Physiology, Body Mass Index
- Article Author:
- Asia Zierle-Ghosh
- Article Editor:
- Arif Jan
- Updated:
- 7/26/2020 7:05:44 PM
- For CME on this topic:
- Physiology, Body Mass Index CME
- PubMed Link:
- Physiology, Body Mass Index
Introduction
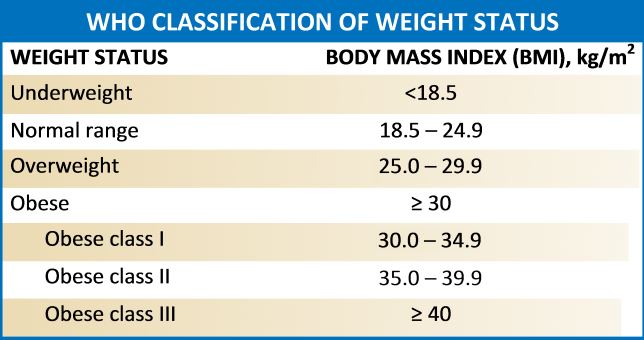
Body mass index (BMI) is a quotient that has been in use since the mid-19th century. It is used to identify adults and adolescents that have an abnormal weight in proportion to their height. It is the calculation of weight divided by height, and it is universally expressed in kg/m2.[1]
It is important for a clinician to understand BMI due to the extensive research that is being done correlating BMI to various disease pathophysiology, and because of its use as stratification measure in many clinical treatment guidelines.[1]
Issues of Concern
Body mass index has been a useful tool due to its universal acceptance as a categorizing factor of body fatness. BMI is considered to be an indication of the relative amount of body fat on an individual's frame. Since it does not measure adipose tissue, it has the potential for inaccuracy. People with significant lean body mass, for example, could be classified as “overweight” while they would likely have a low body fat percentage. You will see this in bodybuilders and other athletes. In these cases, other anthropometric measurements may offer more clinical relevance.
Another caveat is that the physical distribution of adipose tissue has been shown in many studies to affect morbidity and mortality. BMI has no way to account for this variable. In the calculation, height is squared to reduce the contribution of leg length in taller people. This was done because the majority of mass remains within the trunk. However, with this normalization, the equation distributes equal mass to each level of height. This does subtract from the utility of BMI in studies that differentiate body types.[1]
Even with these weaknesses, BMI is an excellent tool that is easy to work with, and useful in most patient populations.
Cellular
BMI is a gross measurement of body fat. Can it have an effect at the cellular level? Literature shows that it does. These studies show associations between BMI and cancer growth at a cellular level, as well as association with other disease states. However, there is data showing that an increased BMI may also be protective.
Clinicians know that increased BMI influences numerous disease states. Current research is being done to define the pathophysiology of such conditions. Bellows et al. worked on the association of BMI on progenitor cells in the article, Influence of BMI on Level of Circulating Progenitor Cells. The study evaluated the level of mesenchymal stromal progenitor cells and circulating progenitor cells in healthy participants with a BMI less than 30 and in healthy participants with a BMI greater than 30. They found a 5-fold increase in the circulating progenitor cells in the group with the larger BMI. This study was done to elaborate on other studies that showed an increase in white blood cells and associations with neoplasms in obese populations. Progenitor cells are needed for a favorable tumor environment. Tumors require angiogenesis and vasculogenesis to progress. When white adipose tissue mobilizes progenitor cells, they are then recruited by the tumor to support the growth of cancer. Colorectal cancer has been commonly used to study this phenomenon.[2]
Many studies have also shown a link between increased BMI and insulin resistance. One example is the study Body Mass Index a Better Predictor of Insulin Resistance than Waist Circumference in Normoglycemics, Preethi Et al. conducted a study with healthy men aged 18 to 25. Their measurements were taken for BMI and waist-hip circumference ratio. The participants were then given a 2-hour glucose test. As the study title indicates, BMI had a statistically significant higher correlation with insulin resistance.[3] At the cellular level, an increase in BMI is likely going to increase stored energy and adipocytes. With 10 kilograms of weight excess, there is a 10% to 30% increase in beta cell mass.[4] With this increase in beta cell mass, insulin secretion increases. Insulin secretion increases directly with an increase in BMI. Tissue cells then down-regulate their insulin receptors which lead to insulin resistance. This is the precursor to diabetes and the basis of the association of obesity with diabetes. This is not an irreversible change. Long-term weight loss is linearly related to insulin action as well.
