Anatomy, Shoulder and Upper Limb, Axillary Artery
- Article Author:
- Robert Thiel
- Article Author:
- Akul Munjal
- Article Editor:
- Daniel Daly
- Updated:
- 8/22/2020 10:14:27 PM
- For CME on this topic:
- Anatomy, Shoulder and Upper Limb, Axillary Artery CME
- PubMed Link:
- Anatomy, Shoulder and Upper Limb, Axillary Artery
Introduction
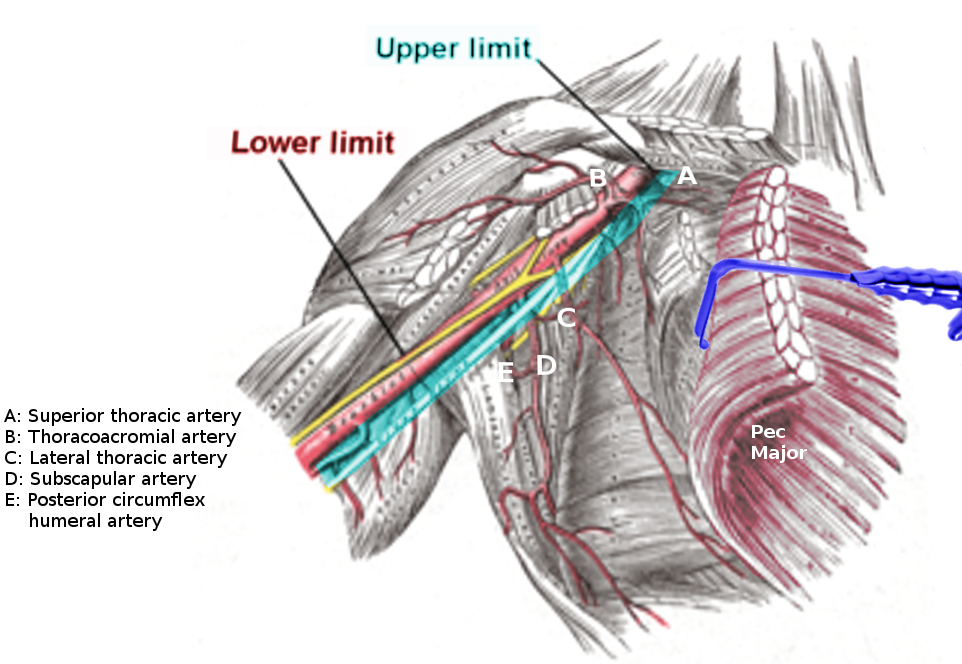
The axillary artery is a blood vessel that provides the axilla, the lateral portion of the thorax, and the upper limb with oxygenated blood. It consists of three parts separated by the pectoralis minor, which lies superficially to the artery. The first part is an extension of the subclavian artery. The delineation between the subclavian artery and the axillary artery is the lateral most border of the first rib. The axillary artery terminates at the lower border of the teres major muscle. It then continues as the brachial artery. The axillary vein accompanies the axillary artery. The vein runs medial to the artery along its entire length. The brachial plexus’ cords are intimately associated with the axillary artery, each being named according to its position relative to the second part of the artery. [1][2]
Structure and Function
The axillary artery is classically divided into three parts.
- The first part lies distal to the lateral border of the first rib and proximal to the pectoralis minor. It lies on top of the serratus anterior. It has one branch called the superior thoracic artery. This branch supplies the first two intercostal spaces superficially with oxygenated blood.
- The second part lies directly underneath or posterior to the pectoralis minor muscle, beginning at the upper border of the muscle and ending at the muscle's lower border. It has two branches. The first branch is the thoracoacromial trunk, which quickly divides into four arteries. These arteries are the acromial artery, the pectoral arteries, the clavicular artery, and the deltoid artery. The acromial artery provides blood to the acromion region of the scapula. The pectoral arteries provide blood to the pectoralis major and minor muscles. The clavicular artery provides blood to the subclavius muscle region. The deltoid artery provides blood to the deltoid region. The second branch of the second part of the axillary artery is the lateral thoracic artery. It provides blood to the lateral portions of the chest wall and the mammary gland.
