Blount Disease
- Article Author:
- Dakshina Murthy T S
- Article Editor:
- Alessandro De Leucio
- Updated:
- 7/27/2020 11:21:16 AM
- For CME on this topic:
- Blount Disease CME
- PubMed Link:
- Blount Disease
Introduction
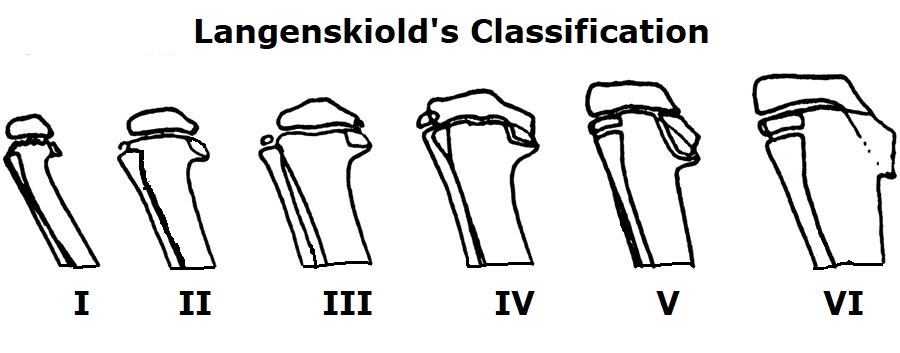
In 1937 Blount described a bilateral genu varus deformity in children. In 1964 in Sweden, Langenskiold and Riska suggested a radiograph based classification for the same. Infantile and adolescent variants are observed in this disease based on clinical presentation. Infantile type is seen under 4-year male children in both limbs, while adolescent variant is seen in the later ages of childhood .unilaterally.Parents usually notice the deformity bilaterally when the child starts walking. Obesity, African-American lineage, and early walkers are more prone to develop this disease. Medial proximal tibial physis defect, mainly in cartilage, is the cause for genu varum in these cases. The severity varies from articular cartilage irregularities to limb length discrepancies.[1]
Etiology
The etiology of Blount disease is thought to be multifactorial. Mechanical overload and genetic susceptibility are considered as risk factors. Mechanical overload leads to osteochondrosis of the medial proximal tibial physis and epiphysis, later progresses to a physical bar. Overweight children, in particular in specific demographic populations such as Hispanics and Blacks, are reported as more likely to develop this condition.
Epidemiology
Infantile Blount disease, also known as pathologic genu varum, is generally seen in children 2 to 5 years of age, with males more likely to develop than females and bilateral 50% of the time. Adolescent Blount disease, also known as adolescent genu varum, is more likely to be seen in children >10 years of age, generally less severe, more likely to be unilateral. Infantile Blount disease is more frequent than adolescent Blount disease and typical of the early walkers, Hispanics, and Afro-Americans.
Pathophysiology
Mechanical overload and genetic susceptibility are risk factors. Mechanical overload leads to osteochondrosis of the medial proximal tibial physis and epiphysis, later progresses to a physeal bar. Overweight children, in particular in specific demographic populations such as Hispanics and blacks, are reported as more likely to develop this condition. Langenskiold classified the progression of the disease in four stages according to the medial metaphyseal slope, the angulation, and the aspect of a metaphyseal bar.[2]
History and Physical
The typical patient is an overweight black African, African-American, or Afro-Caribbean child. Disease onset is before three years of age. The prevalence of early-onset Blount disease in the Caribbean has been estimated at 1/1200 live births. Early ambulation, before ten months of age, is common. The physiologic bowing of the legs becomes more marked and often asymmetrical. The abnormality is bilateral initially in 50% of cases.
