Anatomy, Abdomen and Pelvis, Adductor Canal (Subsartorial, Hunter's Canal)
- Article Author:
- Allan Migirov
- Article Editor:
- Renato Vilella
- Updated:
- 9/13/2020 3:27:34 PM
- For CME on this topic:
- Anatomy, Abdomen and Pelvis, Adductor Canal (Subsartorial, Hunter's Canal) CME
- PubMed Link:
- Anatomy, Abdomen and Pelvis, Adductor Canal (Subsartorial, Hunter's Canal)
Introduction
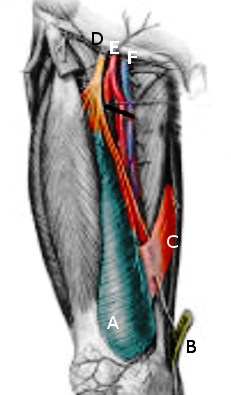
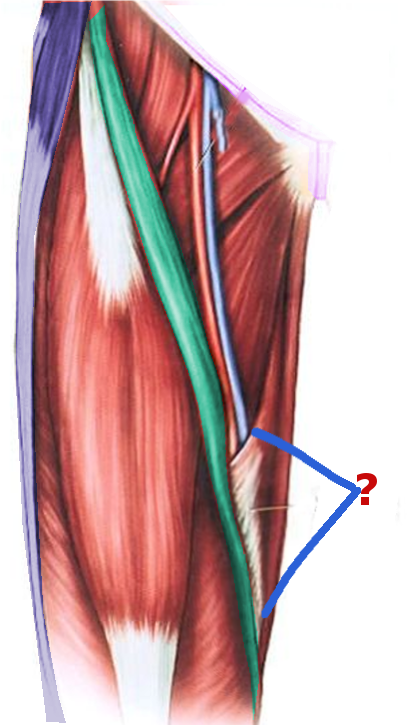
The adductor canal (AC), also known as the subsartorial or Hunter's canal, is a conical musculoaponeurotic tunnel passing through the distal portion of the middle third of the thigh. It functions as a passageway for several neurovascular structures from the femoral triangle to the adductor hiatus. The adductor canal has three borders. The vastus medialis muscle forms the anterolateral border, and the adductor longus and adductor magnus muscles form the posterolateral border. Medially, the adductor canal's border is an aponeurosis - the vastoadductor membrane, which is immediately deep to the sartorius muscle. Major structures passing through the canal include the superficial femoral artery, the femoral vein, and the saphenous nerve. Other structures, such as the nerve to vastus medialis and medial femoral cutaneous nerves, have previously been described to pass through the adductor canal, but their exact locations remain controversial. In addition to functioning as a key anatomical landmark, the adductor canal is clinically relevant. It can be a site of disease or suffer damage by trauma. It is also an increasingly-common site for the administration of regional anesthetic (nerve block) for knee, ankle, and foot surgeries.[1][2][3][4][5][6]
Structure and Function
The adductor canal is a space located distal to the midpoint of the anteromedial thigh that functions as a tunnel for several neurovascular structures. The average length of the canal is reportedly between 8.5 to 11.5 centimeters, depending on specific study and differences in sex.[1]
- Anatomical Location
- Proximal Border: The AC begins at the apex of the femoral triangle. This is the point where the medial border of the sartorius muscle crosses the medial border of the adductor longus muscle. Some sources cite the apex of the femoral triangle as the lateral border of the adductor longus muscle. However, the most recent consensus maintains that it is the medial border of the adductor longus muscle.
- Distal Border: The AC ends at the adductor hiatus, which is the largest of five fibrous openings within the adductor magnus muscle. As the superficial femoral artery passes distally through the adductor hiatus, it is renamed the popliteal artery.