As mentioned before, an increased BMI is detrimental, but not in every aspect. BMI is usually indicative of more adipose tissue. Adipocytes produce the hormone leptin. This is the hormone that allows the body to spend its energy. It has been shown to have a strong association with memory formation, and there is a higher incidence of leptin receptors within the hippocampus than other parts of the brain. Specifically, some studies have shown that it can reduce deposition of amyloid-beta and tau proteins in neuronal cells when peripheral leptin is high. This is also one of the many contributing factors to the learning disabilities in underweight children. However, higher levels of peripheral leptin also promote a pro-inflammatory environment. Researchers are further investigation correlation this as a link between obesity and disease states like rheumatoid arthritis and fibromyalgia.[5][6]
Overall, at the cellular level, an increase or decrease in BMI can have a significant effect on physiology. Research has shown associations with BMI to insulin resistant states, inflammatory states, and cognition.
Development
Adolphe Quetelet is responsible for the development of BMI. He was a mathematician, statistician, and worked in sociology as well. Quetelet was searching for a way to relate an individual’s height to their ideal weight, as a tool for studying populations. The quotient was first cited in 1972 in the Journal of Chronic Diseases. The article discussed BMI as useful in population studies, or "social physics," as Quetelet called them. It was specifically mentioned that this measurement was not useful to study an individual. However, due to the simplicity of the equation, it remains the most commonly used anthropometric analysis.
Other anthropometric assessments require measurements of an individual’s body. These numbers are less reliable than BMI because they can change depending on the location where the measurement is done. BMI relies on the accuracy of the scale that an individual is weighed on, and can be comparatively referred to as an objective evaluation. It is for these reasons that a quotient developed in the mid-1800s is so widely utilized in the 21st century.[7]
Organ Systems Involved
As mentioned in the cellular discussion, a change in BMI effects nearly all organ systems. We have already elaborated on the effects of BMI, the hormones secreted by adipose tissue, and the links with neurology.
Cardiovascular disease has a known association with increased BMI. It is well known that increased BMI is associated with hypertension, hyperlipidemia, and diabetes, which are all risk factor for coronary heart disease.[8]
In the respiratory system, an increase in BMI is most commonly associated with obesity hypoventilation system. The intra-abdominal pressure, and the actual weight of the mass on the ventral side of the body inhibits the physiologic movements of the lungs. This causes people to feel short of breath, take shorter quicker breaths, and increases the incidence of atelectasis. An increase in BMI is also known to be correlated with obstructive sleep apnea (OSA). OSA can then lead to pulmonary hypertension, cause abnormal heart rhythms, and lead to excessive fatigue.[8]
In the gastrointestinal (GI) system, an increase in BMI has been associated with gastro-esophageal reflux disease (GERD), hepatic disease, cholecystic disease, and colon cancer. The association with colon cancer has been discussed above. Abdominal pressure is directly related to the mass in the abdomen. The increase in abdominal pressure pushes against the cardiac sphincter in the stomach, and allows gastric contents to be regurgitated into the esophagus. This is why, as clinicians, it is important to advise patient with persistent acid reflux to try to lose weight.[9]
Hepatic disease has also been shown to be linked with obesity. Fatty deposition within the liver, known as non-alcoholic steatohepatitis, is one of the leading cause of liver failure in the United States. The accumulation of fat within the liver causes inflammation, injury, and then scarring. This type of scarring is as detrimental as alcoholic cirrhosis.[9]
The endocrine system is affected by increased BMI as mentioned above with insulin resistance and leptin pathways. In the case of this system, the endocrine hormones usually have more commonly known effects on obesity than vice versa. Thyroid hormones control metabolism. The stress hormone, cortisol, causes more energy storage, and breakdown of muscle mass.
A larger than normal BMI causes effects on the integumentary system as well. The increase in adipose tissue increases inflammation within the dermis. This is associated with the immune-mediated hidradenitis suppurativa. Through the proinflammatory state, it has also been linked with psoriasis. On the other end of the spectrum, a lower than normal BMI causes dry, thickened dermis, with less exfoliation, and fine hair growth known as lanugo.[10]
In the genitourinary system, a lower BMI can be more detrimental than a high BMI. Underweight is defined as a BMI less than 18 kg/m2. In this population, the occurrence of acute kidney injury is higher than in the general, healthy population. This is likely due to the nature of the development of this disease, with excessive food/drink restriction, purging, and use of laxatives. All of the listed items can lead to dehydration and pre-renal injury. The electrolyte abnormalities that accompany these same behaviors can lead to nephrolithiasis, and post renal injury. Hypokalemia and hypovolemia have been named as 2 of the most significant contributors to chronic kidney disease. These changes can sometimes be irreversible if they go untreated.[11][12]
Increasing BMI has been directly related to decreasing reproductive function. The current literature has demonstrated a higher incidence of anovulation/subfertility in young women with BMIs greater than 30 kg/m2. Obesity has also been shown to have a strong influence on reproductive cancers including neoplasms of the breast, prostate, endometrial lining, and ovarian. The mechanism of these effects is not known. We do know that adipose tissue is a metabolizer of sex steroids and glucocorticoids. This could be a potential connection between obesity and reproductive dysfunction. Emerging data is also considering the oxidative stress of the inflammatory state caused by obesity on epigenetics. More research will need to be conducted to draw solid conclusions.[11]
Function
The function of body mass index is to identify people of abnormal body mass. Clinically, the measurement is used to screen people for an excess of adipose tissue. Again, this does not directly measure adipose tissue. When people are identified with abnormal proportions, they can then be further classified based on their BMI.
