Achilles Tendonitis
- Article Author:
- Miguel Medina Pabón
- Article Editor:
- Usker Naqvi
- Updated:
- 8/8/2020 9:02:33 PM
- For CME on this topic:
- Achilles Tendonitis CME
- PubMed Link:
- Achilles Tendonitis
Introduction
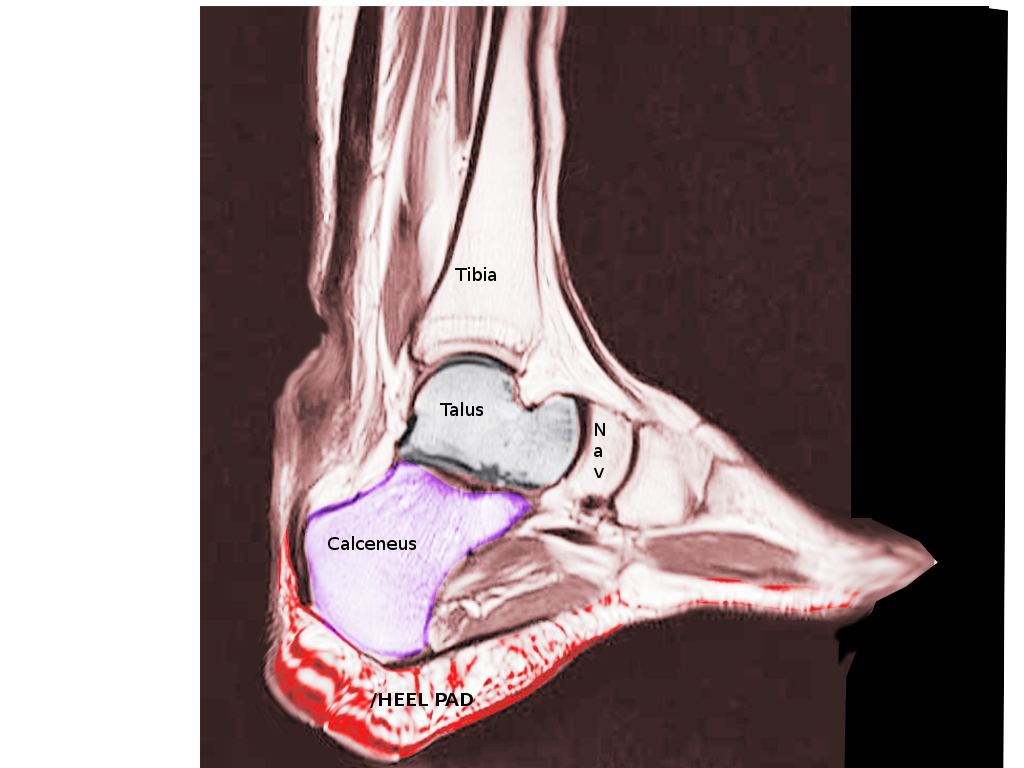
The Achilles tendon ranks as the strongest tendon in the human body. This tendon connects the plantaris, gastrocnemius, and soleus to the calcaneus bone. A sheath-like structure comprised of a single layer of cells surrounds the tendon; this is called the paratenon. The paratenon supplies a significant portion of the blood supply to the tendon. Studies have shown an area of hypovascularity 2 to 6 cm proximal to calcaneal insertion; this is a common area of injury. The Achilles tendon allows the calf muscles to act on the heel, which is necessary for walking or running. The tendon has several causes of injury as well as several locations that are the most commonly injured. In this review, we will discuss insertional tendinitis, mid-body Achilles tendonitis, paratenonitis, and tendon rupture. Please refer to the tendinosis chapter for more information regarding the histological differences between tendinitis and tendinosis.
Etiology
The causes and mechanisms of Achilles tendinopathy (AT) include the following:
- Intrinsic factors: This includes anatomic factors, age, sex, metabolic dysfunction,[1] foot cavity, dysmetria, muscle weakness, imbalance, gastrocnemius dysfunction,[2] anatomical variation of the plantaris muscle,[3] tendon vascularization,[4] torsion of the Achilles tendons,[5] slippage of the fascicle,[6] and lateral instability of the ankle.