- Anterolateral Border: Vastus medialis muscle
- Posterolateral Border: Adductor longus and adductor magnus muscles
- Medial Border: Vastoadductor membrane (VAM). This is also sometimes referred to as the “roof” of the AC. Superficial to the VAM is the sartorius muscle (see clarification below).[1][2][4][2][7]
- Clarification: True Adductor Canal vs. Subsartorial Space
- There is inconsistency among published sources, textbooks, and online resources regarding the roof/medial border of the AC. Some sources define the medial border as the sartorius muscle. The adductor canal is deep to the sartorius muscle, and the span of the sartorius muscle determines its limits. However, deep to the sartorius muscle is an aponeurosis called the vastoadductor membrane. The true adductor canal is roofed/bordered medially by the VAM. The space between the VAM and sartorius muscle is a plane called the subsartorial space or the subsartorial compartment. This naming can cause confusion as the adductor canal (Hunter’s canal) is sometimes called the subsartorial canal. However, the distinction is important because the true AC and the subsartorial space (superficial to the VAM) contain distinct groups of nerves.[7][8]
- Function
- The AC functions as a tunnel that transmits neurovascular structures from the femoral triangle in the proximal thigh to the popliteal fossa and maintains an anatomic continuity between the two compartments.[2]
- Surface Landmarks
- The adductor canal can be located using surface landmarks along with ultrasound. It was initially reported that the midpoint between the anterior superior iliac spine (ASIS) and the patellar base corresponds to the proximal end of the AC. However, this was disputed by several studies that demonstrated that the midpoint between the two landmarks actually localizes the femoral triangle. Rather, the adductor canal can be more reliably localized a few centimeters distal to the original midpoint location.[1][3][4][8]
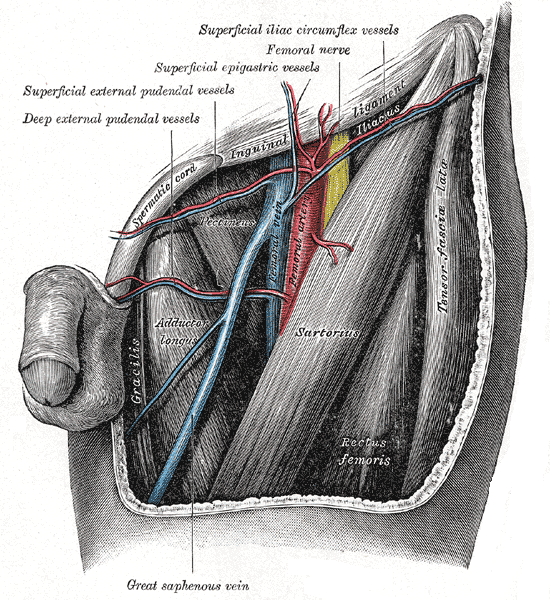
- Structure of Femoral Triangle (Scarpa’s triangle)
- Proximal border: inguinal ligament
- Lateral border: medial border of sartorius
- Medial border: medial border of adductor longus
- Floor: iliopsoas, pectineus, adductor longus, and possible adductor brevis muscles
- Apex: the intersection between the medial border of the sartorius muscle and the medial border of the adductor longus muscles[4]
Blood Supply and Lymphatics
Overview: The adductor canal houses the superficial femoral artery and the femoral vein.
The course of the Superficial Femoral Artery:
- Proximal to the adductor canal, the common femoral artery gives off a branch called the deep femoral artery (also called the deep artery of the thigh or the deep femoris artery) and continues distally as the superficial femoral artery. The superficial femoral artery travels from the femoral triangle (FT) into the adductor canal. From the adductor canal, as the superficial femoral artery passes distally through the adductor hiatus of the adductor magnus muscle, and is renamed the popliteal artery.[9]
The course of Femoral Vein:
- As the popliteal vein ascends through the adductor hiatus, it becomes the femoral vein. As the femoral vein continues to ascend, it receives multiple minor tributaries. It eventually joins with the deep femoral vein and the great saphenous vein to become the common femoral vein. As a clarification, some sources use the name “superficial femoral vein” instead of “femoral vein.” This name is a misnomer as the vein is not superficial but is a source of confusion as it runs along with the superficial femoral artery.[10]
Nerves
The saphenous nerve (SN) exits the femoral triangle at its apex and enters the adductor canal immediately lateral to the femoral artery. The saphenous nerve travels through the adductor canal until it diverges from the femoral artery distally. The saphenous nerve proceeds to exit between the sartorius and gracilis muscles.
The nerve to vastus medialis (NVM) has been previously described to travel within the adductor canal. However, other studies dispute this claim and report that the NVM travels through the subsartorial space, superficial to VAM, and deep to the sartorius muscle (see the section on clarification above). The subsartorial space also houses the subsartorial plexus, which is formed by contributions from three nerves: the medial cutaneous nerve of the thigh, the saphenous nerve, and the anterior branch of the obturator nerve.[2][7][8]
Muscles
Below is a summary of the major muscles that border the adductor canal. For further detail, please see the references for each respective muscle.
- Adductor Longus
- Origin: Anterior aspect of the pubic bone
- Insertion: Linea aspera of the femur
- Innervation: Obturator nerve
- Function: Adduction of the thigh [11]
- Adductor Magnus
- Origin: The muscle has two distinct portions with multiple origins, including the pubic ramus, the ischial ramus, and the ischial tuberosity.
