Approach New Breast Mass
- Article Author:
- Catriona Daly
- Article Editor:
- Yana Puckett
- Updated:
- 8/2/2020 4:25:18 PM
- For CME on this topic:
- Approach New Breast Mass CME
- PubMed Link:
- Approach New Breast Mass
Introduction
Breast lumps or masses are very common, particularly among women of reproductive age. Over 25% of women are affected by breast disease in their lifetime, and the vast majority of these cases will present initially as a new breast mass in the primary care setting. Breast masses have a wide range of causes, from physiological adenosis to highly aggressive malignancy. Although the majority of breast masses present in adult women, children and men can also be affected. Indeed, male breast cancer is a well-documented condition and requires a considered index of suspicion for its timely diagnosis and intervention.[1][2]
Breast cancer is the most common type of cancer in women worldwide, with an incidence of approximately 12%, and therefore although the vast majority of breast lumps are benign, a thorough and structured approach is required in all cases. In general, the approach should follow the triple-assessment pathway of clinical examination, radiological imaging, and pathology analysis. Such an approach will be described in this article, with examples throughout of the common breast pathologies encountered.[3][4]
Function
Anatomy
The breast, or mammary gland, is a modified sweat gland containing various proportions of fibrous tissue, glandular tissue, and adipose tissue. Each breast has 15 to 20 lobes, which are drained by lactiferous ducts that converge beneath the nipple in the subareolar region. The lobes are supported by fibrous stroma and fatty stroma. Lymphatic drainage is primarily through the axillary lymph nodes, but can also involve the pectoral, subscapular and internal mammary nodes.[5]
Breast tissue is present in children and males but is more developed in females of reproductive age due to hormonal surges that arise at puberty. Breast tissues involute significantly following the menopause, the glandular tissue atrophies due to the reduction of circulating estrogen levels and is largely replaced by fatty tissue. Breast tissues, and indeed the majority of breast pathologies, are responsive to changes in hormone levels.[5]
History
A thorough and accurate history is the cornerstone of approaching any new breast mass.[6] Particular emphasis should be placed on the chronological development of the lump and symptoms associated with it.
Timing
It is not always possible to establish the duration for which the mass has been present. Patients who do not regularly carry out breast self-examination may take longer to notice a breast lump, and indeed a proportion of breast lumps are identified through routine screening, so this is not necessarily an accurate way of determining acuity of such a mass.[7] More important is to establish whether the mass had developed in association with trauma or other symptoms and how rapidly the mass appears to be growing or changing, if at all
Associated Symptoms
Localized:
An acutely tender breast lump is more likely to be an abscess or hematoma secondary to trauma. Cancerous breast masses rarely present with pain, although the presence of pain should not exclude neoplastic lesions from the differential. Nipple changes or discharge merits attention, as these can correlate with some less common breast tumors, as well as changes to the overlying skin, including ulceration, eczema, or tethering.[7][8]
Systemic:
As is the case with every new patient assessment, a careful systems review should take place to seek evidence of disseminated disease. History of weight loss, dyspnoea, and bone pain are important in highlighting potential sites of metastasis.[9]
Family History
Family history would be one of the key risk factors for breast cancer, particularly if family members were young (>50) at the age of diagnosis. Establishing an accurate family history is crucial, and it should also include relatives diagnosed with non-breast cancers, especially if at a young age. Detailed family history can be highly useful in generating an accurate risk profile.[10]
