Basilar Artery Infarct
- Article Author:
- Asad Ikram
- Article Editor:
- Atif Zafar
- Updated:
- 8/10/2020 4:43:10 PM
- For CME on this topic:
- Basilar Artery Infarct CME
- PubMed Link:
- Basilar Artery Infarct
Introduction
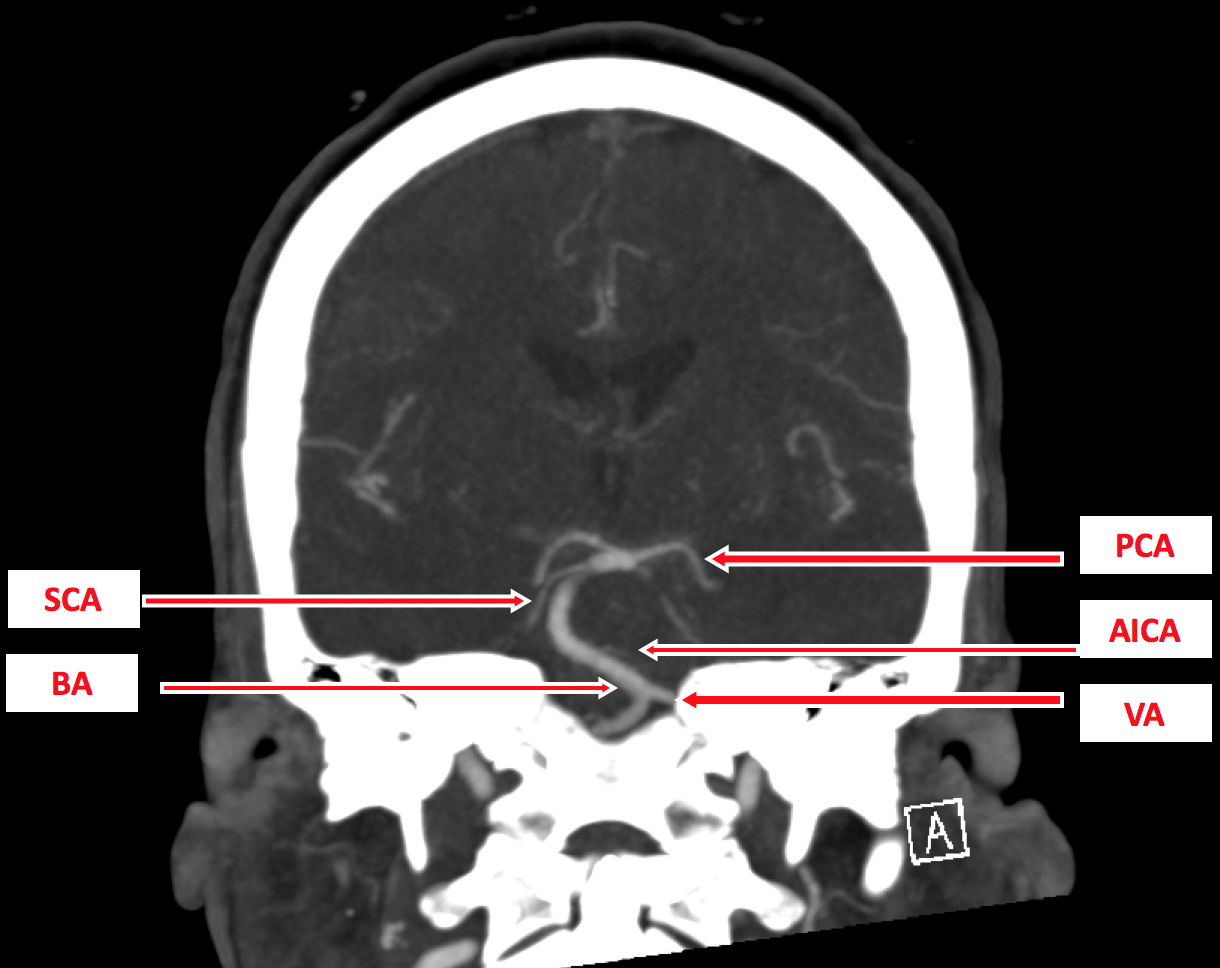
The basilar artery (BA) is formed over the surface of pons by two vertebral arteries to supply the critical areas of the brain and brainstem. Anatomically, it can subdivide into three arbitrary segments: proximal form vertebral artery (VA) to anterior inferior cerebellar arteries (AICA), middle from AICA to the origin of superior cerebellar arteries (SCA) and finally distal segment from SCA to the terminal posterior cerebral arteries (PCA).[1] Basilar artery infarct or occlusion (BAO) results from the obliteration of blood supply to the posterior circulation or vertebrobasilar system of arteries to the brain. BAO was first described in 1828 by Scottish physician John Abercrombie.[2]
The most common causes are atherosclerosis and thromboembolism from large vessel occlusion (LVO) or heart. The clinical presentation can be very mild as nausea, dizziness, headache, confusion, vertigo to the severe symptoms like aphasia, dysarthria, dysphagia, hemiparesis/quadriparesis, loss of consciousness, coma, cranial nerve abnormalities, vision loss and even cardiac or respiratory compromise which is usually lethal unless immediately identified to achieve revascularization.[1][3] Reduced consciousness is the hallmark of basilar artery occlusion. A patient presenting with these brainstem symptoms and signs qualifies for rapid evaluation, consult to the stroke and endovascular teams and an urgent imaging confirmation with computed tomography (CT) scan of the head, CT angiography of head and neck and/or magnetic resonance imaging (MRI) with or without perfusion imaging are usually done.[4] The whole process should not delay the administration of intraarterial thrombolytics like alteplase (tPA) or tenecteplase and transfer to angiography suite for mechanical thrombectomy (MT) in the eligible patients to achieve potentially good clinical outcomes.[5][6][5][7][8]
Etiology
