
Mid Forehead Brow Lift
- Article Author:
- Bhupendra Patel
- Article Editor:
- Raman Malhotra
- Updated:
- 9/15/2020 10:13:52 AM
- For CME on this topic:
- Mid Forehead Brow Lift CME
- PubMed Link:
- Mid Forehead Brow Lift
Introduction
In most medical conditions, definitions rely upon exact numbers. In the case of brow ptosis, it is judgment combined with measurements. Brow ptosis exists when it interferes with aesthetics or function. The level of brows deemed low in one person may be perfectly acceptable or "normal" in another.
Brows descend over time in everyone. With the brow being a mobile structure and with the secondary effects of age, solar elastosis, muscle action, trauma, lesions, and gravity, some degree of brow descent will occur in everyone. The brow position is regarded differently in different genders, races, ages, and even generations. In some communities, the concept of changing a brow position or curve as we age is considered anathema. In many Western societies, it is an accepted desire. Age-related eyebrow ptosis is secondary to gravitational, involutional, and exposure changes.
In women, brows usually sit above the orbital rim and arch upward and outward so that the peak of the brow is at the lateral limbus, although in some societies, a further lateral flare is even more desirable. Therefore, in women, brow ptosis would is present if the brow is lower than this ideal. Even a brow above the orbital rim may be low (have brow ptosis), and repair or repositioning may be desirable.
In men, eyebrows normally sit at or just above the superior orbital rim, with the brow shape being more horizontal. There is variability in the ideal brow in men and women depending upon age, cultural influences, occupations, and secondary effects of the environment. Therefore, in a weather-worn farmer, a low brow would be considered normal as it would protect the farmer from environmental factors like light, dust, and wind. In an actor, there may not be an ideal brow position as the brow movement would be utilized to show different expressions in that profession. In a lorry driver or train driver, where peripheral vision is vital, the brow position may need to be higher than in other patients, male or female. So unlike say ptosis, where clinicians measure corneal reflex-lid margin distance and levator function and diagnose ptosis numerically, brow ptosis is a subjective assessment based upon many factors.
Brow ptosis is rarely symmetrical because of many factors, including differences between the right and left sides of the face (sometimes with hemifacial microsomia), different exposure to the elements, and the side a patient may sleep on, among others.
Common Causes
- Aging
- Facial palsy
- Tumors
- Trauma
Clinical Presentation
- Cosmetic
- Visual obstruction caused by secondary dermatochalasis
- Asymmetric brow positions
- Irritation caused by secondary lash ptosis
Brow ptosis, in the absence of trauma, paralysis, or disease, occurs slowly, and most patients will not be aware of the brow ptosis until pointed out after a clinical examination. Almost everyone over the age of 40 years, male or female, will have some degree of brow ptosis. Most of these patients will not need surgical correction.
Surgical Procedures
- Direct brow lift
- Mid-forehead brow lift
- Pretrichial brow lift
- Temporal brow lift
- Coronal brow lift
- Endoscopic brow lift
- Internal brow lift
This article reviews the assessment and planning of brow lifts, in general, and indications for the mid-forehead lift, in particular.
Procedure History[1]
Historically, many surgical procedures such as cataract surgeries, nose reconstructions, or skin flaps, have been performed for hundreds of years, and some of these, like cataract surgery, thousands of years. Surprisingly, brow lift surgery was only recorded in the last century when Lexer first discussed and presented the forehead lift in 1910. Subsequently, a coronal incision and resection of tissue were described by Hunt, who did not undermine any of the tissues, which led to limited results. Joseph, in 1931, presented detailed descriptions of a pretrichial brow lift and also incisions made lower on the forehead used to lift the brows. Many surgeons continued simple tissue resection without any undermining of the proximal or distal tissues until Passot improved upon excision of skin behind the hair with temporal facial nerve denervation in 1933. This method would improve the forehead wrinkles; however, the tonic component of the frontalis muscle would be lost and was therefore not a suitable advance to brow lifts. For reasons not exactly clear, surgeons continued to explore nerve destruction. Edwards presented isolated temporal neurectomy as recently as 1957.
