contact their primary physician to organize further investigations. A TIA can be considered as the last warning. The reason for the condition should be immediately examined by imaging of the brain.
The initial treatment is aspirin, second line is clopidogrel (PLAVIX), third line is ticlopidine. If TIA is recurrent after aspirin treatment, the combination of aspirin and dipyridamole is needed (Aggrenox).