The growth disorder occurs at the posteromedial proximal tibia and results in a three-dimensional deformity combining varus, procurvatum, and internal tibial rotation, as well as in limb length discrepancy. Lateral thrust during weight-bearing is a critical clinical finding. Irreversible asymmetric medial proximal tibial epiphysiodesis usually develops towards 6 to 8 years of age, making conservative treatments ineffective. The knee deformities and associated abnormalities worsen gradually.[3] The child's gait should be carefully observed. The lateral thrust of the knee at the initiation of the stance phase is typical. Persistent genu varum in a young overweight child, particularly of Afro-Caribbean ethnicity, is often the first indicator of the diagnosis.[4]
Evaluation
Long-leg anteroposterior radiographs are used for screening and measuring varus in the early stages. Proper measurement can be done only when the radiograph projects from hip to ankle bilaterally.
On X-ray evaluation of tibia Blount disease is suspected in the pediatric population if varus focused at proximal tibia with asymmetric bowing with sharp angular deformity and metaphyseal breaking:
- Medial and posterior sloping of proximal tibial epiphysis: physeal deformity is more severe in infantile variety. This variant is associated with compensatory distal femur deformity. In the adolescent variant, it is associated with less severe physeal abnormality and compensatory distal femur, distal tibia deformities. Spontaneous regression is seen up to stage IV in the infantile form.
Metaphyseal-diaphyseal Angle (Drennan)[5][6]
- This angle is between the line connecting metaphyseal beaks and a line perpendicular to the longitudinal axis of the tibia. Greater than 16° is considered abnormal and has a 95% chance of progression. Drennan angles between 11-16° necessitate close observation for the progression of tibia vara. Angles <10° has a 95% chance of natural resolution of the bowing.
- The angular abnormalities include intra- and extra-articular varus malalignment, internal tibial rotation, procurvatum, distal tibial valgus, lateral and medial laxity, and distal femoral deformities.
MRI evaluates cartilage, menisci, ligaments, and vascularity of physis effectively. MRI detects cartilaginous changes effectively compared to radiographs. That's why it is more accurate than radiograph in measuring the slope as the main pathological lesion is tibial cartilage at epiphysis.[7] Thus, gadolinium-enhanced MRI is particularly helpful in neglected or delayed forms seen after four years of age but before the development of radiographic epiphysiodesis. Conservative treatment of the growth plate is a rational option when the MRI shows a homogeneous vascular supply with no signal abnormalities at the growth plate. Patients with uncontrolled obesity, progressive varus malalignment, and MRI evidence of impaired growth plate vascularity invariably progress to asymmetrical epiphysiodesis.
Treatment / Management
The treatment of Blount's disease depends upon the age of the child and the severity of the deformity.
Brace
Bracing used generally extended from the upper thigh to the foot and applied valgus force to the knee. Commonly, KAFO is used. Orthotic treatment may be useful when started before three years of age in non-obese children who wear the brace chiefly at night. The treatment should be continued for one year. However, even with orthotic treatment, osteotomy must be performed before four years of age when indicated. The available level of evidence is not sufficient to support the efficacy of orthotic treatment. An important limitation of this treatment is that braces are complicated to impose on boisterous obese children younger than three years of age.[8] In patients with progressive early-onset Blount disease, surgical axis re-alignment before four years of age ensures a full recovery in 80% of cases. Lateral thrust upon weight-bearing is a characteristic sign that marks the onset of mechanical knee failure.
Graded Growth
Hemiepiphysiodesis of the lateral epiphysis with staples, pin, tension band plating is commonly used procedures. A minimum of 4 years of growth should be there to make this procedure successful. According to the Hueter-Volkmann principle, compression inhibits longitudinal growth. This forms the basis of this type of treatment modality.
Osteotomy
Re-alignment osteotomy is usually performed before four years of age in patients with documented and progressive Blount disease (FDF stage 1) who exhibit risk factors.[9] Proximal tibia/fibula osteotomy, with goals of correction including overcorrection to valgus not indicated (as is the case in infantile Blount) and striving for neutral mechanical axis. Two techniques are utilized, a) high tibial osteotomy with rigid internal fixation and the osteotomy with external fixation and gradual correction; b) high tibial osteotomy with rigid internal fixation, with the closing wedge, opening wedge, dome, serrated and inclined osteotomies.