A more anatomical approach was presented by Bames in 1957 when he described a direct eyebrow lift. Through this approach, he weakened the corrugator muscles and undermined the forehead all the way up to the hairline, while crosshatching the frontalis muscle.
Modern hairline and coronal approaches (1 cm behind the hairline) to the forehead lift and brow lift were ushered in by Pangman and Wallace in 1961. Further refinement in cosmetic surgery occurred when in 1962, Gonzalez-Ulloa performed the forehead lift by incorporating it into his facelift procedure.
Despite the initial enthusiasm for coronal lifts, reports in the 1960s and 1970s suggested that results of coronal forehead lifts were short-lived, which led to the procedure losing favor. It had not been appreciated that without undermining after excision of a strip and somehow modifying the frontalis muscle, the results were bound to be temporary. So until the early 1970s, most surgical procedures consisted of resection and repair without undermining or manipulation of the forehead muscles. This situation was partly because the anatomy and physiology of the forehead were not adequately appreciated.
A significant advance occurred in the mid-1970s when several surgeons (Skoog, Vinas, Hinderer, Griffiths, Marino, and others) began to manipulate the frontalis muscle, usually by excising a strip of the muscle to eliminate the dynamic lines on the forehead. This technique also allowed better stretching of the superficial tissues. Washio was one of the first to carry out cadaver studies when he noted (1975) that removal of a transverse section of the frontalis muscle resulted in a significant elevation of the forehead. More dramatic surgical innovations by Tessier, LeRoux, and Jones (1974) advocated the complete removal of the frontalis muscle. Not surprisingly, this overtly destructive approach did not endure.
In the 1980s and 1990s, the coronal brow lift became the established approach to brow lifting; this was partly because of the advances made by Tessier and his group in the approach to the skull via subperiosteal approaches. It has been said, not entirely in jest, that the coronal brow lift with the associated loss of hair and sensation and the overly tight look to the forehead and the brows was "a surgical procedure designed by men for use on women."
In the 1990s, endoscopic approaches to brow lifts were developed. After the evolution of fixation techniques, it became apparent that in "brow lifting," brow shaping was more important. Repositioning of the brows and forehead could be controlled with a proper release of the periosteum from the "lateral canthus to the lateral canthus" across the superior orbital rims and the nasal bridge, combined with manipulation of the depressor and elevator muscles of the brows. Anatomical details were studied and understood so that safe approaches could be designed using minimal incision approaches. Understanding the sensory and motor innervation of the forehead and the periorbital tissues allowed more accurate manipulation and modification of the tissues and allowed more limited lifts like the pretrichial lift and the temporal brow lift.
After some debate about the longevity and effectiveness of endoscopic brow lifts when compared to coronal brow lifts, there are now two schools: one school still largely performs coronal brow lifts. However, more and more surgeons are becoming experts at performing endoscopic brow lifts. When patients are chosen correctly, these endoscopic brow lifts are creating reliable and long-lasting results. Coronal brow lifts, pretrichial brow lifts, mid-forehead brow lifts, direct brow lifts, and temporal brow lifts are now performed for specific indications. The so-called internal brow lift should be called a supporting procedure than a proper brow lift. No long-term studies show effective brow lifting, and the design of the procedure does not address the complete arch of the brow, nor the forehead.
The midforehead lift procedure has specific indications, advantages, and limitations. We have found this approach to be useful in males who have heavy brows with overactive frontalis muscles and deep forehead wrinkles. The thicker, more sebaceous skin allows one to hide scars better, although there is some debate about this.
Development of Brow Ptosis
A common refrain in plastic surgery is "I am becoming my mother" or "I look like my dad." What the patient is saying is that family characteristics (bone structure, genetics, among others) are manifesting. The commonest cause of brow ptosis is aging (time and the environment). Everyone has an "aging clock," which is genetically determined, but skin and structures are also affected by environmental factors such as smoking, exposure to ultraviolet (UV) light, health, and diet, among others. It is helpful to examine photographs, not only of the patients when they were younger, but also photographs of their parents.