The common causes of ischemic stroke can also cause infarct in the basal artery territory. Interruption to the blood supply due to atherosclerosis or from an embolus anywhere form the heart to the basilar artery can cause the obliteration of flow through the basilar artery leading to an infarct of the brainstem (mainly pons) or brain region supplied by the basilar artery and its branches. The most commonly involved segments are proximal and middle segments of the basilar artery.[9] Atherosclerosis of the phenomena by which cholesterol and repeat injury to the vessels leading to injury to the intimal side of blood vessels, exposing collagen and releasing factors leading to platelet adhesion to the surface forming a thrombus or plaque. When the plaque rupture, it can either close the vessel, ultimately leading to the high-grade vessel stenosis, and the organizing thrombus can further breakdown and throw the emboli in the cerebral circulation.
Alternatively, a small part of the thrombus can detach and cause occlusion of small vessels distally. Both mechanical symptoms eventually can cause the occlusion of several vessels leading to an infarct in the corresponding cerebral territories. Another mechanism is cardioembolism from the heart, where a clot in the heart mainly composed of fibrinogen, usually forms due to dysrhythmias like atrial fibrillation, metallic valve, severe mitral stenosis, large MI, acute heart failure and wall motion abnormalities, etc. Rarely, external compression of the vertebral artery (bow hunter syndrome or vertebrobasilar insufficiency) can cause posterior circulation stroke, which needs either endovascular deconstruction or reconstruction, external surgical decompression, surgical bypass techniques.[10]
Epidemiology
Although the exact incidence of basilar artery occlusion remains unknown, it is estimated to account for 1% of all ischemic strokes.[11] Data from the center, including 129 patients with an LVO, showed that the estimated incidence was four persons per 100000/year.[12] As per the Basilar Artery International Cooperation Study (BASICS) registry, among 592 patients with basilar artery occlusion, the average age of the aorta is 63 years, females being 37%, and admission National Institutes of Health Stroke Scale (NIHSS) of 22 (11 to 30).[13] In this era of advanced imaging in diagnosing techniques, we need further prospective randomized studies to determine the current incidence and prevalence of this disease, mainly because we have more treatment options for this patient population.
