Bilobed Flaps
- Article Author:
- Rosalind Mole
- Article Author:
- Talel Badri
- Article Editor:
- Nicholas Sebes
- Updated:
- 9/13/2020 8:41:33 AM
- For CME on this topic:
- Bilobed Flaps CME
- PubMed Link:
- Bilobed Flaps
Introduction
The bilobed flap is a local flap used primarily for the reconstruction of small to moderate cutaneous nasal defects. It was first described in 1918 by Esser for use in nasal tip reconstruction. The original flap used a rotational arc of 180 degrees and based the second lobe superiorly towards the glabellar region.
In 1953 Zimany demonstrated that the second and third lobes could be smaller than the first and that the flap could be utilized for reconstruction in more anatomical areas. In the 1980s, McGregor and Soutar introduced the concept that a reduced pivotal angle would result in smaller standing cutaneous deformities and decreased pin-cushioning. Zitelli went on to describe limiting the total rotational arc to between 90 to 110 degrees. This variant is the most common modification in use today. This overview of the bilobed flap will focus on the most recent modification. It will describe the relevant anatomy, the situations in which you might choose to use the bilobed flap, and describe in detail how to plan and execute this valuable flap.[1][2][3]
Anatomy and Physiology
The bilobed flap is a double transposition flap where the first flap (or lobe) serves to fill the primary defect, and a further flap (or lobe) fills a secondary defect. This approach seeks to distribute tension across a wider area. It is a random pattern flap. The random pattern nature of the flap means that the flap has no specified blood supply. The flap is supplied by the musculocutaneous and cutaneous arteries that perforate through the subcutaneous tissue.[4][5][6]
Indications
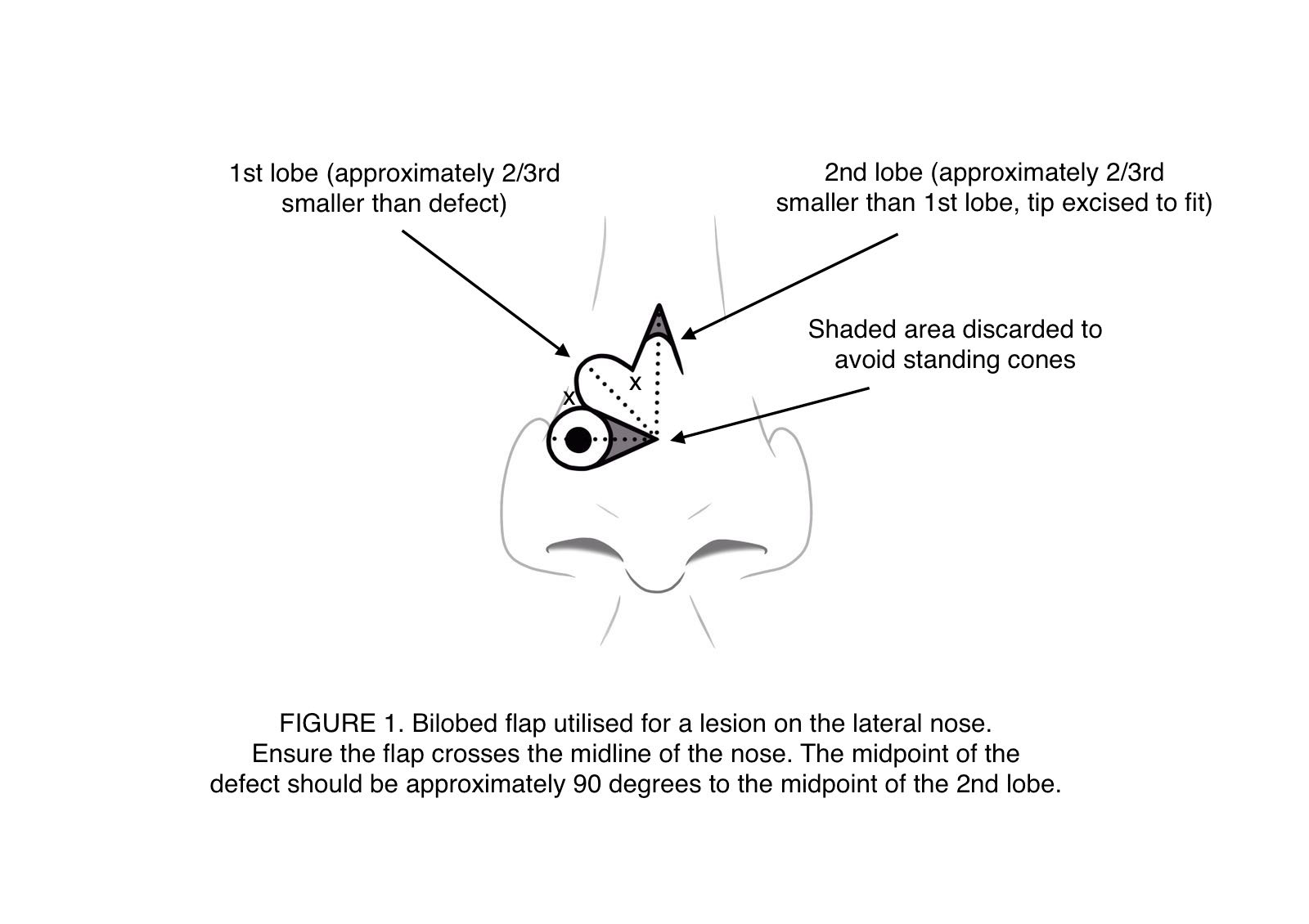
The bilobed flap was first described for its use in reconstruction of the nasal tip using a rotational arc of 180 degrees and having the second donor site in the glabellar region. This technique has fallen out of favor as the large arc created large flaps that require significant undermining. It is now more commonly used for reconstruction of the lateral portion of the nose. It utilizes the mobile skin of the cephalic part of the nose to reconstruct the more immobile skin in the caudal part of the nose. The second donor site should remain in the superior plane towards the glabella (see image).