Patients exposed to the elements (farmers, sportsmen, and women) will show marked overaction of the corrugator, procerus, and frontalis muscles, especially if they have not protected their eyes from sunlight and other harsh environmental factors. The "weathered face," as one describes it, seen in sailors and farmers (and the explorers of the 19th century) shows these changes well, not just in the region of the forehead and the brows but also the lower face and neck. These patients develop marked corrugator and procerus muscle lines, which are the vertical "elevenses" and the horizontal lines at the root of the nose, respectively. The eyebrow heads will appear closer because of the overaction of the corrugator muscles. In these patients, contrary to common teaching, surgeons make an effort to elevate and separate the brow heads when performing a surgical procedure. There will be deep horizontal forehead lines secondary to a constant frontalis overuse. There is also a "fat nose syndrome" appearance that these patients develop, caused by the downward slide of the procerus muscle and the inward movement of the corrugator and procerus muscles. This results (especially apparent in ladies), a widened bridge of the nose with the soft tissues "collapsing" downwards and inward. In these patients, especially when addressing them for cosmetic reasons, it is vital to slim this "fat nose syndrome."
It is always helpful to compare the current appearance of the patient with photographs when the patient was younger to assess the degree to which the brow positions and curves have changed. Sometimes one is surprised to see that the brows have changed very little from their teenage years. Another truism is that the young look good with brows high or low; with age, people look a little better with somewhat higher brows.
Besides the central and medial changes to the brows, lateral brow droop almost always becomes exaggerated because of a lack of support from the frontalis muscle. This anatomical insertion of the frontalis muscle changes as we age. It has recently been shown that the angle of insertion between the frontalis muscle and the orbicularis muscle becomes more acute, thereby leading to further loss of support laterally: this gives the temporal hooding, lash ptosis, and temporal brow droop in such patients, with secondary crow's feet. On occasion, and often in men, one will see an exaggerated temporal brow droop because of the lack of support by the frontalis muscle, with almost an acute change in the curve of the brow, demanding modified approaches to correct the problem.
Clinical Presentation
Presentation of brow ptosis varies from cosmetic complaints of forehead lines, secondary heaviness (hooding) of the upper eyelids, to the presence of frown lines and problems with vision. Patients will only rarely complain that their brows are heavy or droopy. Indeed, unlike many other aging changes of the face, brow ptosis is one condition that is explained to the patient with the help of a mirror as most patients will not be aware of the changes shown.
Cosmetic patients will also mostly focus on the "heavy upper eyelids and excessive upper eyelid fullness." Other complaints may include "looking tired, looking angry or unhappy" either from the patient or from family and colleagues.
History
A thorough preoperative assessment of any surgical patient is vital. Past illnesses, medications, allergies, and any history of unusual scarring are noted. Specific emphasis is placed upon any history of thyroid disease, prior eyelid or brow surgery, unusual scarring tendency, and any tendency to develop unusual edema. Patients with thyroid disease must be controlled and stable, ideally for at least six months. Patients with thyroid disease will have deeper frown lines and may suffer from madarosis of the brow hairs. These patients also tend to develop prolonged edema after any facial surgery.
Examination of Forehead and Eyebrows
We always examine the whole face whenever assessing patients with a complaint of problems with lids, brows, jowls, or neck. Indeed, it is good practice to develop an examination technique and routine, which ensures that you can detect any age-related and other changes which may not be apparent to the patient but need to be discussed. The differences between the right and the left sides of the face are examined for asymmetry; an assessment is made of which side the patient sleeps on, and the presence of any lingering edema (often seen in the malar regions) noted. Sometimes, what a patient sees may not be what you see when you examine the whole face. There have been patients who present for a forehead lift who are better served with blepharoplasty and lower lid and face surgery and vice versa.
Specific Examination of Brow Ptosis
- Assess the hairlines
- Assess the density of scalp hair centrally and temporally
- Measure the height of the forehead (distance between the corneal reflex and the anterior hairline or the distance between the central brow and the anterior hairline.
- Measure the brow position compared to the opposite side
- Measure brow position: there are several ways to do this. The surgeon should develop his/her system that is repeatable. The brow can be measured relative to the superior orbital rim or measured from the lid margin to the brow or from the corneal reflex to the brow centrally and from the medial limbus and the lateral limbus to the brow medially and laterally. Others use the medial and lateral canthi as the reference points.
