Asbestosis
- Article Author:
- Jenish Bhandari
- Article Author:
- Pawan Thada
- Article Editor:
- Yub Raj Sedhai
- Updated:
- 10/16/2020 5:34:30 AM
- For CME on this topic:
- Asbestosis CME
- PubMed Link:
- Asbestosis
Introduction
Asbestosis is an interstitial lung disease caused by inhalation of asbestos fibers. These fibers are different mineral silicates (mainly hydrated magnesium silicates) and are classified into two main categories based on their shape i.e., serpentine and amphibole.[1] Serpentine fibers include chrysolites that are curly and flexible and are less pathogenic than amphibole fibers. Chrysolite being more flexible, curvy, and more soluble settles in the upper part of the respiratory tract. The mucociliary function is more prominent in the upper respiratory tract, so chrysolite fibers are easily removed. Amphiboles (crocidolite, amosite, tremolite, and anthophyllite) are straight, stiff, more brittle fibers. They are more toxic than serpentine fibers as they are less soluble and straight, and they usually align along the airstream and reach deeper into the lungs and the interstitium by penetrating the epithelium. Asbestos fibers have been historically chosen for construction, shipping, mining, and aerospace engineering commercial use because of its high electrical and thermal resistance and low-cost.
Etiology
There are three main forms of asbestos exposure. Direct work-related environmental exposure is common among workers at shipyard, mining, aerospace, etc. Bystander exposure is the second form of exposure commonly seen in certain professionals like electricians, mason, and painters. The third and the most common form of asbestos exposure is the general community exposure, such as the use of asbestos road surface, playground material, landfills, and chemical paints. The disease is dose depended; the dose of exposure is higher in the first group and respectively lower in the second and third forms of exposure. Also, the risk of the disease is more with amphibole variety compared to the serpentine asbestosis fibers.
Epidemiology
The prevalence of the disease is more in those disciplines where the intensity of exposure is high. A study conducted in Okayama, Japan among construction workers revealed that workers working in the installation of the asbestos board have the highest number of cases (39.1%) followed by sprayer of asbestosis (38.5%). And also longer the duration of exposure, more the chances of asbestosis.[2] In the UK, insulation workers have the highest risk of Asbestosis followed by asbestos stripping.[3] It is estimated that asbestos causes around 55000 deaths per yr in the world.[4] More prevalent in construction workers.[3]
The latent period for benign disease is shorter than other pulmonary complications. The incidence of pleural effusion is associated with the site of exposure and was found to be 9 cases per 1000 in heavily exposed groups. Although mesothelioma is less prevalent than lung cancer, over 2000 cases per yr in the twenty-first century were reported in the united states of America.
The incidence of lung cancer is comparatively more than mesothelioma. The use of asbestos in developed countries has reduced but use in developing countries like Nepal, Pakistan has considerably high.
Pathophysiology
Interstitial fibrosis is regarded as the principal pathogenic mechanism of asbestosis. It is believed that after deposition and transmigration of asbestos fibers in the lung, there is an accumulation of macrophages followed by fibroblasts that lay the foundation for fibrosis. Reactive oxygen species produced by immune cells and phagocytes in response to asbestos fibers result in oxidative injury. These reactive oxygen species and transepithelial migration of fibers injure the type I alveolar cells. Injured epithelial cells also produce fibroblast growth factor-beta, which induces fibrosis. Macrophages, in an attempt to phagocytose the foreign body, produce inflammatory mediators such as tissue necrosis factors, interleukins, and stimulation of phospholipase C pathway.[5][6] These mediators have a key role in stimulating the other cells like lymphocytes, myofibroblasts. This leads to the proliferation of fibroblasts and an increase in the number of cells in the matrix by about 2-fold. Macrophages also produce fibroblast growth factors, platelet-derived growth factor, and insulin-like growth factors that cause fibrosis. Plasminogen activator produced by macrophages degrades the matrix glycoproteins, which further damages the interstitium.