Risk Factors
The primary risk factor for developing breast cancer is excess exposure to estrogens. Therefore, it is essential to interrogate lifetime estrogen exposure in all patients presenting with a new breast mass. Early age of menarche, late age of first pregnancy, nulliparity, oral contraceptive or hormone replacement therapy, and late menopause increase estrogen exposure, while breastfeeding is a protective factor.[8] Male patients should be asked about previous hormonal treatments for prostate cancer, the use of finasteride or testosterone, episodes of orchitis/epididymitis, or previously diagnosed Klinefelter syndrome.[11] Other risk factors, such as excess alcohol intake and obesity, are thought to increase endogenous estrogens.[12]
Medical History
A detailed understanding of the patient's medical history and medications is crucial in the initial work-up of any new patient. A patient who is taking oral contraceptive medication, hormone replacement therapy, corticosteroids, or other steroid medication such as spironolactone must understand the implications of these, and a medication review may be necessary before carrying out further investigations.[8]
Triple Assessment
Physical Examination
Clinical examination of a breast lump is the first stage in the triple-assessment approach. Both breasts and axillae should be examined meticulously by the clinician, as well as carrying out a physical examination of other body systems as indicated by the history. Although it can be tempting to bypass the physical examination in favor of other, more targeted investigation modalities such as mammography or sonography, the findings of the physical examination are crucial for effective diagnosis and management of breast disease.[13] Repeated studies have indicated that only by combining all three assessments can optimal sensitivity and specificity be achieved.[4][13]
Clinical breast examination is often conducted with a chaperone present to make the patient feel more comfortable. The entirely of the chest and abdomen should be exposed, Each breast and axilla should undergo a visual inspection, looking for skin changes, nipple discharge, visible masses or asymmetry, and tethering to underlying structure; this feature can be exaggerated by asking the patient to place their hands on their hips or lift the arms.[14]
The breasts can most easily be palpated by asking the patient to lie back at approximately 30 degrees and rest their hand palm-up underneath their head. Palpation of the breast must proceed in a structured manner; generally, clinicians will use a four-quadrant approach (upper outer, upper inner, lower outer, lower inner quadrants), followed by palpating the areola and then the axillary tail. Particular attention should focus on the inframammary fold and the axillary tail. The normal breast is examined first, and the tissue assessed for its overall consistency. Masses are most often detected in the upper outer quadrant, as the majority of breast tissue is located here.
Palpable breast masses should be described in terms of location, size, shape, tenderness, fluctuance, mobility, texture, and pulsatility. If the patient describes nipple discharge that is not immediately visualized, it is appropriate to ask the patient to try to express the discharge themselves before the clinician attempting to do so.[15]
Following palpation of the breast, the clinician must always palpate the axilla and supraclavicular region for lymphadenopathy. This area may present with enlarged, tender, or firm nodes, the number, and nature of which should be documented. During the examination of the axilla, the weight of the patient's arm should be taken by the clinician to relax the pectoralis muscles.[16]
Radiological Assessment
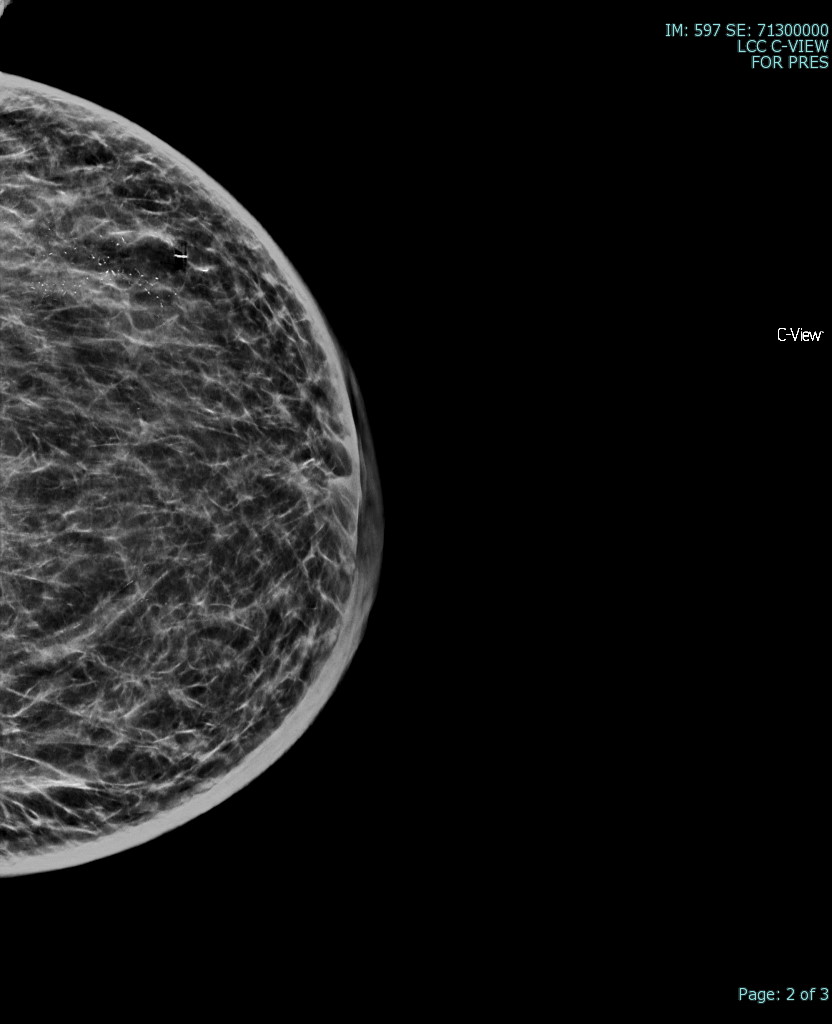
The most common radiological tools for imaging breast tissue are mammography, ultrasound, and occasionally MRI.