Pathophysiology
Almost 30 to 35% of the strokes in posterior circulation are due to an embolus originated from an LVO in VA, BA, and PCA. An occlusion of BA is often due to an LVO by an embolism from heart, aorta or VA (36%), atherosclerosis of BA (35%), dissection (5%) of BA and occasionally dolichoectasia or vasculopathy or undetermined (24%) causes.[13] Emboli usually arise from the heart or large arteries to cause occlusion of BA. In contrast, thrombus may arise directly from the basilar artery due to atherosclerosis to produce BAO or may propagate from a thrombus from a VA due to atherosclerosis or dissection. Often, both proximal and middle segments get occluded due to thrombi arising from bilateral vertebral arteries, and an embolus from VA can lodge into the distal section directly.[1]
The perfusion pressure drops due to the presence of an embolus in the proximal portion of BA, causing a reversal of blood flow from bilateral PCAs, and this reflux can prevent an embolus from reaching the distal segment of the BA.[14] Basilar syndrome is mostly caused by distal basilar artery occlusion and involves behavioral disturbance, confusion, oculomotor, and visual abnormalities but often spares motor findings. The extent of thromboembolism can be a single segment occlusion of BA or may involve all three segments of BA, and we can visualize this on the vessel imaging, preferably CT angiography of the head and neck. With time, as the occlusion ages, the embolus becomes harder to get extracted by thrombectomy. Hence time is of utmost importance.
Histopathology
Microscopic examination of the brain tissue in the autopsies shows ischemic changes due to a thrombus or an embolus. The histopathology examination of thrombus shows an increased amount of aggregated platelets consistent with the atherosclerotic disease. In contrast, there is an increased amount of fibrinogen in the emboli extracted from basilar arteries consistent with the cardioembolic etiology.
History and Physical
- Ipsilateral cranial nerve deficits, contralateral hemiparesis, sensory impairment, coordination deficits, quadriparesis, nausea, dizziness, headache, vertigo, aphasia, dysarthria, dysphagia, loss of consciousness, coma, and cardiopulmonary compromise can be caused by a variable degree of BAO.
- Confusion, oculomotor abnormalities, and bilateral central vision loss and often seizures can result from basilar tip occlusion, also called the top of the basilar syndrome.[15]
- Dysphagia, ataxia, and Ipsilateral sensory impairment over the face, as well as Horner syndrome, is caused by occlusion of VA and PICA.
To guide history and physical examination, the following is a summary of specific signs or symptoms based on the infarct location[1]:
- spinothalamic tracts, medial lemnisci, and thalamic nuclei involvement lead to anesthesia or hypesthesia
- corticospinal tracts in the cerebral peduncles and pons cause hemiplegia or quadriplegia and extensor plantar sign
- ascending reticular activating system with coma or impaired consciousness
- cerebellar peduncles, cerebellum, proprioceptive tracts involvement cause loss of coordination of limbs and posture (ataxia)
- labyrinth, vestibulocerebellum, vestibular nuclei involvement leads to loss of balance, vertigo, and directional nystagmus
- dorsal longitudinal fascicle (sympathetic fibers) dysfunction cause Horner's syndrome
- trigeminal fibers involvement causes head and neck pain
- efferent and afferent fibers and medullary autonomic nuclei cause cardiopulmonary signs and symptoms
- sympathetic and parasympathetic fibers and hypothalamic nuclei involvement leads to incontinence
- cranial nerve III nuclei, dorsal commissure, and rostral interstitial nucleus of the medial longitudinal fascicle (MLF) involvement lead to variable oculomotor palsy, bilateral ptosis, vertical gaze paresis, non-reactive pupils, anisocoria and loss of vestibulocochlear reflex
- MLF involvement cause internuclear ophthalmoplegia
- CN VI nucleus and paramedian pontine reticular formation (PPRF) involvement cause horizontal oculocephalic reflex loss and horizontal gaze paresis
- CN VII nuclei and corticobulbar tract involvement cause facial palsy
- cerebellar involvement cause gaze-evoked nystagmus
- brainstem oculomotor system, and CN II, III, IV and VI cause diplopia and strabismus
- CN VII nuclei and lateral lemniscus involvement cause hearing loss, vertigo and tinnitus
- cerebellum, corticobulbar tracts, and caudal cranial nerve nuclei (X, XI) involvement cause dysarthria and dysphagia
- occipital lobe involvement leads to vision loss or hemianopia
