Annular Disc Tear
- Article Author:
- Steven Tenny
- Article Editor:
- Christopher Gillis
- Updated:
- 8/10/2020 4:49:46 PM
- For CME on this topic:
- Annular Disc Tear CME
- PubMed Link:
- Annular Disc Tear
Introduction
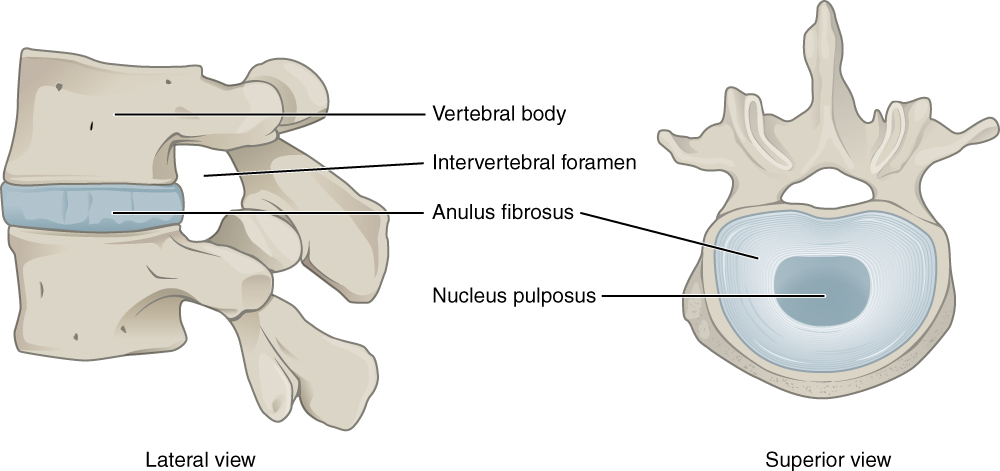
An annular fissure or tear is a deficiency of one or more layers of the annulus fibrosus.[1][2][3]
Most annular fissures are asymptomatic, but some may be painful. Typically, simple symptomatic annular fissures without disc herniation are treated with non-steroidal anti-inflammatory medications and low-impact physical therapy. Chronic pain due to annular fissures can be due to granulation tissue or in-growth of nerve endings which is usually seen near the dorsal root ganglion. Additionally, an annular fissure can allow extrusion, for example, disc herniation, of the nucleus pulposus and compress the adjacent nerves.
Etiology
The annulus fibrosus is the type I collagen surrounding the nucleus pulposus in approximately 15-20 layers. Together, the annulus fibrosis and nucleus pulposus form the intervertebral disc between adjacent vertebrae. The annulus fibrosus runs obliquely between edges of adjacent vertebrae, connecting the inferior endplate of the superior vertebra with the superior endplate of the inferior vertebra. The directions of the layers of the annulus fibrosus alternate which adds to the strength of the annulus fibrosus. Near the central region, the annulus fibrosus blends with the nucleus pulposus. The posterolateral aspect of the annulus fibrosus has a greater content of vertically oriented fibers leading to relative focal weakness at the posterolateral aspect. This anatomy of the annulus fibrosus explains why most annular fissures are at the posterior or posterolateral aspect of the annulus fibrosus.[4]
Epidemiology
Pathophysiology
The posterolateral aspect of the annulus fibrosus has a greater content of vertically oriented collagen fibers. In other regions of the annulus fibrosus layers are alternating obliquely oriented layers. Thus in the postero-lateral region, the vertical alignment of the fibers is more likely to allow for focal deficits of the annulus fibrosus and tearing or separation between the vertically oriented fibers.
History and Physical
Most annular fissures or annular tears are asymptomatic and discovered incidentally on imaging. If an annular fissure or tear is symptomatic, it may cause one of two findings: localized pain secondary to the tear or radicular symptoms secondary to irritation of the passing nerve root. The pain may either be acute if the tear occurs suddenly or more chronic if there is a slower development of the annular fissure.
If the annular fissure is locally symptomatic, it may cause pain localized deep pain worse with movements that can stress or irritate the focal annular tear. In such cases, there is no radicular nerve involvement, and the physical exam may be unrevealing. Sometimes the annular tear can irritate the traversing nerve and cause radiculopathy. If the annular fissure or annular tear is significant enough, disc material can herniate to irritate or compress traversing nerves or spinal cord. In either case, when the traversing nerve is irritated, it can cause radicular symptoms including pain, paresthesia, and/or weakness depending on the extent of nerve irritation or compromise.
Evaluation
An annular fissure can be concentric, transverse, or radial in orientation and may involve some or all layers. On magnetic resonance imaging (MRI) T2 sequence, the annular fissure is hyperintense (bright) compared to the rest of the annulus fibrosus (which is normally hypointense or dark) due to the relative increase in water content at the fissure compared to the normal annulus fibrosus.[7]
If there is herniation of intravertebral disc material, there must be incompetence of the annulus fibrosus, and thus, an annular fissure or annular tear must be present even if not specifically visualized on the imaging. Thus, an annular fissure or annular tear can be implicated any time intravertebral disc herniation is identified.
