Ankle Fractures
- Article Author:
- Jessica Wire
- Article Editor:
- Valori Slane
- Updated:
- 8/11/2020 8:17:44 PM
- For CME on this topic:
- Ankle Fractures CME
- PubMed Link:
- Ankle Fractures
Introduction
The ankle joint is a highly complex joint. The ankle joint has multidirectional mobility for its complex role in supporting the weight of the body and fulfilling a myriad of daily functions. It is a combination of bones and ligaments structured around the talus. It includes the tibia, fibula, calcaneus, the tibiofibular ligament, the lateral ligament complex, and the medial ligament complex. The talocrural joint is the place where the distal tibia, distal fibula, and talus articulate. The tibia and fibula are anchored together via the syndesmosis. The syndesmosis consists of the interosseous membrane as well as the transverse, anterior, and posterior tibiofibular ligaments. There are both lateral and medial collateral ligament complexes which help to increase the stability of the ankle joint. The lateral collateral ligament forms from the fibulocalcanear ligament (FCL), the anterior fibulotalar ligament (AFTL), and the posterior fibulotalar ligament (PFTL). The medial collateral ligament consists of the deltoid ligament and the plantar calcaneonavicular ligament. The ankle joint moves in a unique way due to its structure. As the talus is asymmetric, the ankle is not purely a hinge joint. Instead, it acts as a rotary hinging movement. As many structures are involved in the ankle joint, in the context of an acute ankle fracture, it is easiest to think of it as a ring of structures situated around the talus. One break in the ring leads to a stable injury, while two or more breaks in the ring lead to an unstable injury.[1][2]
Etiology
Ankle fractures can be caused by excessive strain to the ankle joint as well as by blunt trauma.[3]
Epidemiology
Acute ankle fractures occur in 174 per 100000 adults per year. In those presenting to healthcare facilities with the chief complaint of ankle injury in the emergency department, 15% are attributable to ankle fractures. Medicare reports that 8.3 out of every 1000 Medicare recipients suffer from an ankle fracture each year. In the elderly, ankle fractures are the third most common osseous injury right behind the hip and distal radius fractures. In sports medicine clinics, ankle fractures account for approximately twenty percent of visits. With age, there is a bimodal distribution of ankle fractures which peaks in younger males and older females.[3][4][5][6]
Pathophysiology
There are various methods to classify ankle fractures.
Percival Pott described ankle fractures in terms of the number of malleoli involved (unimalleolar, bimalleolar, and trimalleolar).
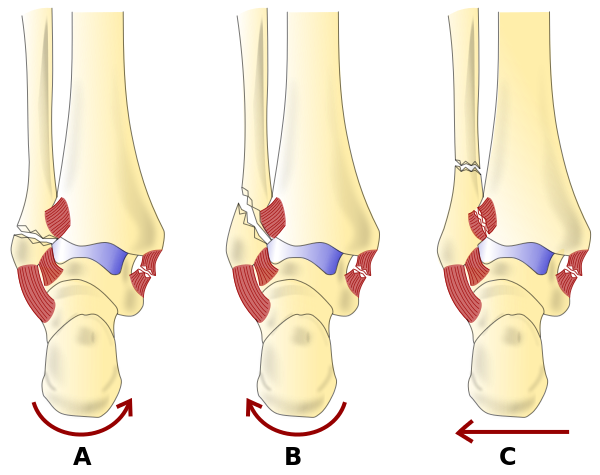
The Danis-Weber classification system categorizes ankle fractures by assessing the location of the distal fibula fracture in its relation to the syndesmosis.
A - Below syndesmosis
B - At the syndesmosis level
C - Above syndesmosis (i.e., Maisonneuve fracture)
Although this method describes the fracture relative to the syndesmosis, it does not accurately predict damage or injury to the syndesmosis. It also does not address damage to any medial ankle structure.
Type A is managed operatively with a closed repair. Type B & C require internal fixation.
The Lauge-Hansen classification system uses the mechanism of injury to determine the extent of injury to the ankle joint. By knowing the mechanism of injury or the deforming force, one can establish a sequence of injuries of the likely structures injured. Assessing the mechanism of injury can be valuable in deciding the appropriate treatment.