- Measure the degree of true dermatochalasis as opposed to secondary dermatochalasis caused by the brow ptosis.
- Assess the medial and central fat pads and any lacrimal gland prolapse.
- Assess forehead rhytids
- Assess corrugator and procerus lines
- Assess crow's feet
- Assess any blepharoptosis that may be present
- Basic lower eyelid assessment must always be performed whenever considering brow surgery or upper eyelid surgery (or indeed any facial surgery).
When documenting brow ptosis, one repeatable measurement is the measurement of the distance between the inferior limbus and the center of the brow. Determine if brow ptosis is present: in most patients, this distance will be more than 22 mm. Although a measurement of less than 22 mm will suggest brow ptosis, this will be determined by the many other factors we discussed above: age, gender, occupation, among others.
An ideal brow position is an individual feature best determined by the surgeon and patient. Surgeons customarily review photographs of all patients to determine if an age existed when the brows were located in a position that the patient considers acceptable. Furthermore, brow shape is a more crucial determinant of an aesthetic brow. In other words, position and shape go together.
Dynamic Measurement of Brow Ptosis
With a ruler held medially, centrally, and laterally, the brow is elevated and moved (sometimes more lateral) to assess the degree of brow ptosis. Location is measured in 3 positions, and the difference between the desired brow position and the relaxed brow position indicates the degree of brow ptosis. However, the frontalis will be active to different degrees in different patients and also at different times of the day, making exact measurements difficult.
Brow asymmetry also needs to be assessed and documented. Patients are shown the findings in front of a mirror, as many will be unaware of asymmetry.
Although all discussions concentrate on the brow and the brow height and curve, surgeons must not forget that the forehead is just as important; they should document the severity of glabellar, corrugator, and frontalis lines and also skin changes related to solar elastosis.
The distance between the brow and the anterior hairline needs to be measured because, in some patients, it may be desirable to bring the hairline forward. In these cases, a properly performed pretrichial brow lift will give excellent results. Bear in mind that cultural, racial, gender, and age-related differences make it difficult to provide exact normal measurements.
Every patient seen for or considering a brow lift should have their upper eyelids and lower eyelids assessed. The forehead/brow, upper eyelid, and lower eyelid region are a continuum as procedures performed above the canthus (brows and upper eyelids) may be influenced by lower eyelid changes (laxity, retraction, ectropion). Procedures on the lower eyelids may affect the final appearance of upper eyelids, especially if there is underlying ptosis or dermatochalasis, primary or secondary. Indeed, one may argue that the continuum should be forehead, brows, upper lids, and cheeks. Research has shown that one raises the nasojugal and malar groove (sometimes called the orbital groove), it makes the brows look better even when nothing is done to the brows, which is an interesting and important observation that the serious aesthetic surgeon would do well to study further. Discuss this in the overall assessment of the face in aesthetic patients.
Assessment of the upper eyelid should include the following:
- Corneal reflex-lid margin distance
- Position and presence of upper eyelid skin crease.