As this is a progressive disease, fibrosis increase over time. Asbestos fibers also activate serum complement C5a, a chemotactic factor for macrophages.[7] In most cases, asbestos fibers coated by other toxins, including transition metals, induce the formation of reactive oxygen species. In one cell-free system, iron-coated on these fibers has a role in the production of hydroxyl ion, causing free radicle injury.[6]
A recent investigation revealed that the length of fibers has a direct relation with pathogenesis. Longer fibers are more potent than shorter fibers in the stimulation of the NF-kB pathway and gene promoter activity.[5] Exposure to amphibole is linked to autoantibodies production. It is believed that patients with positive antinuclear antibodies test have more chances of developing interstitial and pleural abnormalities.[8] In addition to cellular and fibrotic reactions, asbestos possibly functions both a tumor initiator and promoter. Amphibole type has more tendency for carcinogenesis of pleura. The severity of asbestos-related pulmonary fibrosis is related to the total dose of exposure.
Histopathology
On gross examination, visceral pleura is markedly thickened, especially on the lateral and diaphragmatic surface of the lung with localized fibrous plaques and pleural effusions. Diffuse fibrosis of the lower lobe of the lung is visible on the cut section.On microscopic examination, asbestosis is marked by interstitial fibrosis with the presence of characteristic asbestos bodies and ferruginous bodies. The presence of both asbestos bodies and ferruginous bodies help pathologists differentiate between asbestosis and interstitial lung fibrosis. Asbestos bodies are golden yellow, beaded rod-like structures with the translucent center. It formed when asbestos fibers get coated with iron-containing proteinaceous material. A ferruginous body is an indication that the patient may have had prior exposure to asbestos and appear as golden-brown fusiform rods resembling dumbells. Fibrosis causes distortion of the lung parenchyma architecture, which causes the formation of enlarged air space surrounded by a thick fibrous wall and hyperplastic type II pneumocytes called honeycomb appearance.
History and Physical
The history of occupation is crucial for both diagnosis and management approach. History of exposure to asbestosis helps to exclude other chronic interstitial lung diseases. Usually, there is a history of 10 to 20 years of exposure to asbestos and progressively worsening dyspnea. Cough with sputum and wheezing are unusual, though, if present are mainly associated with smoking. The patient may complain of chest discomfort due to heart failure following pulmonary hypertension. Duration and intensity of exposure whether the patient has direct occupational contact with asbestosis. History of smoking and dyspnea on exertion are important, and nonproductive cough is quite common. History of loss of appetite and weight, hemoptysis indicates the suspicion of lung tumors. Gradual onset of localized pain or breathlessness and then radiating to the shoulder may be evident in pleural involvement.[9]
Physical examination reveals clubbing in 32% to 42%, asbestos warts, reduced chest expansion due to restrictive lung disease (38%). Bibasilar rales are best auscultated at lower lateral and basal areas.[9][10] In advanced disease, the patient may show signs of cor pulmonale such as pedal edema, jugular venous distension, right ventricular heave, hepatojugular reflux, cyanosis. These signs are mainly due to right-sided heart failure from pulmonary vascular remodeling.
Evaluation
The diagnosis of asbestosis is largely clinical. First, the history of asbestos exposure is central to the diagnosis. The overall clinical picture is characterized by progressive restrictive pulmonary disease with interstitial fibrosis on radiography. The pulmonary function test reveals characteristic restrictive disease.[3]
Pulmonary Function Tests
Spirometry and Lung Volumes
This includes forced vital capacity (FVC), forced expiratory volume in 1 sec (FEV1), total lung capacity (TLC), functional residual capacity, and residual volume. Like any other restrictive lung disease, all earlier mentioned lung volumes are reduced.FEV1/FVC ratio is either normal or increased.
Diffusing Capacity
Total carbon monoxide diffusion capacity (DLCO) reduction is a common but nonspecific finding. Reduced total carbon monoxide diffusion capacity (DLCO) is manifested earlier.[11] This is due to the mismatching of ventilation and perfusion (V/Q).