- The third part lies distal to the lower border of the pectoralis minor muscle, anterior to the subscapularis muscle and teres major muscle. It has three branches that are variable in their order: the subscapular trunk, the anterior humeral circumflex artery, and the posterior humeral circumflex artery. The subscapular trunk is typically the largest branch of the axillary artery. It gives rise to the scapular circumflex artery and the thoracodorsal artery. The scapular circumflex artery runs through the triangular space and provides blood to the scapular region. The scapular circumflex artery eventually anastomosis with the suprascapular artery, thus connecting and providing a collateral route between the first and third parts of the axillary artery. The thoracodorsal artery provides blood to the latissimus dorsi muscle. The two remaining branches of the third part of the axillary artery, the anterior and posterior humeral circumflex artery, provide blood to the head of the humerus and shoulder joint. These arteries anastomose with one another. The anterior humeral circumflex is smaller and runs anterior to the humerus. The posterior humeral circumflex is larger and runs posterior to the humerus.
Embryology
Development of the upper limb arteries is very complex. The main artery develops lengthwise as the limb bud grows. Upper limb artery formation is also closely associated with bone development.
Physiologic Variants
Many variations of the axillary artery have been discovered and are discussed throughout the literature. The brachioradial artery is one of the variations in the axillary branching pattern. It is a terminal branch that has a superficial course distally. It travels through the cubital fossa, along the lateral portion of the forearm, and terminates in the deep palmar arch. This variation, along with other more rare variations discovered, has many surgical and diagnostic implications.[3]
Surgical Considerations
Clamping the axillary artery can be accomplished without harming the arm. Any surgical procedures concerning the axillary artery require delicacy due to the proximity of the brachial plexus. In cardiac surgery, the right axillary artery is frequently used as an arterial cannulation site, especially in the repair of aortic dissection.
Clinical Significance
Injuries to the axillary artery are rare but can cause limb loss. They most commonly arise from penetrating or blunt trauma to the shoulder. Examples include but are not limited to anterior shoulder dislocation, reduction of anterior shoulder dislocation, and humoral neck fracture. These mechanisms of injury may cause axillary artery rupture and subsequent thrombosis. Patients may present with pain, pallor, coldness, absent or delayed capillary refill, numbness or tingling, or lack of radial pulse to the injured limb. The collateral blood supply in the shoulder, however, may mask some of these symptoms. Thus, presentation of axillary artery injury is variable, so a high level of suspicion is essential. [4][5][6]
Axillary Artery Aneurysm
Axillary artery aneurysms are one of the injuries that can occur due to penetrating or blunt trauma. They may, however, develop from atherosclerotic processes over long periods of time. They often are associated with neurological complications due to the close proximity of the axillary artery and the brachial plexus. Aneurysms may arise from improper use of crutches. Presentation of these patients may include neurological deficits of the upper limb, ischemic fingers, or occlusion of the redial and ulnar arteries due to embolization from an aneurysm. Axillary aneurysms are confirmed by imaging. CT angiography is the most useful imaging technique when diagnosing. It is currently the gold standard. An alternative imaging modality includes magnetic resonance angiography when intravenous contrast is contraindicated. Ultrasound is also very useful for detection and diagnosis. An aneurysmectomy and grafting with a saphenous vein is commonly the surgical procedure employed to reverse these complications. Another treatment option for patients is an endovascular aneurysm repair.
Arterial Positional Compression
Axillary artery thrombosis and aneurysm may also be seen, although very rarely, in healthy athletes that preform frequent overhead throwing motions such as pitching a baseball or hitting a volleyball. In the throwing motion, the anterior displacement of the humerus places compression on the third portion of the axillary artery. Intermittent compression of the axillary artery may cause chronic changes in downstream vascular sufficiency. This could lead to subsequent thrombosis and aneurysm. Medical staff dealing with these athletes should be vigilant for symptoms of ischemic pain, cold intolerance, numbness, or arm fatigue immediately following practice or competition. Medical staff should note that symptoms will present later in the disease process due to the fact that only significant embolization or decreased blood flow causes perceptible changes in temperature or sensation. CT angiogram and magnetic resonance angiogram can be used to diagnose or screen athletes at risk of symptomatic arterial positional compression.