Acarbose
- Article Author:
- Lindsey McIver
- Article Editor:
- Jayson Tripp
- Updated:
- 8/10/2020 10:51:58 PM
- For CME on this topic:
- Acarbose CME
- PubMed Link:
- Acarbose
Indications
Acarbose is FDA approved for the treatment of adults with type 2 diabetes mellitus as an adjunct to diet only or diet and exercise, depending on the patient's health status.
Based on the combined data of six placebo-controlled trials in patients with type 2 diabetes mellitus using acarbose as monotherapy, researchers noted the following changes from baseline glycosylated hemoglobin (hemoglobin A1c) by dose:
- Acarbose, 25 mg three times daily, decrease by 0.44
- Acarbose, 50 mg three times daily, decrease by 0.77
- Acarbose, 100 mg three times daily, decrease by 0.74
- Acarbose, 200 mg three times daily, decrease by 0.86
- Acarbose, 300 mg three times daily, decrease by 1.00
Although the acarbose 300 mg three times daily regimen is superior to lower doses at lowering hemoglobin A1c, the approved maximum daily dose of acarbose is 100 mg three times daily. There is no statistically significant difference in hemoglobin A1c lowering between the 50 mg three times daily regimen, 100 mg three times daily regimen, and the 200 mg three times daily regimen.
Acarbose is not FDA approved for the treatment of type 1 diabetes mellitus; however, studies have evaluated the safety and efficacy in this patient population. In a study of 121 patients with type 1 diabetes mellitus, acarbose 50 mg three times daily for two weeks, followed by 100 mg three times daily, was found to reduce 2-hour postprandial glucose significantly. There were no differences between the placebo group and the acarbose group in hemoglobin A1c lowering or episodes of hypoglycemia.[1] In two subsequent, single-center, placebo-controlled studies, 40 patients with type 1 diabetes mellitus were given metformin for six months after acarbose replaced metformin. The research demonstrated acarbose significantly decreased the 2-hour postprandial blood glucose concentration when compared to baseline. When compared to metformin therapy, the acarbose therapy group showed a statistically significant decrease in low-density lipoprotein (calculated), triglycerides, and total cholesterol. Acarbose use also led to a statistically significant reduction in regular insulin use.[2]
Acarbose is not FDA approved for the treatment of prediabetes. Acarbose has also undergone evaluation as a potential pharmacologic option for preventing the progression from prediabetes to type 2 diabetes mellitus. In a study of patients with impaired glucose tolerance tests, participants were randomized to acarbose 100 mg three times daily or placebo three times daily. Thirty-two percent of the acarbose group developed type 2 diabetes mellitus compared to 42% in the placebo group, resulting in a statistically significant hazard ratio of 0.75.[3]
The effect of acarbose on weight loss has also been a target of research. In an analysis of post-marketing data of 67,682 patients, the data revealed acarbose to decrease body weight significantly, independent of baseline body weight. It also was found to significantly reduce fasting plasma glucose, postprandial glucose, hemoglobin A1c, and postprandial glucose concentrations.[4]
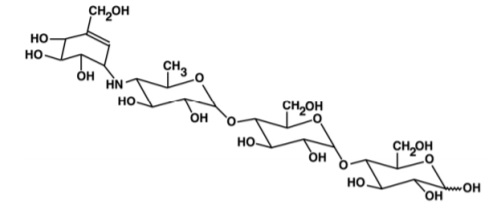
Mechanism of Action
Acarbose is a complex oligosaccharide that acts as a competitive, reversible inhibitor of pancreatic alpha-amylase and membrane-bound intestinal alpha-glucoside hydrolase. Pancreatic alpha-amylase hydrolyzes complex carbohydrates to oligosaccharides in the small intestine. Intestinal alpha-glucosidase hydrolase breaks down oligosaccharides, trisaccharides, and disaccharides (sucrose, maltose) to monosaccharides (glucose, fructose) in the brush border of the small intestine. By delaying the digestion of carbohydrates, acarbose slows glucose absorption, resulting in a reduction of postprandial glucose blood concentrations.
Pharmacokinetics
Absorption
Acarbose acts locally in the gastrointestinal (GI) tract with low systemic bioavailability (less than 2% gets absorbed as the active drug, and 35% as metabolites).