Arterial Blood Gas
Arterial oxygen tension (pao2) may be normal or may reveal hypoxia and respiratory alkalosis.[12] Carbon dioxide retention is rare; if present indicates the end-stage disease, and there may also be evidence of airflow obstruction due to small airway dysfunction. Nevertheless, it is important to note that asbestosis is a diagnosis of exclusion, and it is clinically relevant to differentiate asbestosis from idiopathic pulmonary fibrosis because both essentially have many similar presenting symptoms. Both asbestosis and IPF are characterized by progressive interstitial pulmonary fibrosis, with a restrictive lung disease picture in PFT. There are orally subtle differences between the two radiographically and histologically. It is important to differentiate between the two because there are distinctly targeted therapies available, although not that effective.
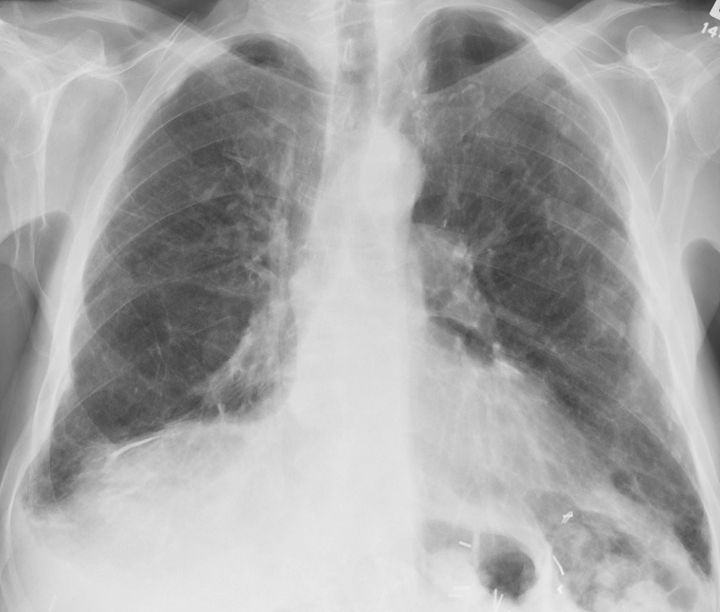
Plain X-ray of the Chest
It shows interstitial fibrosis. High-resolution computed tomography (HRCT) is often diagnostic of asbestosis.[13] HRCT shows ground-glass opacities, along with diffuse interstitial fibrosis in asbestosis whereas, in idiopathic pulmonary fibrosis, there is evidence of patches of opacities. Pleural thickening and calcified pleural plaques in tomography is the hallmark of the disease. Asbestosis mimics idiopathic pulmonary fibrosis radiographically, especially in CT. An important distinguishing point is that asbestosis begins more centrally and dissipates peripherally following a centrifugal pattern. In contrast, idiopathic pulmonary fibrosis begins peripherally, especially at the bases, and progresses centrally and upwards as the disease progresses. At least theoretically, IPF follows a centripetal pattern. Differentiating asbestosis and idiopathic pulmonary fibrosis (IPF) on CT can be challenging, and histopathology can be conclusive.
Lung Biopsy
It shows interstitial fibrosis with characteristically peribronchial fibrosis. The distribution of fibrosis in asbestos disease is from the center to periphery, i.e., centrifugally. The microscopic view of asbestosis shows distinct Asbestos bodies coated with iron-containing proteinaceous material and diffuse pulmonary interstitial fibrosis, but in contrast, idiopathic pulmonary fibrosis (IPF) displays patchy interstitial fibrosis. The profuse proliferation of fibroblasts, i.e., fibroblastic foci and subsistence of both early and late proliferative lesions (temporal heterogeneity), are well defined in IPF and rare or absent in asbestosis.