- Assess if the patient has primary and secondary skin creases
- Amount of tarsal platform show
- Degree of dermatochalasis: primary and secondary
- Upper-fat herniation medial and central
- Assess lacrimal gland prominence
- Assess upper eyelid skin condition (solar elastosis, vertical wrinkles, vessels showing, among others)
Assessment of the lower eyelid should include the following:
- Medial canthus: Position, laxity, dystopia, scarring, webbing
- Lateral canthus: Position, dystopia, laxity, scarring, webbing
- Lower eyelid distraction test
- Lower eyelid snapback test
- Inferior scleral show
- Presence of medial central and lateral fat pads
- Nasojugal and malar grooves
- Malar angle
- Bell's phenomenon
- Tear film integrity and tear breakup time
- Blink completeness
- Corneal sensation and health
- Hertel measurement of the globe (proptosis or enophthalmos may be present)
A summary of patient evaluation that is specific for forehead and brow elevation is as follows:
- Hair: Density and distribution
- Hairline: Frontal and temporal
- Forehead height relative to facial proportions and racial characteristics
- Forehead height: Eyebrows to anterior scalp hairline
- Forehead transverse rhytids: Distribution and depth
- Forehead temporal rhytides
- Crow's feet
- Skin thickness, quality, and sebaceous quality
- Eyebrow shape and symmetry
- Eyebrow position (degree of medial, central, and lateral ptosis)
- Eyebrow hair distribution: Evidence of plucking, loss, other changes
- Eyebrow mobility: Paralysis, scarring, tumor
- Severity and distribution of glabellar and nasal root rhytides
- Degree of dermatochalasis, hooding, and eyelid ptosis
- Facial nerve function and any history of prior facial palsy
- Prior scars
- Do not forget to assess lower eyelid tone, position, and canthal position
Anatomy and Physiology
Surface Anatomy[2]
More than most other cosmetic and reconstructive procedures on the face, surgery to the brows demands an accurate understanding of the surface anatomy, the brow position, and shape. Although there is variation in the brow height and curve in different races, the overall difference in brow shape and position between males and females applies to most societies.[3]
Generally, male brows are more horizontal, while female brows have a more impressive arch and curve from medially to laterally. In either gender, the medial brow generally sits about 1 cm above the superior orbital rim. Over time, it rides lower in men, which means this measurement does change with age but would still rate as normal. Male brows run mostly horizontally with only a mild arch laterally. In women, the arch of the brow is at its highest at the lateral limbus, although some cultures admire brows that rise further out from the point of the lateral limbus. The exaggerated lateral arch has been used in Chinese opera and other arts to give the brow, and therefore the face, a dramatic look.
When assessing brows for possible ptosis or an ideal position and curve, the patient requires examination sitting up and ideally with photographs from when they were younger. Patients should bring pictures from the age of 18 years but also the photographs in which they think they look the best. This approach applies to brow lifts, blepharoplasty, face, and neck lifts. Sometimes, the appearance at 18 years of age may not be optimal. Many ladies, for example, prefer the appearance of the face, jawline, and neck when they are in their 30s. The same applies to eyebrows. It is important for the surgeon not to impose his aesthetic upon the patient. What may look good to the surgeon may look unacceptable to the patient. Therefore, during the consultation, surgeons should lift the brow medially, centrally, and laterally to assess the best position and arch while showing this to the patient in a mirror. Computer morphing graphics are an option; however, patients may focus on the minutiae and try to change the shape in ways that are impractical. We have stopped using computer morphing graphics in our practice.
The "two-finger approach" shows patients the desired height and curve to the brow (similar to the "two-finger facelift" predictor). Do it to each brow and then both brows together. One finger is placed a few centimeters above the medial brow and the other a few centimeters above the lateral third of the brow. It is essential to keep the fingers high up on the forehead to illustrate the height and curve of the desired brow position. Doing this can also illustrate how the secondary dermatochalasis of the upper eyelid is reduced, and the improvement one can get in the lateral crows' feet area and also allows the surgeon to judge how much actual upper eyelid surgery needs to be performed relative to the skin, orbicularis, and orbital pre-aponeurotic fat. In men, the aim is to create a more horizontal brow to keep with a masculine look but with adequate lateral support to reduce or correct temporal hooding and eyelash ptosis.
Scalp and Forehead
The five layers of the scalp are:
- Skin
- Fibrofatty superficial fascia (adherent to the skin and the underlying muscle and aponeurosis)
- Galea aponeurotica: The galea splits to form sheaths around the posterior occipitalis muscles and the anterior frontalis muscles.
- Areolar tissue, which is between the periosteum and the muscle sheath; this areolar tissue has emissary veins and small arteries.
- Periosteum
Muscles
The eyebrow/forehead complex is composed of the following major muscles, all innervated by the facial nerve:
Occipitofrontalis[4]
Occipitofrontalis is composed of two posterior bellies and two anterior bellies: occipital and frontal. The galea aponeurotica or epicranial aponeurosis connect these muscles. The superior nuchal line on the occipital bone gives origin to the occipital muscle bellies. These muscles insert into the galea aponeurotica. The anterior galea is attached to the skin and fascia of the eyebrows, passing through the orbicularis orbitalis muscle and posteriorly becomes the galea between the brow and the coronal suture. The blood supply to the occipital belly is from the occipital artery; the supraorbital and supratrochlear arteries supply the frontalis. The frontalis muscle inserts into the eyebrow and also interdigitates with the corrugator supercilii muscles.