- medial temporal lobe and thalamic nuclei involvement cause memory disturbance, confusion, and disorientation
- pyramidal tracts involvement causes jerking, shaking, convulsive seizures, and extension posturing or rigidity
Evaluation
On arrival to ED, the first test should be a CT head without contrast to rule out hemorrhagic stroke. In the meantime, quickly gather information including blood pressure, blood glucose level, the time of last known normal (LKN) or onset of stroke signs/symptoms (s/s), National Institute of Health Stroke Scale (NIHSS), use of anticoagulants/antiplatelets, past medical and surgical history, renal function, and if indicated run the alteplase (tPA) checklist. If CT head is negative for bleed and there is a concern for basilar artery occlusion (BAO), subsequent intravenous access and CT angiogram of head and neck is advised to rule out an LVO. If CT angiogram is unobtainable, an MR angiogram can be used to evaluate cerebral vessels provided no contraindication. MRI brain without contrast can be done later to characterize the stroke further, but it should not delay the revascularization treatment with intraarterial thrombolysis (IAT) and mechanical thrombectomy (MT).[16] In the diffusion-weighted imaging (DWI) sequence of the MRI scan, the nerve density of the tracts in the pons may appear "SMOGGY" or "hazy," due to the diffusion restriction in the axonal tracts. This "smog sign" is a predictor of a good predictor of neurologic outcomes after mechanical thrombectomy.[8]
After the initial management, stroke workup should be done to evaluate the cause to guide the goal-directed treatment. After the evaluation of vertebral and basilar circulations, other workup includes a transcranial doppler (TCD to find out the stability of plaque), transthoracic echocardiogram (TTE or TEE to rule out the clot, valvular abnormalities, wall motion abnormalities, and PFO), electrocardiogram, telemetry, event monitor or loop recorder (to rule out arrhythmias), and blood workup (HbA1c, lipid panel, homocysteine, and other workup based on etiology: antiphospholipid antibody syndrome, verify-now for platelet function, malignancy workup, etc.).[17]
Treatment / Management
If the patient has arrived within the tPA window (less than 3 to 4.5 hours since LKN) and has no contraindication to tPA, he/she should immediately receive alteplase/tPA or tenecteplase for the intraarterial thrombolysis. If eligible, the patient should be transferred to the angiography suite for mechanical thrombectomy (MT) within 24 hours of LKN.[4][6][16] Everyone should be considered for tPA if the patient has arrived in the ED within the window and has no contraindication is present. The patient should first receive tPA if eligible, and after tPA administration, the patient should transfer to an angiography suite for MT. Admit patients to the neuroscience ICU for the post-tPA and post-MT care, including neuromonitoring, hemicraniectomy watch, airway watch, respiratory support, blood pressure management, and symptomatic care.[17] Further management should take place at the stroke unit with a multidisciplinary team approach rather than an admission to the general ward.[18]
Patients who are not tPA candidates, and who have a plaque burden in the posterior circulation are manageable through acute anticoagulation or antiplatelet regimen. Recent data is supporting the use of single or dual antiplatelets, over anticoagulation for large artery atherosclerotic disease, particularly if there is a large infarct burden.[19][20] For intracranial atherosclerosis, it is recommended to use dual antiplatelets for 90 days after stroke and followed by aspirin only.[21] Further details regarding the management of basilar artery occlusion and ischemic stroke of currently available and ongoing data can be found in the "pertinent studies and ongoing trial" section of this review. However, be advised that most of the currently available data came from anterior circulation strokes rather than posterior circulation strokes. Secondary prevention, including the use of aspirin, atorvastatin, and anticoagulants if indicated. At the time of discharge, vascular risk factor modification with LDL goal below 70, a blood pressure goal less than 130/80, and reasonable glycemic control with A1c goal under 6.5, as well as the goal-directed treatment, should be considered based on the etiology of stroke.[22] Also, lifestyle modification, including the Mediterranean diet, smoking cessation, limit alcohol, and no illicit drugs, have proven benefits in preventing stroke recurrence.
