Bowel Adhesions
- Article Author:
- Nick Welle
- Article Author:
- Hussain Sajjad
- Article Author:
- Ayesha Maryam
- Article Editor:
- Bracken Burns
- Updated:
- 7/17/2020 7:08:32 AM
- For CME on this topic:
- Bowel Adhesions CME
- PubMed Link:
- Bowel Adhesions
Introduction
Bowel adhesions are irregular bands of scar tissue that form between two structures that are normally not bound together. The bands of tissue can develop when the body is healing from any disturbance of the tissue that occurs secondary to surgery, infection, trauma, or radiation. While the abdominal adhesions that form are a normal response to the injury of the peritoneal surface, they are the cause of significant morbidity, including adhesive small bowel obstruction (ASBO), infertility in females, chronic abdominal pain, and create a difficult environment for future surgeries.[1][2][3][4] Complications of subsequent surgery when adhesions are present may include: difficult abdominal access and distorted anatomy, inability to safely perform laparoscopic surgery, inadvertent injury to the small bowel, bladder, or ureters, increased duration of surgery, and increased blood loss.
Etiology
The most likely source of abdominal adhesions in the Western world is prior abdominal surgery. The surgeries most likely associated with adhesive small bowel obstruction are open gynecologic procedures, the formation of the ileal pouch-anal anastomosis, and lastly, open colectomy. Other causes of adhesions include (but not limited to) trauma, diverticulitis, Crohn disease, ventriculoperitoneal shunt (VP) shunt, peritonitis (e.g., tuberculous peritonitis), pelvic inflammatory disease, and abdominal or pelvic radiation. Congenital conditions such as malrotation may also be associated with adhesions known as Ladd bands.
Epidemiology
Adhesions account for approximately one percent of all general surgical admissions and three percent of all laparotomies. It is estimated to cost the United States over $2 billion annually in the management of adhesion-related complications. Medical malpractice claims from cases involving adhesions most likely arise due to failure to warn patients during the consenting process of possible visceral injuries, failure to use specific preventative measures, and failure to diagnose or delayed diagnosis of complications.
Pathophysiology
When the peritoneal surface is injured during surgery or a traumatic event, a repair response is initiated. The formation of adhesions involves a complex interaction of cytokines and growth factors secreted by cells near the area of injury. The response to injury begins immediately with hemostasis and coagulation, which release several chemical messengers. The most abundant messenger cells are the leukocytes, specifically the macrophage, and mesothelial cells. [5][6] Macrophages send a signal that will attract new mesothelial cells that re-epithelialize the entire injured peritoneal surface (as opposed to traditional wound healing that heals from edge to edge). This response goes through an immediate inflammatory phase peaking on day four to five. The presence of adhesions is dependent mainly on the balance of fibrin deposition to degradation (fibrinolysis).
A fibrin gel matrix is necessary for the formation of adhesions. Several enzyme systems work to break apart fibrin in the peritoneum that is protective against adhesions, such as tissue plasminogen activator (tPA), that can remove the fibrin gel matrix and subsequently reduce the incidence of adhesions. The extent of fibrinolysis and contact of damaged surfaces are key events in the determination of the extent of adhesion formation. Incomplete fibrinolysis and poor resorption of degradation products allow connective tissue scarring and adhesions to develop, ultimately allowing ingrowth of fibroblasts, capillaries, and nerves.
History and Physical
The majority of patients having bowel adhesions are asymptomatic. Approximately 75% of all patients presenting with symptoms related to adhesive disease have a history of prior abdominal surgery. The remaining 25% have a history of intra-abdominal or pelvic inflammatory processes. Symptomatic patients typically manifest as intestinal obstruction (complete or partial), chronic pain, and infertility in females.
- Adhesions are responsible for most cases of intestinal obstruction in Western countries. Any patient with prior abdominal or pelvic surgery presenting with obstruction should be suspected of having bowel adhesions. Most commonly, these patients describe nausea, vomiting, cramping, and obstipation. Periumbilical pain with cramping every 4 or 5 minutes is typical. More focal pain may indicate peritoneal irritation. Sudden onset of severe pain may suggest acute intestinal ischemia and possible perforation. The physical exam may demonstrate a dehydrated patient, has a distended abdomen, and variations to bowel sound on auscultation. These can be high-pitched tinkling or absent sounds depending on whether or not the bowel is distended with air or fluid.
- Chronic abdominal pain or pelvic pain can be attributed to adhesions. While this relationship is poorly understood, there is evidence that extensive adhesions may limit the natural mobility of organs resulting in visceral pain.
- Adhesions can be a source of infertility in females. Interference with ovum capture and transport or from tubal or intrauterine adhesions can hinder sperm transport and embryo implantation.
For any patient with suspicion of symptoms related to adhesions, a complete physical evaluation of the abdomen should be performed. Symptoms of obstruction and certainly of peritonitis should prompt surgical consultation.