A lung biopsy can be achieved by endobronchial, transbronchial, and video-assisted thoracoscopic (VAT) approaches. The endobronchial biopsy is done with ultrasound-guided bronchoscopy to visualize the airway and adjacent structures. This technique has been routinely used in many centers due to its high diagnostic value and low risk. Endoscopically-guided forceps do Transbronchial lung biopsy. Conventional transbronchial biopsy has a higher risk of complications and bleeding. The modern technique is the minimally invasive video-assisted thoracoscopic (VAT) guided biopsy. VAT has fewer complications, is more sensitive, specific, and has more diagnostic yield than transbronchial biopsy. So, VAT is preferred over transbronchial lung biopsy, though VAT has some discrepancies like cost and expertise requirement.[14]
Bronchoalveolar lavage has a limited role. Samples can be taken from suspected patients for cellular analysis of asbestos bodies count, inflammatory cells like macrophages, neutrophils, eosinophils, and dust particles. Asbestos body formation is more common in amphibole fibers, while chrysotile fibers have a shorter half-life and have fewer chances of asbestos body formation. So the absence of asbestos bodies in chrysotile asbestosis leads to a false-negative result.[15]
Lab analysis shows elevated C-reactive protein, erythrocyte sedimentation rate, rheumatoid factor, and antinuclear antibodies.
Treatment / Management
Asbestosis has no specific treatment, so supportive care is the only available option. Therefore, prevention is the best management. Monitoring of the occupational environment and minimizing asbestos exposure has a significant role in asbestosis control.
Drug Therapy
The goal of corticosteroid therapy is to suppress the acute and chronic inflammatory process, thereby further reducing lung damage, but the success rate is low. Steroids suppress the release of reactive species and mediators in the ongoing inflammatory process. Because of the lack of placebo-controlled trials, there is no direct evidence of the benefits of steroids in improving the survival of life. The proper dose and length of therapy of steroids are not known.[16] High dose corticosteroid and other immunosuppressive drugs such as azathioprine have some roles in reducing exacerbation of acute asbestosis. The starting dose of prednisolone is usually considered 0.5 to 1 mg per kg in a once-daily oral dose for 4 to 12 weeks. The patient is monitored and reevaluated. The dose is tapered to 0.25 to 0.5 mg/kg for further 4 to 12 weeks if the patient is stable and improving. But some studies show that the use of agents like cyclophosphamide accelerates the fibrotic process, so its use is limited. If the condition is not improving and the patient is unstable, then either other drugs are added, or steroid is withdrawn. Colchicine is found to be a mild antifibrotic agent.[17] Antibiotics therapy should be prompt for superimposed respiratory infections as well as immunization against pneumococcus and Haemophilus influenza.
Oxygenation
Patients with hypoxemia (Pao2< 55 mmHg) at rest or with exertion should be supplemented with oxygen. Pulmonary rehabilitation and management of cor pulmonale have shown to improve the quality of life as the disease progresses.
Surgery
Decortication of subpleural fibrosis by thoracotomy improves the atelectasis. Pleurectomy can be performed in pleural fibrosis.[18] But if the collection of pleural fluid is rapid, then only palliative removal of fluids to relieve breathlessness should be done.[9]
Lung Transplantation
This is the ultimate treatment in severe asbestosis, where all other therapies have failed in case of chronic and irreversible fibrosis.
Differential Diagnosis
Differentials of asbestosis include the diseases involving interstitium of lung parenchyma such as idiopathic pulmonary fibrosis, interstitial pneumonitis, rheumatoid arthritis, hypersensitive pneumonitis, pleuropulmonary fibroelastosis, drug-induced pneumonitis, combined pulmonary fibrosis, and emphysema. Diagnosis of asbestosis requires the exclusion of these differentials.