Mammography is the first-line imaging for women over the age of 35 who present with a new breast mass. Mammography is also useful for screening of asymptomatic women who fit their regional screening criteria. This process involves obtaining X-ray imaging in both a craniocaudal and mediolateral oblique plane to ensure imaging of all breast tissue. Mammography tends to have higher specificity and lower sensitivity than ultrasound in all cases.[17] Mammography can have negative findings in up to 15% of patients with breast cancer.[18]
Ultrasound imaging is preferred to mammography in younger women and men as their breast tissue tends to be denser, with a much lower proportion of fatty tissue. This dense tissue impedes the accuracy of mammography and makes it more challenging to detect microcalcifications.[17]
MRI can also be useful in the assessment of a new breast lump. It is not routinely used as it is more expensive with longer wait times but shows high sensitivity for detecting and delineating breast masses. It is the preferred modality for patients who have had previous breast augmentation surgery as the breast implants can distort the underlying parenchyma in mammography or ultrasound. It may also be a recommended approach for high-risk patients, such as those with known underlying BRCA mutations.[19]
Imaging reports are standardized using a tool called BIRADS – Breast Imaging Reporting and Data System (fifth edition). This standard allows breast imaging to be described according to a certain structure as follows: density of breast tissue, presence and location of a mass or masses, calcifications, asymmetry, and any associated features.[20] This classification system divides patients into categories 0 to 6, depending on the likelihood of malignancy in the obtained images:
BIRADS 0 – insufficient or incomplete study
BIRADS 1 – normal study
BIRADS 2 – benign features
BIRADS 3 – probably benign (<2% risk of malignancy)
BIRADS 4 – suspicious features (divided into categories 4a, 4b and 4c depending on the likelihood of malignancy)
BIRADS 5 – probably malignant (>95% chance of malignancy)
BIRADS 6 – malignant (proven malignant on tissue biopsy)
The BIRADS system includes different classifications for masses depending on the imaging modality in question. In mammography, to be considered a mass, the lesion must be visible in two different projections, must have convex outer borders, and must be denser in the center than on the periphery.[21] In ultrasound, a mass requires visualization in two different planes. Masses are defined according to their shape, margin, and density. In terms of shape, a mass can categorize as round, oval, or irregular. Circumscribed margins are more apt to be benign, whereas microlobulated, indistinct, or spiculated are more likely to be malignant. The margin may also appear obscured. Mass density is described in comparison to that of the surrounding normal tissues - higher, equal, or lower - or may reflect the presence of fat within the mass.[20]
Pathology Analysis
The third aspect of triple-assessment requires an invasive procedure in order to allow pathological diagnosis. Pathology analysis involves either fine-needle aspiration cytology (FNAC) or core biopsy.[4] Cytology allows an analysis of cells in isolation, while histological examination of a biopsy can provide more detail about the architecture of tissues. Both of these are invasive procedures involving risks to the patient and should, therefore, only take place when the index of suspicion is present. The decision whether to perform FNAC or core biopsy depends on several factors, including the expertise of the clinician, available diagnostic equipment, and site of the lesion. However, FNAC is generally preferred as first-line since it is less invasive.[22]
The need for pathological analysis has undergone review and, in certain cases, is thought to be unnecessary if the physical examination and radiological assessments are negative in a patient of low risk (i.e., young patients under the age of 25).[23] The decision to proceed with FNAC or core biopsy is a clinical one, but in all cases should not be undertaken without due consideration of the risk-benefit analysis.
Many other investigations can be carried out in the analysis of breast masses, depending on the likely differential and the level of resources available.
Baseline blood tests are usually recommended in a patient who is likely to undergo surgery, with particular emphasis on hemoglobin, bone profile, and liver function tests in case of suspected hepatic metastasis. Inflammatory markers and blood cultures should be considered where a breast abscess is suspected. Tumor markers such as Ca27.29 and Ca15-3 can be used for prognostication and monitoring for recurrence.