Supination-Adduction (SA)
- Distal fibula transverse fracture
- Medial malleolus vertical fracture
Supination-External Rotation (SER) - most common ankle injury (60% fractures)
- Anterior inferior tibiofibular ligament injury
- Spiral (or oblique) fracture of the distal fibula
- Posterior inferior tibiofibular ligament injury OR posterior malleolus avulsion
- Fracture of medial malleolus OR deltoid ligament injury
Pronation-External Rotation (PER)
- Fracture of medial malleolus OR deltoid ligament injury
- Anterior inferior tibiofibular ligament injury
- Spiral (or oblique) fracture of the fibula (aspect proximal to tibial plafond)
- Posterior inferior tibiofibular ligament injury OR posterior malleolus avulsion
Pronation-Abduction (PA)
- Fracture of medial malleolus OR deltoid ligament injury
- Anterior inferior tibiofibular ligament injury
- Comminuted or transverse fibular fracture (proximal to tibial plafond)
1st word (position of the foot during the time of injury)
- Pronation: Eversion, abduction, dorsiflexion; medial ligaments stretched and prone to injury
- Supination: Inversion, adduction, plantarflexion; lateral ligaments stretched and prone to injury
2nd word (movement of talus in ankle mortise relative to the tibia) Injuries always occur in a cumulative pattern; for example, a SER4 injury includes injuries of SER1, SER2, and SER3.
Pronation-dorsiflexion injuries are not classified in either the Danis-Weber or the Lauge-Hansen systems. Although uncommon, it is a unique mechanism in which injury results from axial loading. An example of this type of injury is a pilon fracture. In this type of injury, the sequence of events is as follows:
- Axial loading drives the talus into the tibia causing a medial malleolus fracture
- Another fracture occurs at the anterior tibial margin
- Supramalleolar fibular fracture
- Transverse fracture of the posterior tibia
Talar fractures often result from sudden hyperextension. Most often they are avulsion fractures on the anterior aspect of the talar neck. CT is the imaging of choice for these fractures. Talar fractures can also be due to pronation injury, plantar hyperflexion injury, or dorsiflexion injury.[1][3][7]
History and Physical
History is an integral part of any medical evaluation. In addition to the standard history (setting, chronology, location, quality, quantity, aggravating/alleviating factors, associated symptoms), it is important to ask specific questions targeted toward an ankle injury.
Questions include: Where is the pain? Is this an isolated injury or are there other injuries? Other injuries can be missed if there is a severely distracting injury such as an open ankle fracture-dislocation. Ankle fractures are usually the result of a twisting mechanism sustained as a result of a low-energy injury. Higher energy mechanism should raise the specter of compartment syndrome of the leg or a more grave injury such as a pilon fracture (axial loading). An ambulating patient is unlikely to have an unstable fracture. The ankle position at the time of injury and subsequent direction of force generally dictates the fracture pattern, as described by the Lauge-Hansen classification system. Past medical history can also be an important factor. Prior injuries/surgeries to the affected joint may affect the presentation. Comorbidities including diabetes, peripheral vascular disease, and smoking can complicate wound and fracture healing or increase risk of a Charcot neuroarthropathy. A patient's baseline/goals should be established through a social history including the patient’s level of mobility pre-injury, home situation, and regular activities as well as their future functional goals.
Physical Examination Always examine the contralateral un-injured ankle first, as it helps to establish a baseline ankle examination (what it looked like before injury). It is also vital to examine the tibia, fibula, knee, and foot as well. Some injury mechanisms can cause other injuries superior to the ankle (i.e., Maisonneuve fracture). Examine the ankle visually for swelling, pain, ecchymosis, and soft tissue injury, including abrasions and lacerations. Palpate the ankle to localize the point of injury. To ensure full examination, work methodically. Starting at the proximal tibia/fibula and working down. Once palpation is complete, perform examinations to assess neurological and vascular integrity. Assess for sensation, motor function, capillary refill, and pulses. It is important to test the passive and active range of motion, as well as weight-bearing status. It is imperative to assess and continue to monitor for signs of compartment syndrome.[3][2][8]
Evaluation
Ottawa Ankle Rules
Ankle radiographs should only be needed if there is pain or tenderness in either malleolus AND one of the following
- Tenderness of the bone at the posterior edge or tip (within 6 cm) of either the lateral or medial malleolus
- Patient unable to bear weight at the time of injury AND on arrival to the emergency department. Weight-bearing is determined by the patient's ability to take four steps.