Orbicularis Oculi[5]
Orbicularis oculi muscle is composed of the pretarsal, the preseptal, and the orbital orbicularis oculi. All three muscles arise from the medial canthal tendon with the preseptal portion having a deep head from the posterior lacrimal crest and the pretarsal fibers having a Horner muscle component medially. The orbital orbicularis meets laterally over the zygoma. The preseptal muscle forms the lateral palpebral raphe laterally, and the pretarsal muscle fibers unite laterally at the later canthal tendon. The orbicularis oculi is a constrictor, allowing closure of the eyelids, but it also draws in the brows, the lower part of the forehead, and the temple regions, mostly via its orbital component. The orbital orbicularis is a significant depressor of the brow. It is sometimes manipulated to change the positions and/or shape of the brow, as is done frequently with injections of botulinum toxin into the lateral orbital orbicularis fibers. These orbital orbicularis muscle fibers are also particularly active in patients with blepharospasm, who experience forceful closure of the eyelids with an inferior movement of the brows.
Corrugator Supercilii Muscles
These are responsible for producing the vertical frown lines, the "elevenses." The muscle originates from the frontal bone at the superomedial orbital rim (nasal process) and inserts laterally into the medial and central third cutaneous part of the brow and interdigitates with the frontalis muscle. It bears mentioning that the lateral extent of the corrugator muscles is often variable in different people. Sometimes, it extends all the way to the lateral third of the brow. The assessment of the corrugator action is important when treating patients with botulinum toxin for cosmetic reasons or blepharospasm. There has been some controversy about the medial corrugator muscle, which was thought by some to be an elevator of the medial brow: this view is not widely accepted.
Procerus Muscle
This muscle arises from the nasal bone and merges into the inferior part of the frontalis muscle: it pulls down the medial eyebrows resulting in horizontal upper nasal bridge wrinkles. Over time, this crease can be quite deep with evidence of the descent of the central frontalis muscle as only by lifting this does the horizontal groove improve. We have called this the "fat nose syndrome" caused by a combination of medial movement of the brows because of the corrugator, the inferior movement caused by the procerus, and the vertical descent of the frontalis muscle, resulting in a widening of the soft tissues at the nasal bridge which looks like a "fat nose."
The Retro-Orbicularis Oculi Fat Pad (ROOF)
Most muscles in the body do not glide over the bone. Many have a fatty plane. Behind the orbicularis oculi and the frontalis muscles where they interdigitate, there is a fibrofatty layer of tissue which has been called the "brow fat pad" or the retro-orbicularis oculi fat (ROOF) pad. It sits distinct from the preaponeurotic fat, which is behind the orbital septum, while the ROOF is on the periosteum of the orbital rim and frontal bone, in front of the orbital septum. In some cases, the fat extends further inferiorly below the orbital rim and into the eyelid, even as far as the inferior septal attachment to the levator aponeurosis. The fat gives the youthful fullness of the brow seen before there is atrophy. Atrophy causes skeletonization of the brow with the orbital bony rim showing. Several surgeons have suggested that this brow fat pad should be removed during blepharoplasty to improve the outcome. The only time this fibrofatty layer should be "sculpted" is when it is increased in its thickness, as is sometimes seen in patients with Graves disease.
In medicine, "rediscovery" is presented as a new finding. This fibrofatty layer was described in 1909 by M. Charpy, although he mistook it to be a lateral fat pocket. It is referred to as the Charpy's fat pad in certain parts of Europe. While the middle eyelid fat pad may spill into the lateral space, any prominence laterally in the upper eyelid should be assumed to be the lacrimal gland until proven otherwise. The ROOF pad should be refilled in aesthetic cases, instead of being removed.