Nuclear medicine, PET scanning, and bone isotope scanning may help to assess the metastatic disease. Genome-mapping may be an option, for example, if a patient is suspected of carrying the BRCA1 or BRCA2 gene.[8]
Differential Diagnosis
The likely differential of breast masses varies significantly depending on patient demographics.
Generalized enlargement of breast tissue can be as simple as hyperplasia due to hormonal changes to drug-induced. It can even be related to liver pathology or, in some cases, related to muscular hypertrophy as seen in athletes or bodybuilders.
In female patients, the most common cause of a new breast mass is a fibrocystic disease, particularly among premenopausal women between the ages of 35 and 50. Fibrocystic changes, including simple and complex cysts, fibrosis, adenosis, and hyperplasia, are extremely common, affecting more than 50% of women of reproductive age, and are usually asymptomatic.[24][23][24]
A new discrete breast mass in the context of fibrocystic disease is most likely to be a simple cyst, which usually presents as a fluctuant, well-circumscribed, smooth round lesion, which may or not be tender. Breast cysts commonly arise from distended lobules and are filled with serous fluid. These usually require no treatment and tend to go away by themselves. A simple cyst that has been diagnosed with mammography does not require tissue biopsy, but a complex cyst or cyst containing debris should receive further investigation to rule out malignancy. Cysts may be multifocal or bilateral and can be recurrent. In post-menopausal women, the rate of fibrocystic disease increases with the use of hormone replacement therapy.[25]
Breast adenosis describes enlargement and proliferation of the breast glands, and while not normally considered under the umbrella of a discrete breast mass, can present with a generalized 'lumpiness' of the breast, and should be considered as a differential. It is common and often asymptomatic.[26]
Among younger women, fibroadenomas are more common, accounting for over 50% of breast masses in females below the age of 30.[27] A fibroadenoma is a biphasic mass containing a combination of glandular and stromal tissue. These are non-tender, firm, rubbery masses and tend to be highly mobile. Core biopsy is the recommendation if there is any diagnostic uncertainty following imaging.[28] These benign lesions are usually self-limiting; however, surgical treatment may merit consideration if a fibroadenoma is particularly large or causing the patient discomfort or cosmetic issues.
In high-risk women, particularly post-menopausal women or those with a history of high estrogen exposure, the likelihood of a malignant diagnosis is more likely. Malignant breast masses are more prone to be hard, nodular, irregular in shape, and fixed to underlying or overlying tissues. Breast cancer must be considered as a differential in all cases of a new breast mass, and triple assessment is advisable if there is any uncertainty. Breast cancer can be divided into non-invasive and invasive cancers and can be classified according to cell type (e.g., ductal, lobular, tubular) and hormone receptor status. Phyllodes tumors and Paget's disease of the breast are not always malignant but are usually considered in this category as they have a high level of malignant potential and need to be treated as such.[8] Further detail as to the different types of breast cancer and their management is outside the scope of this article. Of note, it is crucial to be aware that not all breast cancers are associated with a palpable mass, and indeed a large proportion is diagnosed via screening of asymptomatic individuals.
In children presenting with discrete breast masses, the vast majority (>95%) are benign fibroadenomas. These usually require no treatment but require close monitoring as there are infrequent reports in the literature of pediatric breast cancers.[29]
Males presenting with breast masses must be treated with a high degree of suspicion to rule out malignant tumors.[2] Imaging of male breasts should utilize ultrasound as male breast tissue is not amenable to mammography. In males, central masses located behind the nipple may be attributable to gynecomastia. Gynecomastia is abnormal breast tissue development in males, which can correlate with several different causes, including chromosomal disorders, liver failure, paraneoplastic syndromes, and drugs such as spironolactone and calcium channel blockers.[30] Of note, physiological gynecomastia may also be present in the neonatal period, at puberty and in elderly males, due to hormonal variations.[31]
Breast masses may arise due to local traumatic or infective etiology.
