An alveolus is an anatomical structure that has the form of a hollow cavity. Its plural is alveoli, from the Latin alveolus, meaning little cavity.
Found in the lung parenchyma, the pulmonary alveoli are the terminal ends of the respiratory tree that outcrop from either alveolar sacs or alveolar ducts; both are sites of gas exchange with blood.
The alveolar membrane is the gas-exchange surface. Carbon-dioxide-rich blood is pumped from the rest of the body into the alveolar blood vessels where, through passive diffusion, it releases its carbon dioxide and absorbs oxygen into the blood vessels.
Anatomy of the Alveoli
The alveoli are located in the respiratory zone of the lungs, at the distal termination of the alveolar ducts. These air sacs are at the end points of the respiratory tract.
There are approximately 700 million alveoli in the lungs, covering a total surface area of about 70 m2, which is a considerably larger surface area relative to volume. The large surface area makes gas exchange with the bloodstream more efficient.
The alveoli are highly elastic, so the alveoli can stretch as they are filled with air during inhalation. They then spring back during exhalation in order to expel the carbon-dioxide-rich air.
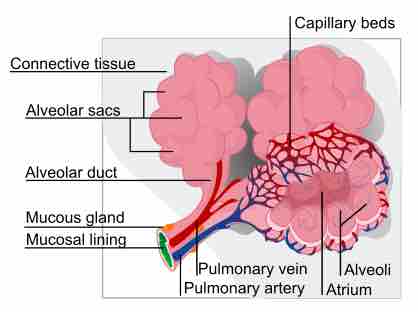
Pulmonary alveolus
A diagram of the pulmonary alveolus.
Histology
The alveoli consist of an extremely thin epithelial layer and an extracellular matrix (a fluid space made of collagen and elastin that contains no cells); it is surrounded by many capillaries, the tiniest type of blood vessel.
The fluid extracellular matrix supports the structure of the alveoli and allows gases to dissolve in water, making passive diffusion of those gases with the capillaries possible. In some alveolar walls there are pores between alveoli called the pores of Kohn, that connect alveoli in order to equalize air pressure between the different sacs of an alveolus.
There are two major types of epithelial cells found in alveoli (pneumocytes):
- Type I (Squamous Alveolar) cells: These form the structure of an alveolar wall. They are extremely thin, and permeable, which facilitates gas exhange with the capillaries. They can't undergo mitosis, making them vulnerable to injury.
- Type II (Great Alveolar) cells: These are the site of surfactant production in the lungs, making them critical for maintaining the elastic recoil of the lung. They are more common than type I cells and can undergo mitosis, and may even proliferate into new type I cells when necessary.
Besides these epithelium cells, there are many macrophages found in the alveoli that provide immune system defense of the alveoli from pathogens and foreign material.
Physiology of the Alveoli
The surfactant produced by type II epithelial cells is very important for maintaining the elastic recoil of the lungs. It is a lipoprotein with hydrophilic and hydrophobic ends that reduce the amount of surface tension from water in the lungs. Without surfactant, the surface tension would cause the lungs to collapse during exhalation, making normal breathing impossible.
Surfactant is first produced by human lungs between 24 and 28 weeks in the womb, and many infants born prematurely do not have enough surfactant to breathe on their own after birth. Surfactant replacement therapy is necessary to save the lives of these premature births.
The alveoli are the site of alveolar ventilation, and are not normally considered dead space. However, alveoli that are injured and can no longer contribute to gas exchange become alveolar dead space.
This is a common occurrence in people with lung diseases like COPD (chronic pulmonary obstructive disorder, i.e., emphysema and bronchitis) or restrictive lung diseases like pulmonary fibrosis, in which scarring of the lung tissue hinders gas exchange in the alveoli, or lung infections like pnuemonia.
Physiological dead space is the sum of normal anatomical dead space and alveolar dead space, and can be used to determine the rate of ventilation (gas exchange) in the lungs. When any type of dead space increases, the rate of ventilation in the lungs will decrease.