Evaluation
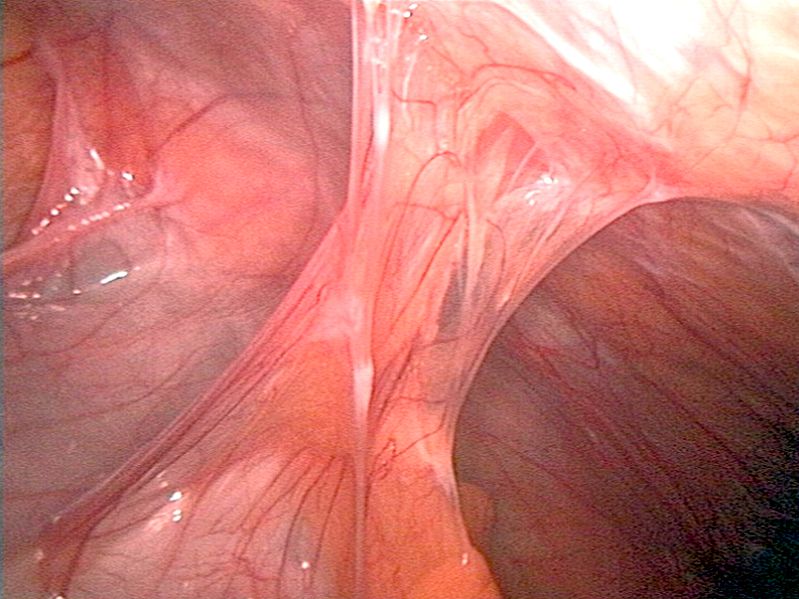
Typically, an adhesion diagnosis is made when clinical suspicion and a detailed history indicate prior risk factors. Direct examination of the abdomen in the form of laparoscopy or laparotomy is the only direct way to confirm the diagnosis of adhesions. Imaging such as plain films, ultrasound, magnetic resonance, computed tomography, and small bowel contrast study can be used; however, these are less reliable than direct visualization for identifying bowel adhesions causing obstruction but can be of value in making the diagnosis of obstruction. [7][8] Signs such as the "fat-bridging sign," a cord-like formation that contains mesenteric fat forms a connection across the peritoneum; twisting or whirling of the mesentery (whirl sign); and anchoring of the omentum are specific signs of obstruction that can be seen in patients presenting with obstruction from adhesions.
The typical laboratory evaluation includes a complete blood count (CBC), complete metabolic panel (CMP), and lactic acid. Although these are non-specific, they may help indicate severity. Arterial blood gas (ABG) and blood cultures should be considered in those with systemic signs, including fever, tachycardia, hypotension, and altered mental status. Metabolic alkalosis is often seen secondary to vomiting, but also, metabolic acidosis may be seen as secondary to bowel ischemia.
Treatment / Management
Most of the treatment is centered around the manifestations of the symptoms, such as bowel obstruction secondary to adhesions. The initial treatment of these patients includes intravenous fluid resuscitation and electrolyte replacement. Nasogastric decompression may also be of benefit. A surgical consult should also be obtained for possible surgery (adhesiolysis) if necessary. Oral intake should be minimized in outpatient situations, and those requiring hospitalization should have nothing by mouth. Often nasogastric tube placement is necessary for bowel decompression and the management of nausea and vomiting. Pain control is done with intravenous pain medications. However, unrelenting pain is often an indication for surgery. Further indications for surgical intervention include complete bowel obstruction, closed-loop obstruction, ischemia, necrosis, or perforation of the bowel wall. These complications of obstruction are based on clinical and radiological examination and should be taken to the operating room for abdominal exploration in a timely fashion if warranted. [9][10][11] Patients with peritonitis should have a prompt surgical consultation. Patients with more of a chronic disease process such as Crohn disease presenting with mechanical obstruction may be observed and at times, followed as an outpatient.
Definitive management for bowel adhesions causing symptoms is laparoscopy or laparotomy with adhesiolysis. As mentioned previously, these procedures are not without risks, and full disclosure of risks vs. benefit should be undertaken with the patient/family when feasible.
Differential Diagnosis
- Acute cholangitis
- Acute Cholecystitis and Biliary colic
- Alcoholic ketoacidosis
- Constipation
- Diverticulitis
- Dysmenorrhea
- Early pregnancy loss
- Endometriosis
- Gallstones
- Inflammatory bowel disease
Pearls and Other Issues
An area of research and a vast field for improvement includes the prevention of peritoneal adhesions. While pharmacologic methods have not been approved for use, the focus has been placed on the barrier agents to prevent adhesions and the technique of the surgeon. The fundamentals behind prevention include minimizing injury, creating a barrier between injured surfaces, preventing excessive coagulation of the serous exudate, removing or dissolving deposited fibrin, minimizing fibroblastic response to tissue injury, enhance recombinant tissue plasminogen activator and novel fibrinolytic.
Surgical techniques include:
- Gentle tissue handling: meticulous hemostasis and gentle, minimal tissue handling are paramount. Preventing serosal injury by minimizing trauma, excess bleeding, and ischemia, and keeping the surgical field moist is recommended.
- Laparotomy sponges are abrasive and should be avoided. When abdominal or pelvic packing is required, place laparotomy sponges in sterile plastic bags or drapes to minimize tissue injury and adhesion formation.
- Preventing foreign body reaction to excess suture, lint, or talc minimizes fibrin deposition. Silk sutures should be avoided as they are fibrogenic.
- Adhesion occurrence is similar regardless of the closure of the peritoneum after laparotomy.
- Laparoscopic surgery minimizes tissue handling and creates smaller abdominal incisions, both of which minimize bowel adhesions. However, this does not guarantee the prevention of adhesions; and longer surgery time and higher insufflation pressure can increase the risk of adhesions.
Enhancing Healthcare Team Outcomes
The prevention of adhesions includes the coordination of care by the interprofessional team that includes nurses, a general surgeon, and anesthesiologist. Prompt recognition of the bowel adhesions by emergency department staff, gastroenterologists, and surgeons can mitigate complications. One of the causes of bowel obstruction is adhesions. While, in some cases, the bowel obstruction caused by adhesions may spontaneously resolve, some patients may require surgery to lyse the adhesions. Operating room nurses should assist surgeons using the measures described above. Emergency and perianesthesia nurses provide initial and postoperative care, reporting changes in condition to the surgeon. They also assist patient and family education. Pharmacists review medications prescribed and assess for drug-drug interactions.
Unfortunately, recurrences are common, and some patients may require repeat adhesiolysis. [8][Level 5]