Differential Diagnosis
- Basilar meningitis
- Basilar migraine
- Cerebellar infarct with brainstem compression and edema
- Drug-intoxication
- Encephalopathy
- Hemorrhagic stroke:
- Cerebellar hemorrhage with brainstem compression
- Pontine hemorrhage
- Focal deficits due to brainstem bleeding from ruptured cerebral cavernous malformations,[23] atriovenous malformation, and fistulas
- Multiple sclerosis [24]
- Seizures
- Tumors in the posterior fossa, leading to mass effect and brainstem compression
Pertinent Studies and Ongoing Trials
Heparin after an acute ischemic stroke
- TOAST (Trial of ORG 10172 in Acute Stroke Treatment) trial [1998] showed no favorable 3-months outcomes with the use of heparinoids after an acute ischemic stroke.[25]
TPA (tissue Plasminogen activator or alteplase) after an acute ischemic stroke
- NINDS (National Institute of Neurological Disorders and Stroke- tPA/tissue plasminogen activator/alteplase) trial [1995] reported the significantly improved outcomes with the use of tPA within 3 hours of acute ischemic stroke onset, despite the increased risk of symptomatic intracerebral hemorrhage.[26]
Thrombectomy in LVO
- The DAWN (Clinical Mismatch in the Triage of Wake Up and Late Presenting Strokes Undergoing Neurointervention With Trevo) trial [2018] showed that in patients with acute ischemic stroke with LVO who received medical management (MM) only versus medical management plus mechanical thrombectomy (MM+MT), with the onset of symptoms between 6 and 24 hours and having a mismatch between infarct core and clinical signs and symptoms, the 90 disability was lower in thrombectomy group as compared to patients receiving standard of care treatment.[6]
- DEFUSE-3 (Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke 3) trial [2018] showed that in patients with acute ischemic stroke (MCA or ICA LVO), with MR perfusion mismatch ratio of greater than 1.8 and infarct volume of less than 70 mL; who received either medical management (MM) alone or medical management plus mechanical thrombectomy (MM+MT), within the 6-16 hours of symptoms onset, the 90 disability was lower in thrombectomy group as compared to patients receiving standard of care treatment.[4]
Carotid Endarterectomy (CEA) for atherosclerotic LVO
- NASCET (North American Symptomatic Carotid Endarterectomy (CEA) Trial Collaborators) trial [1991] showed the benefit of CEA in preventing ischemic strokes in patients with over 70% carotid artery stenosis after TIA and small strokes.
- CREST (Carotid Revascularization Endarterectomy (CEA) Versus Stenting (CAS) Trial) trial [2016] is a huge trial, and after long-term 10-years follow up showed that there was no net outcome difference between the two procedures except in patients over 70 years old, CAS might have more bleeding and procedural complications.[27]
Aspirin+Plavix (dual antiplatelets) appeared to superior to aspirin alone in preventing strokes after TIA/small ischemic strokes
- The CHANCE (Clopidogrel in High-risk Patients With Acute Non-disabling Cerebrovascular Events) trial [2013] is also a randomized, double-blinded, placebo-controlled trial (including 5170 subjects), that compared aspirin monotherapy versus aspirin/clopidogrel in 114 centers across China. The bottom line suggests that in patients with acute TIA or small ischemic stroke, starting dual antiplatelet therapy (clopidogrel load 300 mg then 75 mg/d, aspirin 75 to 300mg/d and placebo group with no other thrombolytics for 30 days) after the symptom onset decreases 90-day stroke risk at the cost of a slightly increased bleeding risk as compared to aspirin monotherapy.[20]
- The POINT (Platelet-Oriented Inhibition in New TIA and Minor Ischemic Stroke) trial [2018] is a randomized, double-blind, placebo-controlled trial (including 4881 subjects), that compared aspirin monotherapy versus aspirin/clopidogrel in 269 centers in North America, Europe, Australia, and New Zealand. The bottom line suggests that in patients with acute TIA or small ischemic stroke, starting dual antiplatelet therapy (clopidogrel load 600 mg then 75 mg/d, aspirin 75 to 325mg/d, and placebo group with no other thrombolytics for 30 days) after the symptom onset decreases 90-day stroke risk at the cost of a slightly increased bleeding risk as compared to aspirin monotherapy.[28]