There are also a variety of fixation devices, including cast, pins and wires, screws, plates, and screws. Along with varus distal fragment is fixed in translation and external rotation to correct external rotation deformity. Other associated surgical procedures such as bar resection and medial plateau elevation should be done in the same sitting along with osteotomy. If the bar is more than 50% area, hemiepiphysiodesis should be done. The level of osteotomy should be below tibial tuberosity to avoid patella Baja leading to extensor insufficiency and knee pain. Any child more than three years irrespective of the stage, stage III patients irrespective of age are ideal candidates of osteotomy.in adolescent variant, and the osteotomy is the only available treatment.
Post-operatively, the patient should be limited weight-bearing with use of crutches for 6-8 weeks. The pros of this approach are that this results in an immediate correction, with cons that there is potential for neurologic injury due to acute lengthening and potential for the development of compartment syndrome. Another common technique is the osteotomy with external fixation and gradual correction. First, an osteotomy is performed, with the connection of the frame that allows for progressive correction. The Taylor Spatial Frame or Ilizarov ring external fixator is commonly used. Post-operatively, 12 to 18 weeks of treatment are needed. The pros of this approach are that this enables gradual correction, which limits the risk of neurovascular compromise and the risk of compartment syndrome with the high tibial osteotomy approach. Furthermore, it allows for the correction of deformity in all planes. Limitations of the method are pin site infection, which may develop as well as the duration of treatment is prolonged.
Differential Diagnosis
Rickets, skeletal dysplasia due to secondary causes such as osteoarthritis, and asymmetric growth are common differential diagnoses. Persistent physiological varus, metaphyseal dysostosis, focal fibrocartilaginous defects, thrombocytopenia, absent radius, and proximal tibia physeal injury (resulting from previous radiation, infection, trauma) may present with similar clinical findings.[10][11] Asymmetrical beaking and sharp angular deformities are commonly seen in Blount's disease, which is unlikely in rickets.
Staging
Staging is done only for infantile form, not adolescent form. Langenskiold classified disease into VI stages with increasing severity and medial physeal collapse. Physeal bar is present from stage V onwards. Catonn and Laville simplified classification later; it was also modified. Recently MRI based classifications are also in use. Fort-de-France (FDF) is a commonly used MRI based classification, but X ray-based classification is most widely used.[12]
Prognosis
The prognosis for Blount's disease varies greatly between the infantile and adolescent forms. The infantile Blount disease has a good prognosis, and deformity recurrence rates are low when the condition is treated at an early stage. Without therapy, the disease has progressive characteristics. Partial or complete regression is possible in early adequately treated forms, while the advanced forms untreated can worsen in the varus deformity over time. These patients may eventually develop significant joint misalignments.[13]
Complications
As the infantile variety is a severe one, it progresses into permanent deformity if it left unattended at its early stages. So early diagnosis is a must for this type of variant. Adolescent variety also causes deformities but less severe compared to the infantile variant.
Proper fit of the brace should be checked periodically as older braces tighten with increasing age leading to superficial skin abrasions and pain. Osteotomy related complications like compartment syndrome will occur. Alternation in extensor mechanism functions will occur if osteotomy is done above the tibial tuberosity level. Residual deformity persists, or recurrence of deformity occurs if overcorrection of deformity is not done as medial physeal growth still persists.
Enhancing Healthcare Team Outcomes
Managing a pediatric lower limb deformity demands a lot more than orthopedic services. Residents should get exposed to pediatric orthopedic clinics, and proper training should be given by faculty in identifying significant risk factors like obesity, radiological features like asymmetrical beaking, which differentiates from metabolic disorders like rickets. Physical medicine and rehabilitation professionals, also with orthotics teaming up with an orthopedic surgeon for effective and timely patient care. In cases of infantile Blount's disease requiring a brace. Orthotists should take measurements for KAFO (knee ankle foot orthosis) in the outpatient department itself. By the time brace will be ready, rehabilitation protocols were discussed with PMR (physical medicine and rehabilitation) regarding materials to be used, pressure pads, hinges placement.[8]