- Extrinsic factors: These include mechanical overload, constant effort, inadequate equipment,[7] obesity,[8] medications (corticosteroids, anabolic steroids, fluoroquinolones,)[9][10], improper footwear, insufficient warming or stretching,[11] hard training surfaces, and direct trauma, among others.[12]
Factors related to a high risk of rupture of the Achilles tendon link to advanced age due to a lack of uniformity of the tendons, slippage of the fascicles, and excessive exercise in athletes,[13] Sports minded individuals tend to have an injury at the Achilles tendon insertion site.[14]
Epidemiology
The Achilles tendon has a cumulative lifetime injury incidence of approximately 24% in athletes. Running-related injuries have a prevalence between 11% and 85% or 2.5 to 59 injuries per 1000 hours of running [15]. Results from one study cite the frequency of Achilles tendinopathy to be 1 to 2% in elite adolescent athletes [16]. Another study cited the frequency of injury as 9% in recreational athletes, [17]. The lifetime injury incidence of 2.35 per 1000 is strongly associated with sporting activities.[18][19][20] This incidence increases in older men.[21] The overall incidence rate of Achilles tendinopathy ruptures is 2.1 per 100000 person-years, and most AT ruptures occur in males, with a 3.5 to 1 male to female ratio.[22]
Pathophysiology
The Achilles tendon has two tendinous portions; one proximally and then another merging gradually distally, resulting in a single, homogenous tendon. It comprises three muscular heads; the soleus is monoarticular and the plantaris and gastrocnemius, which are biarticular. There are two sites where the mechanical tension of the tendon occurs, the medial/central portion of the paratenon and the middle part of the tendon which is the most common site of injury.[23]
Histopathology
The Achilles tendon is comprised of type I collagen fibers; these fibers are both very strong and very flexible. The tendon is covered in a thin layer of connective tissue known as paratenon, which is rich in elastin and penetrates into the tendon, keeping the collagen bundles together while allowing movement between them.[24]
The difference between tendinosis and tendinitis is that in the former there are degenerative changes in the tendon's structure and the sheath, making it more vulnerable and prone to breaking. At the cellular level, there is no evidence of an acute or recent inflammatory process. In tendinitis, the opposite happens; there is an acute inflammatory process, resulting from acute trauma, excessive use, or lack of training.[25] Paratenonitis is an inflammation of the outer layers of the tendon and encompasses conditions such as tenosynovitis and tenovaginitis.[26] This pathology generates edema and exudate with inflammatory cells, followed by a fibrinous exudate that causes crepitus and limitation of the tendinous course within the sheath. It can become chronic by developing an immature connective tissue that expands an organized fibrin network known as adhesions.[27]
One study found that the microenvironment of the Achilles tendon in rats induced the stem cells to differentiate into chondrogenic and osteogenic lineages, which predispose to tendon rupture (tendinosis). After this rupture, an inflammatory cascade appears that increases the expression of proinflammatory cytokine mRNA, matrix metalloproteinase-3 (MMP-3), cyclooxygenase-2 (COX-2), interleukin-6 (IL-6) and necrosis factor tumor alpha (TNF-a).[28]
However, the chronic inflammation induces neovascularization that promotes the rupture of the tendon, increasing disability and complexity in management.[29] In a study with rats, researchers observed that denervated tendons express morphological changes such as disorganization of the collagen network, increased production of type III collagen, hypercellularity; disfigured cells, and increased expression of NK-1R, somewhat similar changes to Achilles tendon injury.[30]
History and Physical
The term "Achilles tendinopathy" refers to tendinitis (acute inflammation) and tendinosis (chronic inflammation). It is a condition characterized by pain, inflammation, and stiffness of the Achilles tendon. The inflammation limits lower extremity functionality. Achilles tendinopathy takes a long time to heal; over time there is thickening of the tendon and loss of elasticity. The pain is related to an alteration of the mechanical properties of tension and rigidity of the aponeurosis of the Achilles tendon.[31][32][33]
Evaluation
Physical exploration: Clinical signs and symptoms of Achilles tendinopathy include localized pain, focal or diffuse sensitivity, swelling, stiffness/morning pain, perceived rigidity in the Achilles tendon, positive arc sign, Royal London Hospital test, and Thompson test.