- Summary of POINT and CHANCE trials: In point trial, the duration of treatment was longer (90 versus 30 days), and clopidogrel dose was higher (600 versus 300), but it is unclear if this was the reason for slightly higher bleeding rates in POINT trial. Although pooled analysis shows that after comparing these two trials, the benefit of dual-antiplatelet therapy appeared limited to 21 days after an ischemic stroke.[29]
- The ASCEND (A Study of Cardiovascular Events iN Diabetes) trial [2018] showed that the use of aspirin for the primary prevention therapy reduces the risk of serious vascular events in patients with well-controlled diabetes (A1c<8; 50% of patients).[19]
Intracranial Arterial Stenosis
- SAMMPRIS (Stenting versus aggressive medical therapy for intracranial arterial stenosis) trial [2011] for intracranial arterial stenosis comparing the roles of addressive medical management (MM) with percutaneous transluminal angioplasty and stenting (PTAS) to prevent recurrent stroke. It reports that MM (i.e., dual antiplatelets for 90 days and aspirin thereafter) is superior to the intracranial stenting in reducing ischemic stroke risk.[30]
Lacunar strokes (small vessel disease)
- SPS 3 (Secondary Prevention of Small Subcortical Strokes) trial [2012] reported that among patients with lacunar strokes use of starting dual antiplatelet therapy (Aspirin and Plavix) is not associated with significant stroke risk-reduction but instead showed an increased risk of bleeding and mortality as compared to aspirin alone. Hence, the use of dual antiplatelet therapy is not indicated after lacunar strokes.[31]
Afib (atrial fibrillation)[32]
- EMBRACE (30-Day Cardiac Event Monitor Belt for Recording Atrial Fibrillation After a Cerebral Ischemic Event) trial [2014] recommends 30-day cardiac monitoring to increase the yield of AFib detection and subsequent goal-directed anticoagulation treatment to prevent recurrent strokes by risk factor modification.[33]
- CRYSTAL AF (Study of Continuous Cardiac Monitoring to Assess Atrial Fibrillation After Cryptogenic Stroke) trial [2014] for AFib detection using prolonged cardiac monitoring for 6 to 12 months using an insertable cardiac monitor was proved superior to identify atrial fibrillation in patients after the admission of stroke.[34]
Cryptogenic strokes and atrial cardiopathy
- ARCADIA (AtRial Cardiopathy and Antithrombotic Drugs In prevention After cryptogenic stroke) trial [2019] is currently enrolling patients with cryptogenic strokes based on atrial cardiopathy on echocardiogram, NTpBNP, and EKG V1 findings.[35]
Patent foramen ovale (PFO) closure
- RESPECT (Randomized Evaluation of Recurrent Stroke Comparing PFO Closure to Established Current Standard of Care Treatment) trial [2017] showed that combined PFO closure and antiplatelet therapy is superior to medical management (antiplatelets) alone to prevent recurrent ischemic strokes.[36]
- CLOSE (Patent Foramen Ovale Closure or Anticoagulants Versus Antiplatelet Therapy to Prevent Stroke Recurrence) trial [2017] reports that combined large PFO closure and antiplatelet therapy is superior to medical management (antiplatelets) alone to prevent recurrent ischemic strokes but with an increased risk of atrial fibrillation after PFO closure.[37]
Hyperlipidemia and Hypertriglyceridemia
- SPARCL (Lipitor In The Prevention Of Stroke, For Patients Who Have Had A Previous Stroke) trial [2006] for high dose statin use in patients with TIA or ischemic stroke showed significant stroke risk-reduction with the use of high dose (81mg) atorvastatin by treating and preventing atherosclerosis.[38]
- REDUCE-IT (Reduction of Cardiovascular Events With EPA - Intervention Trial) [2019] trial reports reduction in stroke risk in patients who received Icosapent Ethyl (highly purified eicosapentaenoic acid ethyl ester) twice daily (toral 4 g/Day)with hypertriglyceridemia despite being on high-dose statin therapy.[39]
Post-stroke depression, motor recovery, and role of SSRI
- FLAME (Fluoxetine on Motor Rehabilitation After Ischemic Stroke) trial [2011] showed improved motor recovery in patients with hemiplegia and hemiparesis with the use of fluoxetine.[40]
Treatment Planning
As described above initial revascularization followed by secondary prevention should be performed in BAO patients.[17]
Toxicity and Side Effect Management
The most significant side effects of thrombolysis and mechanical thrombectomy are intracranial hemorrhagic transformation, groin/femoral artery perforation/bleeding complications, death, and disability. Prognosis and outcomes should be discussed in urgency with the family while administering alteplase and wheeling patients for thrombectomy.