In the medial third of the eyebrow, there can be firm attachments of the galea to the periosteum. These are found in the subperiosteal plane in endoscopic brow lifts and might be the reason why marked medial brow ptosis is rare. The fibrofatty layer described above allows ease of movement of the brow centrally and laterally, causing the wide excursion of the brow above and below the orbital rim when using the relevant muscles.
When dissecting in the brow fat pad (ROOF), a prominent horizontally running artery and vein are encountered. These branches of the temporal artery and temporal vein are preserved when operating in this region.
Motor Nerves
Facial Nerve
The motor supply to the forehead, brow, and periocular muscles comes from the facial nerve, which exits the stylomastoid foramen. It enters the anteromedial surface of the parotid gland and then passes within the posterior part of the parotid gland superficial to the retromandibular vein and external carotid artery. It divides into five terminal branches (frontal or temporal, zygomatic, buccal, mandibular, and cervical branches).
Frontal Branch of the Facial Nerve
This nerve is the most superior branch which exits the superior part of the parotid gland and goes on to supply the anterior and superior auricular muscles, the frontalis muscle, the orbicularis oculi muscle, and the corrugator supercilii muscles. The frontal nerve sends branches to the lateral end of the corrugator supercilii muscle.
Facts about the frontal branch of the facial nerve:
- The surface marking of the frontal branch is called Pitanguy's line, which starts 0.5 cm below the tragus and extends to are 1.5 cm above the lateral brow and 2 cm lateral to the lateral orbital rim.
- The nerve travels in the musculoaponeurotic layer, and above the zygoma, it runs on the undersurface of the temporoparietal fascia.
- The anterior branch of the superficial temporal artery and vein are lateral to the frontal branch.
- Although portrayed as a single nerve, the nerve divides into several (but variable) branches over the zygomatic arch.
- Important landmark over the zygoma: if one measures 2 cm from the lateral orbital rim, then the next 2 cm over the zygomatic arch would be where these branches would be. They can remain safe if the dissection plane here is subperiosteal.
- The exact innervation of the corrugator, procerus, and orbicularis oculi muscles have only recently been worked out. The medial corrugator and procerus muscles receive nerve supply from branches of the zygomatic and buccal branches of the facial nerve, which loop medially and superiorly. They also supply the medial canthal region of the medial upper and lower lids.
Sensory Nerves
The three primary sensory nerves of the forehead and brow are the supraorbital nerve, the supratrochlear nerve, and the infratrochlear nerve.
The supraorbital nerve is the larger and more lateral branch of the frontal nerve (which is the largest branch of the ophthalmic nerve (V1). Other branches of the ophthalmic nerve are the nasociliary nerve and the lacrimal nerve. The supraorbital nerve exits the orbit either through a notch on the superior orbital rim or through a foramen just above the rim. The nerve is deep to the corrugator supercilii muscle at this point. The nerve then divides into a medial (superficial) branch, which passes over the frontalis muscle and provides sensation to the forehead skin and the anterior 3.5 cm of the scalp. A deep (lateral) branch runs laterally between the galea aponeurotica and the periosteum to the coronal suture. It is this division that suffers injury in cosmetic and reconstructive procedures resulting in paresthesia and scalp numbness. It supplies sensation to the upper eyelid, the forehead, and the scalp as far as the lambdoidal suture.
Some important facts about the supraorbital nerve:
- A recent study on Sri Lankan skulls found that 73.8% of supraorbital nerves exited through a notch, with the rest through a foramen.[6] However, other studies have shown the presence of a notch to be between 47% and 92%, and the presence of a foramen to be between 8% and 51%.
- 36.3% had a notch on one side and a foramen on the other side
- 55.1% had bilateral supraorbital notches
- 8.6% had bilateral supraorbital foramina.
- Accessory exits of branches of the supraorbital nerve may be present in up to 20% of cases, usually lateral to the notch/foramen.
- The supraorbital nerve exit was 24 mm from the midline, 28 mm medial to the temporal crest of the frontal bone, and 29 mm from the frontozygomatic suture (rounded numbers).
- When a foramen was present, it was 2 mm above the supraorbital margin in males and 3 mm in females.