It is important to recall that this set of rules were developed to reduce the number of unnecessary radiographs ordered. The reported sensitivity of the Ottawa ankle rules are close to 100%, but the specificity is highly variable across all studies; this is believed to be caused by user interpretation of the rules and provider dependent techniques in assessing tenderness on exam. Therefore, although effective, even the correct application of this rule does not 100% rule out an ankle fracture.
Radiological Features
Ankle x-ray: 3 view
- AP view: assess for soft tissue swelling that may lead to the discovery of other more subtle fractures
- Mortise view: taken with the foot in 15 degrees of internal rotation, evaluates talus positioning and syndesmosis widening
- lateral view: assess for anterior and/or posterior avulsion fractures assess for an effusion of ankle joint
If proximal leg tenderness is present or medial clear space widening with no obvious fibular fracture, radiographs of the tibia and fibula should be obtained to rule out the presence of a Maisonneuve injury. A Maisonneuve fracture is a proximal fibula spiral fracture with concomitant disruption of the distal fibular syndesmosis and interosseous membrane.
More complex axial imaging is rarely necessary; exceptions include triplane and pilon fractures.
Posterior malleolus fractures usually require a CT as the plain film underestimates the degree of impaction.
Weight-bearing radiographs not indicated in the acute ankle fracture in the emergency department, usually used for more stable injuries in outpatient settings
MRI although rarely emergently indicated is used to assess soft tissue, cartilaginous, or ligamentous injuries. It can also help to detect occult fractures.
Ultrasound can be used to assess for fractures as well a ligament and tendon injuries; however, results are user-dependent.[3][8]
Treatment / Management
Assess the injured patient according to ATLS guidelines with a systematic approach. Once the primary survey is complete and life-threatening injuries have been identified or ruled out, management of the ankle can begin. The first step is assessing the neurovascular status of the ankle. This step is necessary irrespective of the degree of deformity of the injured ankle. Skin integrity also requires assessment for any fracture or deformity that could be causing skin tenting. Skin tenting can lead to necrosis and delayed healing. If there is any clinical concern for vascular compromise or skin tenting, reduction to be attempted immediately to try to regain vascular flow and not cause further long term sequela. If there is no concern in the vascular status of the ankle, an X-ray can be obtained thus allowing the person reducing the fracture to visualize precisely where the fragments are which can aid reduction.
Reduce the ankle fracture as soon as possible once informed consent provided to the patient. Assess the neurovascular status of the limb before and after manipulation. Have splinting materials ready and measured out (use the uninjured, contralateral leg for measuring).
Ensure adequate analgesia for the patient including NSAIDs, IV medications, hematoma block, or procedural sedation. Once reduced and splinted in place, recheck neurovascular status, elevate the leg and obtain a post-reduction X-ray. If the fracture has not reduced, it will need re-manipulation. If despite best efforts in the emergency department (ED), there is still not acceptable fracture reduction, there may be soft tissue blocking reduction (such as the deltoid ligament). This status will require an urgent reduction in an OR and likely, ORIF / external fixation. If the fracture remains unreduced, there is a risk of vascular compromise, ischemia, articular damage and prolonged soft tissue swelling of the ankle all of which could result in chronic pain.
Stable fractures are those that are non-displaced. These fractures receive conservative treatment. Patients with stable fractures can be discharged with unrestricted weight-bearing as tolerated. These patients can receive a walking boot and be discharged with a plan for X-ray in 1 week if stability is uncertain. It is essential to provide extensive ED return precautions in the case of a change in the status of the injury. Return precautions should include but not be limited to: uncontrolled pain, numbness, tingling, increased swelling and decrease or change in their ability to bear weight.
