Aspergillosis
- Article Author:
- Michaelia Fosses Vuong
- Article Editor:
- James Waymack
- Updated:
- 8/10/2020 9:04:57 PM
- For CME on this topic:
- Aspergillosis CME
- PubMed Link:
- Aspergillosis
Introduction
Aspergillus is a fungus found throughout the world that can cause infection in primarily immunocompromised hosts and individuals with the underlying pulmonary disease. Many different species of Aspergillus can cause infection. There are three major types of bronchopulmonary Aspergillus infections: invasive aspergillosis, chronic aspergillosis, and allergic aspergillosis. Aspergillosis infection can also manifest as sinus disease in immunocompromised hosts. If left untreated, invasive aspergillosis can have mortality approaching 100%. In cases of suspected invasive aspergillosis, an extensive diagnostic workup is necessary, but treatment should be initiated early to reduce morbidity and mortality.[1][2][3]
Etiology
The primary route of infection is through the respiratory tract. Aspergillus, however, can infect other tissues such as skin, sinuses, central nervous system, eyes, nails or become disseminated throughout the body. Of the many species of Aspergillus, the most common to infect humans is Aspergillus fumigatus. When sinus involvement occurs, Aspergillus flavus is more likely to be the offending organism. Sometimes it is difficult to identify the exact species, and the organism will be identified only as Aspergillus species.[4][5]
Epidemiology
While Aspergillus species are common, invasive aspergillosis is common only in the immunocompromised population, composed of patients with AIDS, neutropenic patients, those on long-term corticosteroids, and recipients of transplants on anti-rejection medications. The incidence of aspergillosis in patients undergoing bone marrow transplantation can be as high as 10% to 20%. Invasive aspergillosis is also be seen in the critically ill intensive care patient with an underlying pulmonary disease such as chronic obstructive pulmonary disease (COPD) or asthma. Overall, the incidence of invasive aspergillosis has risen four-fold in the last 13 years. Patients with underlying lung diseases such as chronic obstructive lung disease, tuberculosis, asthma, lung cancer, and sarcoidosis are also at higher risk for developing the chronic form of aspergillosis. Allergic bronchopulmonary aspergillosis is almost exclusively found in asthma and cystic fibrosis patients. Those working in the construction and farming industries may be at increased risk of Aspergillus infection due to chronic exposure in their work environments. Smoking marijuana contaminated with the fungus may also place an individual at risk for infection. Nosocomial Aspergillus infections have been reported from hospital showers and healthcare facilities undergoing construction.[6]
Pathophysiology
In an otherwise immunocompetent person, Aspergillus conidia are inhaled and taken up by phagocytes in the lungs. The conidia germinate into hyphae at body temperature. In immunocompetent hosts, phagocytes secrete mediators such as beta-D-glucan which activate neutrophils. Neutrophils kill the invasive hyphae, and the Aspergillus infection is kept at bay. If any of these mechanisms are impaired in an immunocompromised patient, the infection may be allowed to spread.[7]
Histopathology
Biopsy specimens can be observed with acute angle hyphae (45 degrees) using Gomori methenamine silver or periodic acid-Schiff staining.
History and Physical
A thorough history and physical exam should be done in every patient suspected of having an aspergillus infection. Care should be taken to understand a patient’s risk factors for invasive diseases, such as immunocompromised status. The clinician should investigate in depth current and past treatment and comorbidities to best assess the potential for an immunocompromised state.
The invasive aspergillosis patient will often be a critically ill person with immunocompromised status. This condition should also be considered in an already critically ill patient with underlying lung disease. Most common initial symptoms include dyspnea, increased sputum production, chills, headache, and arthralgias. As the condition quickly progresses, fever, toxicity and weight loss manifest. On examination, there may be sinus tenderness, nasal discharge, rales, dermatologic changes, or meningeal signs of the central nervous system.
Chronic pulmonary aspergillosis will present most commonly with chest pain, weight loss, cough, hemoptysis, shortness of breath, and fatigue. Allergic aspergillosis will present with recurrent exacerbations of asthma with the most prominent finding being dyspnea and wheezing along with coughing up large amounts of sputum with brown plugs.