If a patient is unable to have an MRI, a computed tomogram (CT) myelogram may show nerve root or cord compression from a disc protrusion. The CT scan can not identify the edema of an annulus fibrosus tear or fissure and thus, it is less sensitive than MRI.
Treatment / Management
An annular fissure or tear can be symptomatic or asymptomatic. Symptomatic annular fissures can occur with or without intravertebral disc protrusion or herniation. Each entity is discussed separately below.[8][4]
Asymptomatic Annular Tear
If the annular tear or fissure is identified incidentally, most commonly on MRI imaging, then no treatment is warranted. Such annular fissures may resolve spontaneously over time and are frequently due to the stresses applied to the spine. It is posited that some asymptomatic annular tears may become symptomatic with time, but there is currently no definitive evidence that the treatment of asymptomatic annular tears provides any benefit or prevents any future issues.
Symptomatic Annular Tear without Disc Protrusion or Herniation
An annular fissure or tear can be symptomatic without disc protrusion or herniation. It is suspected that local inflammatory reactions from the annulus fibrosus tear or fissure lead to irritation of adjacent nerve fibers or traversing nerve roots. The mainstay of treatment for such situations is non-steroidal anti-inflammatory medications as well as low-impact physical therapy. The non-steroidal anti-inflammatory medications may help decrease the inflammatory reaction at the annular fissure which decreases stimulation or irritation of adjacent nerve fibers or traversing nerve roots. The low-impact physical therapy may help strengthen core muscles to mitigate the forces which may have originally led to the annular fissure or tear. Some have suggested local transforaminal steroid injections may alleviate the symptoms more quickly.
Some have argued that long-standing annular fissures or tears may lead to granulation tissue formation at the site of the annulus fibrosus tear or fissure. This local granulation tissue can either irritate or compress the traversing nerve root and lead to a radicular pattern of symptoms. The first-line treatment for such situations is non-steroidal anti-inflammatory medications and low impact physical therapy as discussed above with or without transforaminal steroid injection. In longer-standing cases or instances with weakness or progression some suggest decompression of the nerve with a foraminotomy may prevent further deterioration and improve the symptoms. Some have suggested resecting the granulation tissue itself.
Symptomatic Annular Tear with Disc Protrusion or Herniation
If there is disc protrusion or herniation, it is usually the protruding or herniated disc material itself which causes the clinical symptoms. In such cases, the patient is treated for the disc protrusion or herniation and not the annular fissure or tear. Treatment options for disc protrusion or herniation including conservative measures of nonsteroidal anti-inflammatory medications, physical therapy, and local injections. If symptoms fail to improve, symptoms progress or the patient develops weakness surgical treatment options should be considered including laminotomy, laminectomy, foraminotomy, discectomy, fusion, or some combination thereof. If a discectomy is performed there has been no convincing evidence that closure of the annular fissure, tear, or annulotomy significantly affects the long-term outcome for the patient.
Differential Diagnosis
- Diverticulitis
- Epidural and subdural infections
- Herpes zoster
- Mechanical back pain
- Nephrolithiasis
- Osteomyelitis in emergency medicine
- Pelvic fracture in emergency medicine
- Pelvic inflammatory disease
- Rheumatoid arthritis
- Sickle cell anemia
Prognosis
The natural history of mechanical back pain is benign and subsides on its own. Even with lumbar disc prolapse with no neurological deficits, the prognosis is good with conservative treatment in the midterm and long term.[9] If the patient has neurological deficits, it would be better to resort to surgical management.
Complications
The disc bulge can cause:
- Cauda equina syndrome
- Conus medullaris syndrome
- Deep vein thrombosis, bedsore, atelectasis, and urinary infection - if the patient is bedridden due to paralysis
- Motor neurological deficits
- Sensory neurological deficits
Deterrence and Patient Education
The patients should be instructed to:
- Consume medicines as instructed
- Restrict physical activities as advised
- Avoid activities involving excessive movements of the spine.
Enhancing Healthcare Team Outcomes
Annular tears are quite common and often associated with low back pain. The diagnosis of annular tear and its correlation to symptoms is not always easy. Many patients with mild annular tears have no symptoms and there are others who present with excruciating low back pain, but with minimal evidence of an annular tear. Thus, a thorough neurological exam is key. The decision to obtain imaging studies depends on the severity of symptoms. However, the treatment of annular tears also requires good clinical judgment. A number of patients do improve with conservative treatment like weight loss, regular exercise, discontinuation of smoking, adopting proper lifting techniques, using safety equipment at work and during sports, and avoiding a sedentary lifestyle.[10][5] The orthopedic nurse should assist in patient and family education in lifestyle changes that will minimize further tears and allow healing. The pharmacist may need to provide guidance in regard to pain management. The interprofessional team should work together to educate the patient and provide guidance that will assist with healing and improve outcomes. [Leve V]
(Click Image to Enlarge)