Non-specific Interstitial Pneumonitis
This may be idiopathic or associated with secondary to other connective tissue disorders. Lower lobe involvement, ground-glass opacities, impairment of pulmonary functions mimic this condition with asbestosis, but female predominance and rare honeycombing help in differentiation. History of exposure and histopathology is important to rule out other similar conditions.[19]
Chronic Hypersensitivity Pneumonitis
It is an allergic reaction based upon the antigen-antibody interaction following exposure of allergens. Clinical presentation of hypersensitive pneumonitis such as dyspnea, cough resembles with that of asbestosis. So lung biopsy with histopathology evaluation is required. It involves interstitial inflammation with granulomas and giant cells, usually throughout the whole lung, as compared to more pronounced fibrosis in lower lobes of the lung in asbestosis.[20]
Rheumatic Disease
Rheumatic disease involves the interstitium of the lung in about 10% of cases. Unlike asbestosis, other systemic manifestations like arthritis, Raynaud phenomenon, muscle weakness, skin changes are present in rheumatic disease.[21]
Drug-induced Interstitial Pneumonitis
Some drugs used for purposes other than pulmonary diseases have pulmonary toxicity involving interstitium as their side effects. Anagrelide [22], a phospholipase A2 inhibitor, lamotrigine [23], cyclophosphamide [24], bleomycin [25], nitrofurantoin, etc are the drugs which cause pulmonary toxicity. This interstitial lung toxicity may confuse with asbestosis, but history of drug intake helps to distinguish the real cause of disease.
Pleuropulmonary Fibroelastosis
Pleuropulmonary fibroelastosis is a rare benign condition. Though this disease simulates the asbestosis, this condition involves fibrosis of pleura, and subpleural parenchyma almost simultaneously is the characteristic feature. Fibrosis is due to elastic fiber proliferation. But in asbestosis, pleural involvement is not parallel to parenchymal fibrosis as pleural involvement is usually the late presentation. And also, pleuropulmonary fibroelastosis may involve the upper lobe of the lungs.[26]
Silicosis
Silicosis has more tendency to undergo fibrosis than asbestosis, forming a whorled pattern of collagen fibers that can be appreciated in histology. Occupation history makes an easy way out to exclude silicosis. Fibrosis may also involve hilar lymph nodes and sometimes the calcification called egg-shell calcification.[27]
Sarcoidosis
Sarcoidosis is a chronic granulomatous disease of the lung which involves the multisystem. CD4+ to CD8+ cells ratio is increased as in asbestosis, but it has a more pronounced increment than in asbestosis. Histopathology reveals noncaseating granuloma, asteroid bodes, Schaumann bodies are characteristic of sarcoidosis not found in asbestosis.[28]
Coal Workers' Pneumoconiosis (CWP)
It is also called black lung disease is the coal dust induced progressive massive fibrosis disease. Cut section and biopsy of the lung of workers working in coal mines show black patches mixed with fibrosis.[29]
Combined Pulmonary Fibrosis and Emphysema: Usually, emphysema is highly associated with smoking and occurs without fibrosis. The co-existence of fibrosis and emphysema was first established in 1990.[30] Upper lobe emphysema and lower lobe fibrosis are seen in some male smokers.
Prognosis
The severity of the disease depends upon the duration and intensity of exposure. More intense contact for a long period of time has a poor prognosis. Early intervention is an immediate effect after the first symptoms have good outcomes and prolong survival. The condition worsens in acute exacerbations and in superimposed infections. Radiologic screening in workers helps in picking the earliest abnormal changes. [31] Steroids have only symptomatic treatment. So outcomes after steroid therapy do not always favor the alleviation of disease. Progression of the disease process can be stopped by removing the offenders. In later stages, the disease process becomes irreversible and may finally end with lung cancer. Patients with pleural involvement rarely survive more than a year after diagnosis has been made. But survival from first symptoms or earliest screening is a maximum of 4 years.[32] Radical surgery or radiotherapy of mesothelioma may aid in the extension of tumors to the chest wall.
Complications
Complications increases with the duration of exposure.
Respiratory Gailure
Asbestosis is a restrictive lung disease characterized by the restricted filling of the lung. Fibrosis of interstitium causes impairment of filling due to dysfunction of bronchioles mainly on lower lobes of lungs. Total lung capacity, forced vital capacity are reduced significantly. Patients complain of progressive dyspnea on exertion and cough. Deterioration of diffusing capacity, oxygenation is common. Pleural fibrosis prevents the expansion of the lung. Carbon dioxide retention is another hazard that leads to pulmonary acidosis, and either death or if survived is adversely disabled.[18] In many cases, benign pleural effusion occurs early, followed by pleural plaques formation. Effusion is generally bilateral and exudative and mostly remains asymptomatic. Lung collapses, resulting in atelectasis so that pulmonary insufficiency worsens. Fibrosis causes the derangement of the pulmonary vascular system, especially capillaries, which causes pulmonary hypertension. The decrease in diffusing capacity has a direct impact on hypoxemia.