Prognosis
Prognosis of BAO depends on the severity of the stroke, time to LKN, the treatment offered, successful recanalization, and access to tertiary care hospital and comprehensive stroke center. Overall, mortality is very high in this population, in patients with successful recanalization after thrombectomy has a lower mortality rate of 33 to 50%, versus 74 to 100% in patients without thrombectomy or failed reperfusion.[41] With early arrival and appropriate management, as described above, the outcome may be good, with minimum deficits. But late arrival and failure of revascularisation of BAO invariably result in poor outcomes, including severe neurological deficits and very high mortality in these patients.
Complications
- Death
- Intracranial or extracranial bleeding
- Reperfusion syndrome
- Ischemic stroke
- Groin puncture site hematoma, fistula, and intraabdominal bleeding
- Infections (urinary tract infection, pneumonia)
- Pressure ulcers
- Contractures
- Dysphonia
- Dysphagia
- Deep vein thrombosis/Pulmonary embolism[42]
Postoperative and Rehabilitation Care
- Respiratory therapy
- Physical therapy
- Occupational therapy
- Speech therapy
Consultations
An interprofessional team approach, including emergency department, neurology (stroke), neurosurgery, neurocritical teams, as well as nursing, physical therapy, occupational therapy, and speech therapy collaboration, is essential and the key to good outcomes in patients with basilar artery occlusion.
Deterrence and Patient Education
Counsel the patient and family regarding stroke that the risk of a stroke can be decreased by appropriately treating diabetes, hypertension, high cholesterol, cardiac diseases, obesity, and by quitting smoking, reducing alcohol intake, and staying physically active. Time is of the essence. Discuss the BE-FAST (balance loss, eyesight, facial droop, arm weakness, slurry speech, time) symptoms awareness on all the media and public education channels and campaigns.
The risk of a stroke can be decreased by treating hypertension, high cholesterol, diabetes, heart disease, and obesity and by quitting smoking, limiting alcohol, and staying physically active. Time is of the essence. It is essential to seek treatment within 3 to 4.5 hours of the start of symptoms because, during that time, thrombolytic drugs are an option. Even if one does not know when symptoms began, get treatment as soon as possible. After the 4.5-hour window has passed, treatment may include rest, oxygen, intravenous (IV) fluids, and medicines to thin the blood (anticoagulants). Treatment of stroke depends on the duration, severity, and cause of one's symptoms. Medications and diet may be used to address diabetes, high blood pressure, and other risk factors. Physical, speech and occupational therapists will assess and work to improve any functions impaired by the stroke. Measures will be taken to prevent short-term and long-term complications, including infection from breathing foreign material into the lungs (aspiration pneumonia ), blood clots in the legs, bedsores, and falls. Rarely, surgery may be needed to remove large blood clots or to open up blocked arteries.
Pearls and Other Issues
- For basilar artery infarct, currently available data is inadequate and needs further extensive randomized prospective clinical trials to study pathophysiology. A better scoring system needs to be developed, which is dedicated to posterior circulation strokes to use for prognostication of ischemic strokes secondary to BAO. Also, educational programs and campaigns should be done regarding BAO for both health care providers and patients to improve outcomes of this devastating disease process.
- Other emerging therapies include MRI-guided high-intensity focused ultrasound (HIFU) technique, which uses thermal heating for sonothrombolysis and ablation.[43] Some in-vitro and in-vivo studies have evidenced it, but in both ischemic and hemorrhagic strokes, more extensive prospective studies are necessary. This technique should have research for basilar artery infarct due to basilar artery anatomy and potential ease of access in performing thrombolysis.
- A small number of strokes occur after cardiac and cardiovascular bypass grafting surgeries. The use of perioperative epiaortic ultrasound is potentially useful to detect thrombus during surgery to prevent perioperative ischemic strokes.[44]
- Elevated levels of cytokines like interleukin-37 are associated with an acute ischemic stroke, and further studies are being conducted to determine the role of these chemokines and cytokines in the CRISP trial (NCT03297827).[45]
Enhancing Healthcare Team Outcomes
Measures should be taken to prevent short-term and long-term complications, including infection from breathing foreign material into the lungs (aspiration pneumonia), UTI, DVT, PE, bedsores, dysphonia, dysphagia, and falls. Aggressive physical and occupational therapies should treat post-stroke complications like contractures, follow-up in the neurology clinic, and consideration of botox injection may help with recovery from contractures. Rarely, surgery may be needed to remove large blood clots or to open up blocked arteries. Another significant complication is post-stroke depression; we should be treated by citalopram or fluoxetine, which has been proved beneficial and recent studies for post-stroke depression and motor recovery after stroke.
