Blood pressure generally refers to the arterial pressure in the systemic circulation. However, measurement of pressures in the human venous system and the pulmonary vessels play an important role in intensive care medicine and are physiologically important in ensuring proper return of blood to the heart, maintaining flow in the closed circulatory system.
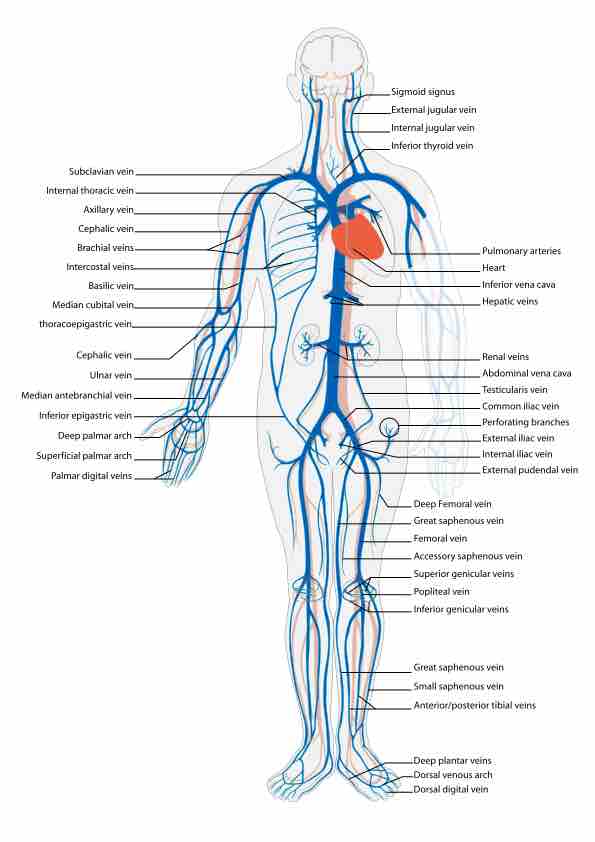
The Human Venous System
Veins (from the Latin vena) are blood vessels that carry blood towards the heart. Veins differ from arteries in structure and function; arteries are more muscular than veins, while veins are often closer to the skin and contain valves to help keep blood flowing toward the heart.
Systemic Venous Pressure
Venous pressure is the vascular pressure in a vein or the atria of the heart. It is much lower than arterial pressure, with common values of 5 mmHg in the right atrium and 8 mmHg in the left atrium. Variants of venous pressure include:
- Central venous pressure, a good approximation of right atrial pressure, which is a major determinant of right ventricular end diastolic volume.
- Jugular venous pressure (JVP), the indirectly observed pressure over the venous system. It can be useful in differentiating different forms of heart and lung disease.
- Portal venous pressure or the blood pressure in the portal vein. It is normally 5–10 mmHg.
Vein Structure and Function
In general, veins function to return deoxygenated blood to the heart, and are essentially tubes that collapse when their lumens are not filled with blood. Compared with arteries, the tunica media of veins, which contains smooth muscle or elastic fibers allowing for contraction, is much thinner, resulting in a compromised ability to deliver pressure. The actions of the skeletal-muscle pump and the thoracic pump of breathing during respiration aid in the generation of venous pressure and the return of blood to the heart.
The pressure within the circulatory circuit as a whole is mean arterial pressure (MAP). This value is a function of the cardiac output (total blood pumped) and total peripheral resistance (TPR). TPR is primarily a function of the resistance of the systemic circulation. The resistance to flow generated by veins, due to their minimal ability to contract and reduce their diameter, means that regulation of blood pressure by veins is minimal in contrast to that of muscular vessels, primarily arterioles. The latter can actively contract, reduce diameter, and increase resistance and pressure. In addition, veins can easily distend or stretch. A vein's ability to increase in diameter in response to a given blood volume also contributes to the very low pressures within this segment of the circulatory system.
Pooling and Fainting
Standing or sitting for a prolonged period of time can cause low venous return in the absence of the muscle pump, resulting in venous pooling (vascular) and shock. Fainting can occur, but usually baroreceptors within the aortic sinuses initiate a baroreflex, triggering angiotensin II and norepinephrine release and consequent vasoconstriction and heart rate increases to augment blood flow return.
Neurogenic and hypovolemic shock can also cause fainting. The smooth muscles surrounding the veins become slack and the veins fill with the majority of the blood in the body, keeping blood away from the brain and causing unconsciousness. Jet pilots wear pressurized suits to help maintain their venous return and blood pressure, since high-speed maneuvers increase venous pooling in the legs. Pressure suits specifically squeeze the lower extremities, increasing venous return to the heart. This ensures that end diastolic volumes are maintained and that the brain will receive adequate blood, preventing loss of consciousness.