- Insertion: Multiple including the gluteal tuberosity, linea aspera, supracondylar line of the femur, adductor tubercle of the femur, and other sites.
- Innervation: Obturator nerve and the tibial portion of the sciatic nerve
- Function: The adductor portion adducts and flexes the thigh; the hamstring portion adducts and extends the thigh. [12]
- Sartorius
- Origin: Anterior superior iliac spine (ASIS)
- Insertion: Superior medial aspect of the tibial shaft. Joins with the tendons of the gracilis and semitendinosus muscles to form the pes anserinus.
- Innervation: Femoral nerve
- Function: Hip flexion, external hip rotation, knee flexion [13]
- Vastus Medialis
- Origin: Inferior aspect of the intertrochanteric line as well as the medial aspect of the linea aspera of the femur
- Insertion: Medial border and base of the patella
- Innervation: Femoral nerve
- Function: Knee extension, stabilization of the patella [14]
Surgical Considerations
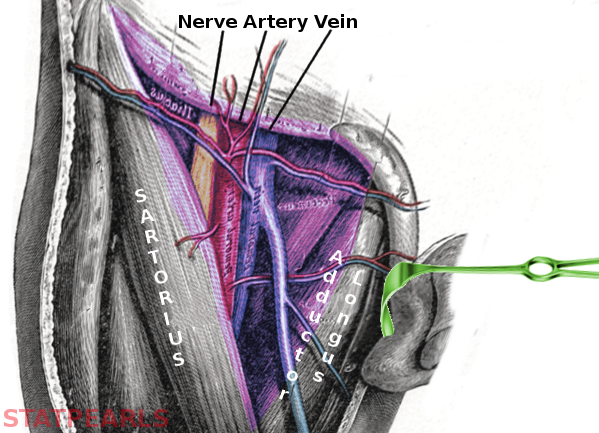
Adductor Canal Block
- Peripheral nerve blocks are becoming increasingly common in the management of postoperative pain. An ideal block provides adequate analgesia while maintaining motor function.
- An adductor canal block (ACB) involves the injection of local anesthetic into the adductor canal to provide analgesia for surgeries of the knee, ankle, and foot.
- The human knee receives innervation by two groups of sensory nerves: an anterior group and a posterior group. A properly performed ACB anesthetizes the anterior group of sensory nerves without affecting motor nerves and can be used in conjunction with another block to target the posterior nerve group. The sparing of motor nerves following knee surgery, such as total knee arthroplasty (TKA), accelerates postoperative ambulation, and likely improves recovery.
- Knowledge of the exact location of the adductor canal is crucial in performing a correct ACB; multiple studies demonstrated that “estimating” the location of the adductor canal often resulted in a femoral triangle block (FTB). An FTB is not motor-sparing because it often leads to weakness of the quadriceps muscles, which may be inferior to an ACB in some clinical situations.[2][3][7][8]
Clinical Significance
The structures passing through the adductor canal are susceptible to multiple pathologies.
- Peripheral Arterial Disease
- A common manifestation of atherosclerosis is peripheral arterial disease (PAD). PAD is defined as an obstruction to blood flow in the arteries (excluding cerebral and coronary vessels). The proximal popliteal and superficial femoral arteries are the most common sites of lower extremity atherosclerosis. Additionally, the superficial femoral artery is the second most common site of the femoral artery aneurysm (about 14% of cases).[6][15]
- Adductor Canal Compression Syndrome
- Adductor canal compression syndrome, ACS, is an extremely rare cause of arterial insufficiency of the lower extremity. It generally affects patients who are young, healthy, and physically active.The pathophysiology of ACS is non-atherosclerotic. Instead, it is caused by chronic and repeated compression of the superficial femoral artery as it passes through the adductor canal. Due to the sparsity of case reports, an exact cause of compression remains unidentified. Reports indicate that at least some cases are due to anomalous embryologic musculotendinous fibrous bands. They are thought to arise from the adductor magnus muscle and become symptomatic alongside hypertrophied adductor magnus or vastus medialis muscles. The treatment is surgical.[16]
- Venous Disease
- Isolated deep venous thrombosis (DVT) in the adductor canal is rare and is more likely to coexist with DVTs in other, more common locations.[17]
- One study hypothesized that femoral vein compression and/or venous valve dysfunction within the adductor canal might contribute to lower extremity venous stasis. However, no additional studies demonstrate this.[18]
(Click Image to Enlarge)