Tests used to diagnose Achilles tendinopathy:
- Lateral and axial calcaneus x-rays: May detect calcifications in the proximal extension of the tendon insertion or bony prominences in the upper portion of the calcaneus. Also, x-rays can help exclude pathological bone tumors.[34][35][36]
- Ultrasound: Can help assess injury to the tendon[37]; can be used to predict the risk of tendinopathy and rupture.[38] Ultrasound may reveal increased thickness of the Achilles tendon with hyperemia associated with hypervascularity, a decrease in the gastrocnemius-soleus rotation angle and a decrease in the length of the Kager fat pad. Ultrasound is also useful during interventional treatment.[39]
- Magnetic Resonance Imaging: Provides significant information about the state of joint structures with a study in multiple planes in static and dynamic views.[40][41] One study found that MRI had lower sensitivity than ultrasound in the detection of early changes of enthesopathy.[42]. Another study found an excellent agreement between tendon thickness measurement between magnetic resonance and ultrasound.[43]
Treatment / Management
Management of Achilles tendinopathy can divide into conservative and surgical. Additionally, one must consider whether it is an acute or chronic condition. Finally, for those with a full rupture, the treatment is usually surgical.
1. Conservative therapy: It is the first line of management and includes the following[49][50][51][52][53][54][55][56][57][58][59][60]:
- Reduction of activity levels
- Administration of non-steroidal anti-inflammatory drugs (NSAIDs)
- Adaptation of footwear, manual therapy directed at local sites may enhance the rehabilitation
- Eccentric stretching exercises should comprise an integral component of physiotherapy and can achieve a 40% reduction in pain; moderate level evidence favors eccentric exercise over concentric exercise for reducing pain
- Tendon loading exercise at short- and long-term follow-up
- If unresponsive to initial management, extracorporeal shock wave therapy reduces pain by 60%, with 80% patient satisfaction, improving functionality and quality of life, with a follow-up at 4 weeks; this might be the first choice because of its safety and effectiveness
- Physiotherapy improves the pain and functionality of the Achilles tendinopathy of the middle portion; however, studies do not show preferences for any particular exercise over another - overall, use of a splint to an eccentric exercise protocol or the use of orthoses to improve pain and function are not a recommendation
- Current evidence shows a lack of efficacy on the use of platelet-rich plasma for Achilles tendinopathy
2. Surgical therapy is optional for 10 to 30% of patients who fail conservative therapy after six months.[61][62] The success rate is higher than 70%, but reports show complication rates of 3 to 40%.[63] The Achilles tendon should undergo reattachment with a tendon rupture of more than 50%.[64]
Differential Diagnosis
Posterior heel and ankle pain is a frequent presentation in primary care, and the risk of developing pain is higher with increasing body mass index and age. Primarily, when patients do not improve despite the management established, further investigations are necessary.[65] The most common musculoskeletal disorders of the soft tissues related to ankle pain are[66][67]:
- Olecranon bursitis
- Plantar fasciitis
- Nerve entrapment or neuroma (pain accompanied by burning, tingling, or numbness)
- Heel pad syndrome (deep, bruise-like pain in the middle heel)
- Haglund deformity (prominence of the calcaneus that may lead to retrocalcaneal bursa inflammation)
- Sever disease (calcaneal apophysitis common in children and adolescents)
Erdheim-Chester disease (ECD) is a rare histiocytosis of non-Langerhans cells, reported in a 36-year-old male, with bilateral xanthogranulomas of the Achilles tendon. Although rare, ECD should be a consideration in the differential diagnosis of intratendinous masses.[68] As with all clinical presentations, the potential for non-musculoskeletal, more sinister causes of pain and systemic disease deserve scrutiny.[69]
Prognosis
Achilles tendinopathy has a better prognosis with early and adequate initial management. Surgical intervention for Achilles tendinosis of insertion (TAI) is successful in over 80% of cases. Stenson and his colleagues,[70] discovered that as the number of risk factors increased, the possibility of failure in non-operative treatment also increased. With the usage of the visual analog scale, limited range of motion of the ankle, prior injection of corticosteroids, and the presence of enthesophytes of the Achilles tendon, the probability of failure of the conservative treatment was 55%. Therefore, usage of the risk factors mentioned above can help the surgeon in the decision to perform surgery in the appropriate clinical setting. In a retrospective study of Sanalla and colleagues, they found that strengthening of the Achilles tendon with bone-tendon autograft was an effective procedure with a low risk of complications and reliable results.[71]
Complications
In a systematic review, Lohrer and colleagues,[72] concluded that the open and minimally invasive surgical treatment success rates did not differ (83.4%) and that there were no differences in patient satisfaction, but complication rates were lower for the minimally invasive procedures. Baltes and his colleagues classified the complications as follows[73]:
- Major complications: Such as ruptured AT, any reoperation, deep vein thrombosis, reflex dystrophy, persistent neuralgia, deep infections, major wound problems
- Minor complications Such as discomfort. Infections superficial, minor wound problems, scar sensitivity, hypertrophy, mild paraesthesia, prolonged hospitalization.