Evaluation
A strong clinical suspicion to identify patients at risk for invasive aspergillosis is the first step in evaluating for aspergillosis since aspergillosis conidia are constantly inhaled. The fungal stain of the sputum should be done first to identify a patient with invasive aspergillosis. In normal hosts the mere presence of Aspergillus does not necessarily indicate acute infection, however, in the immunocompromised host, finding the fungus should prompt the clinician to treat as an acute infection. The culture of the Aspergillus species in the sputum or by bronchoalveolar lavage with the identification of hyphae, which is the gold standard, will confirm that the infection is from Aspergillus and not another mold or fungus. Tissue biopsy of an aspergilloma may be helpful to confirm the diagnosis and exclude other conditions that may cause lung masses.[1][8][9]
Serum biomarkers such as galactomannan (approximately 50% positive pressure ventilation, approximately 90% negative predictive value) and beta-D-glucan assays can also be helpful. Galactomannan can also be measured in a sputum sample from a bronchoalveolar lavage. A positive Aspergillus IgG can also be helpful in diagnosing the chronic form of aspergillosis in the setting of a negative tuberculosis test.
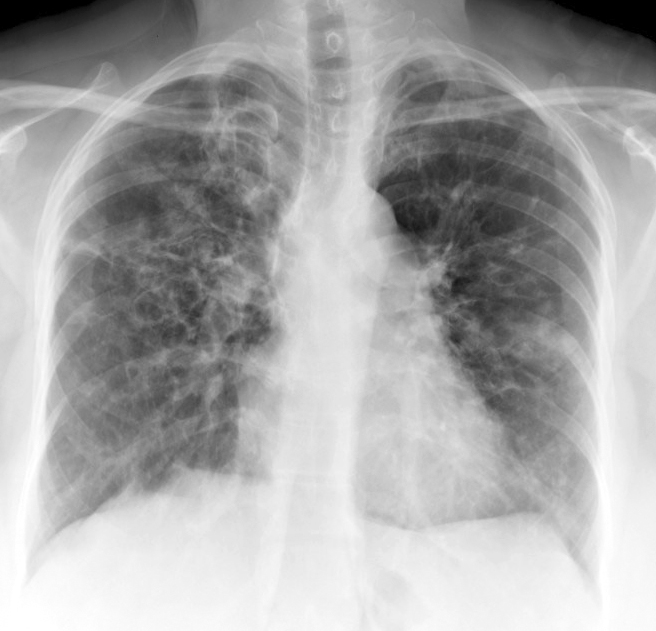
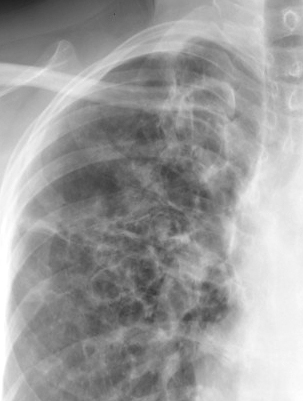
Chest radiographs may show parenchymal opacities of pulmonary aspergilloma (fungus ball). CT imaging of the lungs will show characteristic nodules with surrounding attenuation (“halo sign”), aspergilloma (fungal ball in a pre-existing lung cavity), cavitations, or fibrosis. CT may also be useful to evaluate for sinus involvement such as masses, opacification, or destruction of sinus walls if this manifestation of aspergillosis is suspected.
Treatment / Management
Treatment of suspected invasive aspergillosis should be initiated promptly as the patient's condition can decline quickly over 1 to 2 weeks from onset to death. Intravenous therapy for critically ill patients can include voriconazole (4 mg/kg, twice daily), posaconazole (300 mg IV, daily), micafungin (150 mg IV, daily) or amphotericin B (1 mg/kg, daily) for a 6 to the 12-week course. Voriconazole is considered the first-line treatment. While amphotericin is considered effective, it is deemed a second-line agent due to its adverse effect profile. Consideration should also be taken to resolve the patient's immunocompromised state as much as possible considering their comorbid conditions. [10] [11][12]
Treatment of patients with chronic pulmonary aspergillosis who are exhibiting pulmonary symptoms and loss of pulmonary function is accomplished with oral therapy of itraconazole (200 mg, twice daily) or voriconazole (200 mg, twice daily). A minimum of 6 months of therapy for all patients is recommended, though lifelong therapy for patients with the chronic progressive disease may be necessary. Failure of outpatient therapy usually requires hospital admission for intravenous (IV) therapy.