Metabolized
Acarbose is metabolized in the GI tract by intestinal bacteria and digestive enzymes.
Excretion
The kidneys excrete the absorbed drug, and 51% of an oral dose gets excreted in feces.
Administration
Acarbose is available as a 25 mg, 50 mg, or 100 mg oral tablet. It should be administered orally three times daily with the first bite of each meal. Initial dosing is 25 mg orally three times daily; however, starting with once-daily dosing may limit GI adverse effects. From 25 mg by mouth three times daily, the dose can be titrated every 4 to 8 weeks to reach desired glycemic control while limiting GI adverse effects. The maximum daily dose is 100 mg three times daily.
- If the patient weighs less than 60 kg, the dose should not exceed 50 mg three times daily.
- Patients with renal dysfunction (serum creatinine greater than 2.0 mg/dL) have not been studied.
- Safety and efficacy have not undergone evaluation in pediatric patients.
- Studies have not established the safety of acarbose in pregnant patients.
- Nursing mothers should not use acarbose.
Drug-Drug Interactions
- Acarbose may decrease the bioavailability of digoxin and valproic acid.
- Acarbose may increase hypoglycemic risk when combined with other anti-diabetic agents that cause hypoglycemia.
- Digestive enzymes, including amylase, lipase, and protease, may decrease the effectiveness of acarbose.
- Therapy requires monitoring with other agents that affect blood glucose concentrations.
Adverse Effects
The most common adverse effects are GI symptoms, including flatulence, diarrhea, and abdominal pain. A high carbohydrate diet may worsen the GI adverse effects. GI symptoms tend to become reduced throughout treatment.
Elevated serum transaminases may occur during acarbose therapy. Elevations usually are asymptomatic and reversible once stopping drug therapy.
Hypoglycemia should not occur with acarbose monotherapy. However, the therapy can increase the risk of hypoglycemia when used with antidiabetic agents that cause hypoglycemia such as sulfonylureas or insulins.
Post-marketing reports include cases where there were rare occurrences of pneumatosis cystoides intestinalis with alpha-glucosidase inhibitor use.
Contraindications
Acarbose use is contraindicated in patients with known hypersensitivity, diabetic ketoacidosis, liver cirrhosis, inflammatory bowel disease, or colonic ulceration. It also is contraindicated in patients with intestinal obstruction or those predisposed to intestinal obstruction; patients with chronic intestinal disease, including those who have issues with digestion or absorption; or conditions that will be worsened by the increased gas formation in the intestine.
Monitoring
One- to 2-hour postprandial blood glucose concentrations and glycosylated hemoglobin require monitoring to assess efficacy. Serum transaminase concentrations should be checked every three months for the first year of therapy. The clinician should decrease the dose or discontinue therapy if concentrations become elevated during treatment.
Toxicity
Overdose with acarbose will not cause hypoglycemia but may increase GI adverse effects. If an overdose occurs, patients should not have food or beverages that contain carbohydrates for 4 to 6 hours.
If a patient experiences hypoglycemia while taking acarbose in combination with other anti-diabetic medications, the patient should receive instructions to use glucose (gel, tablets, etc.) as acarbose will prevent the breakdown of sucrose (table sugar) and delay glucose absorption, therefore, failing to correct hypoglycemia quickly. Severe hypoglycemia may require intravenous glucose or intramuscular glucagon administration.
Enhancing Healthcare Team Outcomes
Acarbose is a commonly used medication for the management of type 2 diabetes mellitus. While the drug is useful, it is not a great agent when used as monotherapy. Because the drug works in the gastrointestinal system, it's most common adverse effects are gastrointestinal upset/bloating. Hence, the nurse practitioner, a pharmacist, and the primary care provider must educate the patient on how to use the drug. Further, patients should receive counsel to avoid cola beverages, as the abdominal symptoms may worsen. While hypoglycemia is extremely rare with this agent, if it occurs, one should consider other antidiabetic drugs as the cause. The patient should be treated for hypoglycemia and then counseled on how to prevent further episodes of low sugar. Only through patient education can the side effects be limited, and as with any medication, acarbose management is best by an interprofessional healthcare team across various disciplines. [Level V]