The bilobed flap is very versatile, and although frequently associated with nasal reconstruction, it is, in fact, beneficial in many anatomical locations. Tissiani et al. describe the versatility of the bilobed flap in a case series of 42 patients who had bilobed flaps undertaken in a wide range of anatomical sites including, but not limited to, cheek, upper lip, zygoma, upper limb, and lower limb.[7][8][9]
Contraindications
Cutaneous scars in the flap donor area is a contraindication.
Equipment
This procedure can be undertaken with a standard, minor operations surgical set.
Personnel
Plastic surgeons and dermatologists most commonly undertake this local flap. As it is performed in a sterile field, a scrub nurse and a theatre runner are essential members of the team.
Preparation
Patients should receive education about what to expect from the surgery, including counseling the patient about the theatre setting, explanation of the procedure and possible complications, and what to expect in the post-operative period. The clinician should have the patient sign a consent form.
Technique
The vast majority of these flaps will be undertaken under local anesthetic. The infiltration of the local anesthetic often results in distortion of lines of contour. Therefore, the flap should be planned and drawn before the infiltration of local anesthetic.
This article will use the example of the side wall of the nose to illustrate planning the bilobed flap. When planning local flaps on the nose, it is advisable to try and avoid crossing the delineation of the nose and the cheek. The second lobe of the flap should be positioned superiorly, pointing towards the glabellar region.
Firstly, the lesion due to be removed should be marked with an appropriate margin circumferentially. The pivot point should be marked across the dorsum of the nose 0.75-1 x the wound diameter. The first transposition flap (lobe) should be the length of the defect with a narrower base. The second transposition flap (lobe) should be slightly longer, have a narrower base than the first lobe, and be excised with a triangular tip. This triangular excision will produce a linear scar and decrease the chance of having a dog ear. The pivot point is the right angle produced by the horizontal axis through the midpoint of the defect and the vertical axis through the midpoint of the second lobe. This approach produces a total transposition arc of 90 degrees, with each transposition flap having an arc of 45 degrees. The triangle of skin which traverses the area between the defect and the pivot point is excised as excess. The local flap should then be raised as per the pre-operative markings. Ensure the thickness of the flap is uniform and appropriate to fill the defect. The first step of insetting the flap is a deep suture with an absorbable stitch at the angle created by the separation of the lobes (see figure, x to x). The remainder of the flap is then secured in place. The tip of the second lobe requires trimming to fit nicely into the secondary defect created by the first lobe.
Complications
The possible complications specific to this procedure are swelling, scarring, flap necrosis, infection, and bleeding. Due to the crescentic shape of the flap, it is at risk of developing pincushion deformity as a result of tissue contraction beneath the flap. With less tension, this improves. The small rotation arc helps to reduce tension. Standing cutaneous deformities are also a risk, and again can be reduced with a smaller rotation arc. In the original bilobed flap, as described by Esser as 180-degree rotation, standing cutaneous deformities were almost inevitable. If the tension of the flap is too great, it can undergo necrosis. Infection can occur in any area of the wound, but it is most associated with areas of necrosis. Post-operative bleeding can result in hematoma formation, which can go on to compromise the flap.
Clinical Significance
The bilobed flap is a versatile local flap that spreads tension vectors across a wide surface area and recruits skin from areas where there is relative mobility to close defects in areas where the skin is relatively immobile.
Enhancing Healthcare Team Outcomes
The bilobed flap is versatile and can be used in many parts of the body to revise or reconstruct skin defects. The plastic surgeon primarily performs the flap. Wound care nurses and physicians who have patients with facial and extremity defects that need closure should consult with a plastic surgeon.