Treatment response is measured through evaluation of symptoms and following aspergillus titer. Repeat imaging (CT) may show the disappearance of the fungus ball and cavitary lesions decreasing in size. Repeat imaging should be done after a minimum of 2 weeks of therapy is completed.
Surgery along with antifungal therapy may be required to remove an aspergilloma. This approach is most effective in patients who have a single lesion and not diffuse disease. Intracavitary amphotericin has been attempted in a small trial of patients. Therapeutic embolization to control hemoptysis is another way to manage symptoms though it is not curative of the disease.[13]
Antifungal prophylaxis with voriconazole or posaconazole is recommended for patients with prolonged periods of neutropenia from chemotherapy, lengthy radiation treatments, allogeneic stem cell transplant recipients, severe or prolonged graft-versus-host disease, and solid organ transplant recipients.
Allergic bronchopulmonary aspergillosis exacerbations are typically treated with a 3 to 6-week course of oral corticosteroids in addition to itraconazole.
Differential Diagnosis
-
Asthma
-
Bacterial pneumonia
-
Bronchiectasis
-
Eosinophilia
-
Eosinophilic pneumonia
-
Fungal pneumonia
-
Heart transplantation
-
Heart-lung transplantation
-
Hypersensitivity pneumonitis
-
Liver transplantation
Prognosis
The prognosis of Allergic bronchopulmonary pulmonary aspergillosis is good in patients with mild alterations in function. But many patients may require steroids for a prolonged time if the diagnosis is delayed.
For patients with invasive aspergillosis, the prognosis is poor. Despite intensive antifungal therapy, the mortality remains high. Immunocompromised patients tend to have the highest mortality. Even those who are treated, tend to have a high recurrence rate. Once the infection has spread to the CNS, the mortality is close to 100%.
The high mortality in these patients has been blamed on resistance to the antifungal medications.
Complications
- Lung Fibrosis
- Continued wheezing
- Hemoptysis
- Respiratory failure
- CNS infection
- Endocarditis
- Death
Postoperative and Rehabilitation Care
While allergic aspergillosis can be managed as an outpatient, one still has to monitor the patient with serial IgE levels to determine the response to therapy.
Patients with invasive aspergillosis may require inpatient therapy for a few weeks until there is a resolution of symptoms.
Consultations
- A consult with a pulmonologist is highly recommended for initial treatment.
- Those with allergic aspergillosis may also need a referral to an allergist.
- A thoracic surgeon should be consulted for patients who do not respond or have hemoptysis.
- A Radiologist may be very helpful for embolization therapy in patients with acute hemoptysis.
Deterrence and Patient Education
Since invasive aspergillosis is fatal, the best way to decrease the morbidity and mortality is with the use of HEPA filters, which can lower the concentration of fungi in hospital rooms
In transplant patients, prophylactic antifungal therapy may decrease the risk of fungal infections.
Pearls and Other Issues
When aspergillosis is suspected, the following are recommended:
- Send all tissue and fluid for cytology, culture and histopathology
- If invasive aspergillosis is suspected, order a CT scan and bronchoscopy
- Measure levels of galactomannan as a marker for the disease
- Perform serum assays for D-glucan for invasive aspergillosis
- Start antifungal therapy at the first suspicion of invasive aspergillosis
Enhancing Healthcare Team Outcomes
Evidence-based Practice
Aspergillosis is a benign infection in immunocompetent individuals but it carries a very grave prognosis in transplant patients and those who are immunocompromised. In view of this, it is recommended that evidence-based guidelines be utilized to manage all cases of invasive fungal disease. The an interprofessional team should include healthcare professionals from a broad range of disciplines to coordinate care, including infectious disease and pharmacists. Open communication among consultant and adhering to clinical pathways is critical if one is to avoid the high mortality rates. Integrated diagnostic measures for aspergillosis such as the use of galactomannan and D-glucan levels should be utilized, as well as CT scan and bronchoscopy. Even at the slightest suspicion of invasive aspergillosis, the patient must be immediately started on antifungal agents [14] (Level V).
Outcomes
The outcomes for patients with allergic aspergillosis are good if the lung function is not compromised. However, delays in diagnosis may lead to steroid resistance and development of lung fibrosis. [15] (Level V). For patients who are immunocompromised or have undergone a transplant, invasive aspergillosis carries a mortality rate in excess of 50%. [16] (Level V).
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)