Unstable fractures include those that are displaced, have talar shift, bimalleolar, and trimalleolar. These unstable fractures get treated with open reduction internal fixation (ORIF). If the patient has multiple comorbidities and is unable to tolerate surgical repair, there is the option for casting with 6 weeks of non-weight-bearing status. The ankle would need weekly ankle X-ray and the need for thromboprophylaxis needs to be assessed depending on other risk factors. This plan would require consultation with the orthopedic surgeon.[2][8]
Differential Diagnosis
- Rheumatoid arthritis
- Charcot joint
- Osteoid osteoma
- Ewing’s sarcoma
- Osteosarcoma
- Pathologic fracture
- Osteomyelitis
- Septic arthritis
- Osteoarthritis
- Gout
- Ankle sprain
- Achilles rupture
- Tendon dislocation
Prognosis
For patients with stable fractures that do not require operative repair, the prognosis is excellent. They can gradually bear weight and can be back at baseline as early as 6 to 8 weeks after the initial injury. In those with unstable fractures that undergo ORIF, although full weight-bearing can take place as early as 12 to 16 weeks, it may take up to 2 years until full final functional results. Prognosis is poorer for elderly patients, especially those with comorbidities. One-year mortality after the operative intervention is 12% in those older than 65 years old, increasing to a 50% 1-year mortality in those greater than 95 years old.[2][6][9]
Complications
Complications following ankle fractures can occur after both conservative nonoperative management and operative management.
Nonoperative management complications may include: compartment syndrome, dislocation, complex regional pain syndrome, limited range of motion, or inner pressure ulceration.
Operative management complications may include: compartment syndrome, wound hematoma, impaired wound healing, dislocation, mispositioned screws, inadequate reduction, complex regional pain syndrome, malunion, malposition, impingement syndrome, limited range of motion, or arthrosis.
Another complication of ankle fracture seen in people with diabetes is Charcot arthropathy which is also known as neuropathic arthropathy. This condition occurs when there is a progressive degeneration of the ankle joint, which leads to destruction of the bone, increased bone resorption, which ultimately leads to deformity. Long-term complications of this may lead to ulceration, infection, or eventual amputation.
Thromboprophylaxis is also essential in those with ankle fractures until full mobilization to prevent the development of DVT and pulmonary embolism.[2][10]
Deterrence and Patient Education
In patients with ankle fractures, education is vital. For those with stable fractures which do not require surgical management, it is essential to educate patients regarding appropriate follow-up, and it is crucial that they receive information regarding the expected course of healing so that they can return for re-assessment when necessary or if healing delays. In those with surgical management, the importance of physical therapy and weight-bearing goals need to be discussed before the patient leaving the hospital — red flags of delayed or inadequate healing need to be discussed with all patients.
Pearls and Other Issues
It is essential to perform a full physical exam and appropriate imaging to ensure identification of other associated fractures (e.g., Maisonneuve fracture)
- The associated soft tissue injury (puncture, laceration, abrasion) may be in a different location during evaluation than during the time of injury (due to swelling, less joint stress, etc.)
- Always assess the neurovascular status of the ankle before and after reduction and splinting
- There may be accessory ossicles in the joint due to anatomical variants that can be confused for an avulsion fracture in a trauma
- There are pre-dispositions to different fractures based on the activity performed at the time of injury[4][3][11]:
- Runners: posteromedial tibia, distal fibula, navicular
- Dancers: metatarsals, anterior tibia
- Jumping (i.e., basketball): anterior tibia, calcaneus
Enhancing Healthcare Team Outcomes
Management in the emergency department of patients presenting with ankle fractures is interprofessional. The team approach to the patient with an ankle fracture include the emergency physician, medical specialists, specialty-trained nurses, and respiratory therapy, especially if procedural sedation required for reduction. These team members need to communicate about the case to ensure optimal case management. [Level V] In those with unstable fractures requiring operative intervention, it is crucial to have timely contact with the orthopedic surgeon or podiatrist to improve patient outcomes. While in the hospital, physical therapists are essential in helping patients improve range of motion, strength and weight-bearing abilities. Upon discharge, it is also necessary to have open communications with case managers so that patients can be discharged to rehab centers or can heal safely at home by arranging equipment (walkers, canes, etc.), home nursing, and thromboprophylaxis prescriptions. Each medical team member is vital to the patient in each step of healing.
(Click Image to Enlarge)