Mechanism
Body mass index is a calculation. The mechanism of this measurement is done by obtaining an individual’s weight in kilograms and dividing that number by their height in meters squared. The resulting unit is kg/m2.
Related Testing
When individuals are identified as an abnormal weight, certain testing should be done. For people with a BMI greater than 30 kg/m2, a lipid panel, thyroid level, and diabetes screening should always be done. These patients should be counseled about a healthy diet and exercise. For people with a BMI less than 18 kg/m2, thyroid level, comprehensive metabolic panel, psychiatric screening for an eating disorder, and conditions of malabsorption should be assessed. These tests are considered standards of care in the American Diabetes Association Diabetes Care annual update. If their weight loss was rapid and unintentional, a cancer workup should also be done.
Pathophysiology
The pathophysiology of BMI was initially thought to be based on the environment. The prevalence has increased, especially in urban areas in the western world. These regions are known for serving large portions of high-calorie food. Whenever the body is ingesting more calories that it is spending, storage pathways will be activated. These pathways lead to more adipose tissue, which then alters your proportions of weight to height. The same goes for regions where there is not enough food to support the population. The body would then ingest fewer calories that it is spending, and catabolic pathways would be activated. This would include the breakdown of adipose and muscle tissue, and again alter the height to weight proportions of the individual. This was the only popular theory about changes in BMI until twin, adoption, and family studies were pursued.
Studies looking at the heredity of BMI showed a strong relationship. This lead to further evaluation with large population genetic screening tools, to isolate genes that are associated with BMI and with obesity specifically. Heymsfield et al., reports in the New England Journal of Medicine that eleven monogenic forms of obesity are now recognized. These include disruptions in leptin and melanocortin-4 receptor gene, which are vital in energy homeostasis. See media image for a summary.
This means that abnormal BMI, as a majority of other chronic conditions, is the result of environmental and genetic factors working hand-in-hand. Further research is being done to identify more genes associated with abnormal BMI. As literature comes out with answers about the genetic factors, pharmaceutical interests are pursuing medications to treat these genetic disruptions in energy homeostasis. Throughout the 19th and most of the 20th centuries, infectious diseases were the most significant life-threatening pathologies. At that time, the development of antibiotics was our main focus. In the late 20th and the 21st century, the focus has shifted to chronic diseases. Since this is a relatively new area of investigation, there are still a lot of answers to be discovered.[13]
Clinical Significance
As mentioned above, BMI is extremely clinically relevant. Patients should be screened for an abnormal BMI at each appointment. This is done at most clinics as part of their vital signs. For the primary care provider, an accurate BMI can help to guide your care with regards to cholesterol workup and management, diabetes screening, thyroid screening, diet/exercise counseling, and so much more. A sudden, unintentional, drop in BMI can alert the provider for more thorough cancer screenings, concern for an eating disorder, or concern for malabsorption. In other practice settings, such as surgical clinics, BMI is taken into consideration for calculating the risk of soft tissue infections and recovery time. It is important to know your patient's BMI, if it is abnormal, and what to do next.
Clinical Pearls:
- BMI < 18kg/m2 is underweight
- BMI 19-24.9 kg/m2 is normal
- BMI 25 - 29.9kg/m2 is overweight.
- BMI 30 - 34.9 kg/m2 is class I obesity
- BMI 35 - 39.9 kg/m2 is class II obesity
- BMI 40 kg/m2 and above is Class III obesity
In the primary care setting, people should be screened for hyperlipidemia, hypothyroidism, and diabetes when they are BMI 25kg/m2 or above. They should also be counseled on diet and a exercise plans to help them lose their excess weight, and reduce their risk for co-morbidities.
Treat the patient and not the number. If your patient seems to have a higher than average muscle content, it may be worth it to measure body fat percentage and not treat on the basis of BMI.