There is a lot of high-quality evidence regarding the prevention and management of stroke, as described in any organized and comprehensive stroke guidelines in 2018.[46] Here is is the summary of stroke prevention and management with the corresponding class of recommendation (COR=strength of study) and level of evidence (LOE=quality of study):
- Prehospital systems:
- "Time is brain," hence, is of crucial importance that prehospital arrangements to be made so that patients can be brought to the hospital for the treatment as early as possible. There is a need for education like BE-FAST (dependence, eye or vision, facial droop, arm weakness, speech slurring, and time), etc. as well as education programs and awareness campaigns to make the general population of air off the importance of time. Especially, African-Americans, Native Americans, Hispanics, and other undersurface populations are greatly affected due to the lack of awareness. In a very systemized, targeted manner and campaignings, this issue merits attention. [COR: I and LOE: B-R]
- Activating stroke alert by calling 9–1–1 for any stroke symptom should be encouraged to the public, including family members, are bystanders witnessing someone with the symptoms described above. [COR-I and LOE B-NR]
- It is a strong recommendation that due to increased awareness and decreased time to transit to the hospital, more patients are treated and expand programs for the education of healthcare professionals, including physicians, EMTs, and patients. [COR: I and LOE B-NR]
- Hospital stroke teams:
- There should be a stress on very organized emergency and stroke teams in the hospital, for that there should be a validated protocol for standard procedures and establish to as soon as the hospital is being alerted of stroke arrival by EMS so stroke alert can be activated. The stroke team should be readily available in the emergency department to manage the stroke appropriately. In summary, the recommendation that the clinical staff sees the patient within 15 minutes of ED arrival, CT head without contrast takes place within 25 minutes of ED arrival, and TPA or door-to-needle time should be 60 minutes. [COR-I and LOE B-NR]
- Organization and capacity building:
- In the small hospitals or primary stroke centers, realistic measures should be in place so that initial studies including vascular imaging like CT angiograms are possible in those hospitals before transferring to the larger centers are comprehensive stroke centers. [COR: IIb and LOE: C-LD]
- Mechanical thrombectomy should be performed in the larger stroke centers, with the capacities and capabilities of stroke teams, neurologists, neuro-interventionists, and availability of advanced imaging including perfusion scans, etc. [COR: I and LOE: C-EO]
- Data Repositories:
- It is highly encouraged to build date the repository and research registries in the centers, so that adherence to the protocols and guidelines as well as improvement in patient outcomes is done [COR: I and LOE: B-NR]
- Telemedicine and telestroke services [COR: I and LOE: A]
- Use of Stroke Scales like NIH stroke scale [COR: I and LOE: B-NR]
- Quality improvement processes and system for stroke [COR: I and LOE: B-NR]
- To prevent a recurrence, the primary care providers and the stroke nurse should educate the patient on lowering the risk factors; this means discontinuing smoking, exercising regularly, controlling blood pressure and lipids, and eating a healthy diet.
An interprofessional team approach is necessary for improving outcomes in patients with basilar strokes. In addition to the various clinical specialties already covered, a pharmacist should consult for thrombolytic therapy; this may well be a cardiac board-certified pharmacist. Stroke-certified nursing staff is an invaluable resource, irrespective of which direction therapy takes; they can help in evaluating the patient, assist during procedures, and monitor the patient's condition following interventions, charting, and reporting their findings for the clinician staff. These types of interprofessional actions enhance patient outcomes in basilar artery occlusion and other types of strokes. [Level 5]
(Click Image to Enlarge)

Figure 2 - Schematic diagram of the posterior cerebral artery and its branches: 1, basilar artery (BA); 2, superior cerebellar artery (SCA); 3, posterior cerebral artery (PCA); 4, thalamosubthalamic arteries; 5, posterior communicating artery; 6, internal carotid artery; 7, polar artery of thalamus; 8, posterior choroidal artery; 9, thalamogeniculate artery; 10, anterior inferior temporal artery; 11, posterior inferior temporal artery; 12, occipitotemporal artery; 13, calcarine arteries; 14, occipitoparietal artery
Contributed by Okkes Kuybu, MD and Diana
(Click Image to Enlarge)