Malignancy
Patients with asbestosis have a high risk of developing pleural malignancy. Patients who have low exposure of asbestos fibers have sequelae of asbestosis followed by malignancy, but those with intermediate or high-intensity exposure have high chances of lung cancer even in the absence of asbestosis. Lung cancer has more propensity when the smoker is exposed to asbestos due to the additive effect of each other. Studies show that adenocarcinoma(primary bronchogenic carcinoma) is the major type that accounts for about 45%, followed by squamous cell carcinoma, about 42%, and the rest of the tumor is undifferentiated (13%). Unlike fibrosis, the majority of tumors present in upper lobes (69%) and only 13% in lower lobes[33]. Mesothelioma of pleura and peritoneum is common but is less prevalent than parenchymal lung cancer. In contrast, to bronchogenic carcinoma, the risk of mesothelioma does not increase with smoking in patients with asbestosis. Epidemiologic studies have explored that greater than 80% of mesothelioma is due to asbestos exposure. Pleural angiosarcoma is a rare endothelial sarcoma highly aggressive malignancy whose clinical and radiological presentation mimics the mesothelioma. Immunohistological stains are diagnostic to pleural angiosarcoma helps to differentiate it from mesothelioma.[34]
Heart and Other Organs
It was found that heart weight is increased due to hypertrophy of right ventricle pumping against high pulmonary vascular resistance. More commonly, left auricle hypertrophy has been appreciated. Pulmonary and tricuspid valves are generally normal, but the mitral valve is fibrosed and fused with thickening chordae tendineae. The liver is congested in the centrilobular pattern due to the right-sided damming of blood.[35]
Cancers of Other Organs
Cohort's study has unveiled that asbestosis is related to cancers of the gastrointestinal tract, ovary, adrenals, larynx, and kidney. Gastrointestinal tract cancer is mainly due to exposure to asbestosis through asbestos-lined cement water pipes.[36]
Deterrence and Patient Education
Asbestosis is an occupational disease, so prevalent more in workers. Prevention is the utmost step in the management of asbestosis. Despite the usefulness of asbestos, it is hazardous for long term use and exposure. In the modern world, concern over the harmful effects is rising continuously. Research has been conducted to evaluate the effects of asbestos on health. Because it takes a long time to develop the disease as it is a progressive process, cessation of exposure stops the disease process. Avoiding potential risks, health education and safety training, monitoring of the working environment, periodic examination, and providing them treatment help to control the disease. Workers should be alarmed and have the right to know about the symptoms, outcomes of treatment, the toxicity of drugs, health problems of asbestosis, should consult the health team as soon as possible. They can choose the investigation and treatment modality after consulting doctors. Patients have responsibilities to fulfill something that they can do their own like cessation of smoking, minimizing the exposure, changing the workplace or occupation, self-care, being compliant with medications and instructions.
Enhancing Healthcare Team Outcomes
Competent healthcare systems in collaborations with other organizations and government bodies should work together to control the occupational diseases. The healthcare team has more diagnostic, therapeutic, and supportive care. So prevention or minimization of exposure necessitates the government legislation to act accordingly, international labor organizations, world health organization, dust management teams. Intersectoral coordination has a huge impact on optimizing the working environment and working hours. The application of engineering techniques to maintain appropriate working sites for optimum workers' health is essential. Healthcare disciplines consist of physicians, radiologists, pulmonologists, pharmacists, surgeons, oncologists, nurses, and histopathologists together assist in making consensus diagnosis and treatment.[19] Proper diagnosis with the help of multi-disciplinary healthcare teams helps to devise the right way to the correct treatment. Nursing care during the treatment has its importance in the healthcare system. Complications of asbestosis require multimodality treatment options such as oncologists to treat lung cancer, surgeons for decortication and pleurectomy, etc.