In another review, the surgical results were excellent or good in 89.6% of the cases and fair or poor in 10.4%. The average complication rate was 18.3%, with 15.7% minor complications and 2.6% major complications for surgical treatment of the Achilles tendinopathy insertion.[74]
Deterrence and Patient Education
Patient education and a more conservative approach can prevent chronic tendinopathy[75][76][77][78]:
- A change to another sport (swimming, weight training, rowing, cycling) allows the tendon to rest
- Eccentric exercise therapy (exercises that cause stretching combined with the contraction of a muscle) decreases pain and prevents chronicity
- Scientific evidence supports many conservative treatments, such as the use of non-steroidal anti-inflammatory drugs (e.g., ibuprofen, naproxen)
- The choice of running shoes that provide enough cushioning for the heel strike
- A warm-up exercise routine, and stretching the calf muscles before playing sports
- Gradually increasing the distance and running speed by only 10% per week, avoid running unhurriedly, running on slopes, and cooling properly after exercise
- Extracorporeal shock wave therapy may help
- Moreover, surgery is usually the last resort if recovery is prolonged
Enhancing Healthcare Team Outcomes
Achilles tendinopathy (AT) is a multi-factorial disease, which causes considerable morbidity by limiting exercise in athletes and non-athletes alike. The evidence recommends conservative or physical therapies as first-line treatment of AT; however, despite an increasing volume of research, there is still a lack of high-quality studies that test its effectiveness.[79][80] [Level I]
- Inspection and clinical examination supplemented by ultrasound and magnetic resonance imaging (MRI) are essential to achieving the correct diagnosis. A high interrelation between hypervascularization and tendinopathy of the Achilles tendon was found using Doppler ultrasound [Level 1], but these outcomes were not reproducible.[65]
- There is evidence to support the use of eccentric exercises by providing short-term benefits over brace for persistent Achilles tendinopathy.[56] [Level I]
- Soft tissue treatment plus eccentric exercise appears to be a beneficial treatment program that clinicians should recommend to patients with insertional AT.[54] [Level II]
- Surgery for insertional Achilles tendinopathy can lead to good functional outcomes and satisfactory return to sports when the tailoring of surgical care matches the degree of tendon involvement.[62][Level IV].
- Evidence for the effectiveness of traditional needle acupuncture may be beneficial for Achilles tendinopathy.[81] [Level I]
- Articles comparing minimally invasive techniques to open procedures reported on an average success rate of 83.6 % and 78.9% respectively (p = 0.987). The complication rate was 5.3 % with minimally invasive techniques and 10.5 % for open procedures.[72][Level II]
- In conclusion, endoscopic and minimally invasive procedures may prove to be the future of surgical treatment of middle Achilles tendinopathy.[73] [Level IV]
- There is no unequivocal evidence to advise any pharmacological treatment (comprising injection of a substance or local application) as the best advisable non-operative option for Achilles tendinopathy as an alternative to the most commonly used eccentric loading rehabilitation program. However, the combination of different medications administered with physical therapy may prove beneficial. There is a need for more long-term investigations.[82][Level I]
- Local infiltrations of autologous plasma,[83] [Level I] and the injection of platelet-rich plasma with eccentric training should be avoided, as there is no association between the therapeutic effects and the duration of symptoms in patients with chronic Achilles tendinopathy.[84][Level I]