A new breast mass on the background of recent trauma may represent fat necrosis or hematoma formation. These can arise following direct trauma to the breast or may be associated with surgery, biopsy, or radiation therapy. Fat necrosis is the term that describes the replacement of dead fatty tissue with scar tissue, which can present as a palpable, nodular, and occasionally tender lump due to its contrasting density with the surrounding tissue.[32] A hematoma is a collection of blood under the skin or within the breast tissue, and can also be characterized by scar formation.[33] A hematoma may also be associated with anticoagulant usage, in which case a review of anticoagulation is in order.[34] As these changes can resemble malignancy on imaging, the importance of a clear history must be emphasized to avoid unnecessary and potentially harmful invasive investigations.[32]
A breast abscess is a localized collection of pus, usually arising as a complication of mastitis. Breast abscesses typically appear in association with lactation, as lactating mothers are at a higher risk of bacterial inoculation. The most likely causative organisms are staphylococcus and streptococcus. A breast abscess is likely to be extremely tender, with erythema and induration of the overlying skin.[35]
Treatment
Treatment of a new breast lump depends on whether the lump is benign or malignant, and on the physical health and personal wishes of the patient
Any patient with a proven or suspected malignant mass should receive management with an interprofessional approach, with input from the oncology, radiology, pathology, surgical, specialist nursing, and anesthetic teams, as well as palliative care, social workers, and psychology teams where indicated. Breast cancers are typically treated through a combination of surgery, chemotherapy, radiation therapy, hormone therapy, and immunological therapy.[8] The specific treatments of breast cancer are outside of the scope of this article.
Benign breast masses are treated according to etiology:
- Breast cyst: A simple breast cysts usually involute without any intervention. If persistent or troublesome cyst aspiration may be an option, however, they tend to recur. Cyst aspirate may be sent for cytological analysis, but there is some controversy as to the benefit of this due to the risk of false-positives.[25]
- Fibroadenoma: These lesions are benign and usually involute without requiring any further treatment. However, surgical consultation should be considered if they are large, painful, or causing the patient distress, and these are often removed surgically.[28] If there is diagnostic uncertainty, excision biopsy should take place for diagnostic purposes.
- Fat necrosis, hematoma: This usually does not require any treatment other than analgesia and monitoring. However, the surgical consultant should merit consideration if the mass is causing the patient, significant pain, or cosmetic issues.[32]
- Breast abscess: In general, abscesses require surgical incision and drainage to identify and remove the source of infection. Smaller abscesses less than 3cm in size and lactational abscesses may resolve with oral antibiotics and needle aspiration, but there is a risk of recurrence.[35] In the primary setting, lactational abscesses should have treatment with analgesia and oral antibiotics, and patients should be encouraged to continue breastfeeding if possible, with an onward referral for definitive management. Abscess in a non-lactating patient, or an unresolved, large or multiloculated abscess may require admission for intravenous antibiotics and surgical or radiological drainage, and early breast specialist opinion should be sought in these cases.[36] Abscesses in a non-lactating female requires referral to a triple assessment clinic to rule out underlying inflammatory breast cancer.[35]
- Gynaecomastia: In males presenting with gynecomastia, the investigation should focus on the likely cause, and if none can be found, further referral to endocrinology is recommended.[31]
Clinical Significance
According to the WHO, breast cancer is the leading cause of cancer-related deaths among women worldwide with an estimated lifetime risk of 12%.[3] Benign breast disease is many times more common, affecting between 25% and 50% of adult women and accounting for 3% of GP encounters with female patients.[37] A majority of these cases may present initially with a new breast mass. It is crucial, therefore, for every clinician to have confidence in assessing and managing these patients, and a thorough, consistent approach will enable this. The triple assessment approach discussed in this article has been shown to improve outcomes by allowing timely diagnosis and a coordinated interprofessional approach.[38]
Enhancing Healthcare Team Outcomes
The clinician must always approach a new breast mass from an interprofessional approach as the causes are so diverse, and the investigations and treatments carried out by such a variety of teams. The links between primary care and specialty and subspecialty teams must be clearly defined, with an established protocol for clear and effective communication between the two.
A triple assessment clinic is an excellent example of a multidisciplinary clinic, as physicians or specialist nurses, clinical pathologists and radiographers, sonographers, and radiologists are involved in the process. In this setting, interprofessional communication is not just encouraged but necessary to come to a consensus as to the most likely diagnosis.[4] Treatment of breast cancers can involve an even more extensive range of specialists, including breast and oncoplastic surgeons, oncologists, radiation therapists, immunologists, genetic counselors and nurse specialists who tend to take the lead in coordinating care.[39]
In breast cancer, multidisciplinary or interprofessional care is the gold standard. It has proven to significantly reduce mortality not just from breast cancer but from all causes over a 5-year period.[40] This data demonstrates the importance of enhancing and prioritizing interprofessional relations to improve patient outcomes.
(Click Image to Enlarge)
(Click Image to Enlarge)