- In 80% of cases, the supraorbital foramen/notch is medial to the infraorbital foramen, contrary to the normal belief that both are in the same sagittal plane.
The supratrochlear nerve may exit through a foramen, although more often, it exits through a notch or depression in the bone. The nerve exits lateral to the corrugator supercilii muscle's bony origin. It enters the muscle and divides into three to four branches, which run deep to the anterior surface of the corrugator supercilii muscle. Then, after penetrating the frontalis muscle, the nerves run vertically on the medial surface of the frontalis muscle. The supratrochlear nerve supplies a width of 1 cm of the forehead centrally.
The infratrochlear nerve is a branch of the nasociliary nerve (which is a branch of the ophthalmic division of the trigeminal nerve). The nerve runs along the upper border of the medial rectus and will often have branches from the supratrochlear nerve. Several branches of the nerve pass to the medial angle of the eye, supplying medial upper and lower eyelid skin, side of the nose, the conjunctiva, the lacrimal sac, and the caruncle.
Surgical landmarks: Traditionally, the supraorbital nerve is marked 2.7 cm from the midline and the supratrochlear nerve 1.7 cm. As seen above, there will be variability within a population as well as between races.
Fascia
The temporal fascial planes subdivide into the following:
The temporoparietal fascia is an extension of the superficial musculoaponeurotic system (SMAS), which extends across the zygomatic arch and, together with the galea, the frontalis, and the occipitalis, forms a continuous fascial plane in the face. The temporoparietal fascia is best termed as the superficial temporal fascia. The frontal branch of the facial nerve lies under this surface.
The deep temporal fascia has a superficial and a deep part.
The superficial temporal fascia is separated from the deep temporal fascia by loose areolar tissue, which allows easy dissection when performing a temporal dissection. This plane, also called the subaponeurotic plane, is avascular and allows quick, blunt separation.
The deep temporal fascia is thick and overlies the temporalis muscle, where it is one layer. However, below the level of the superior orbital rim, the deep temporal fascia splits into a superficial and a deep part, separated by Yasargil's fat pad. The extent of Yasargil's fat pad is from the temporal line of fusion down to the zygomatic arch and anteriorly extends to the lateral orbital wall.
The buccal fat pad and the deep temporal fat pad overlying the inferior part of the temporalis muscle and tendon are continuous under the zygomatic arch.
Critical anatomical landmarks: The superficial temporal fascia and the deep temporal fascia adhere to the temporal crest as the temporal fusion line. Inferiorly this fusion is dense and is termed the conjoint fascia, which needs to be released to mobilize the lateral brow. The dissection is always carried under the superficial temporal fascia to the subperiosteal plane by dissecting through the temporal fusion line deep to the superficial temporal fascia and from the lateral to the medial direction.
Indications
Difficulties Assessing Brows
- Every person's brows will descend over time, and therefore there are no statistics to show the true incidence of brow ptosis in a given age group.
- With age, everyone has some degree of brow ptosis.
- Most people may have brow ptosis, but this does not necessarily contribute to any significant visual problems.
- Since the objective assessment of brow ptosis is poorly defined in normally aging populations, it is left to the physician and the patient to decide if brow height and curve need to be changed.
- Almost every patient with significant dermatochalasis, which causes temporal hooding and interferes with the superior visual field, will have some degree of brow ptosis. In theory, every one of these patients would benefit from an elevation of the brows. However, this does not mean they all need surgical intervention.
- Patients as young as in their 20s and 30s will also show some degree of brow ptosis, especially in those who lead an active outdoors lifestyle because of the resultant overaction of the corrugator, procerus, orbital orbicularis, and frontalis muscles, together with solar elastosis.
In a surgeon's office, every patient seeking aesthetic improvement of the upper half of the page (whether seeking forehead rejuvenation, brow lifting, or upper blepharoplasty) should have their brows assessed. Brows will cause vertical redundancy (dermatochalasis, temporal hooding, lash ptosis, brow ptosis) and horizontal redundancy (corrugator frown lines, "fat nose" syndrome). Even if brow repositioning is not performed, it is important to illustrate to the patient the degree to which the forehead and brows and periorbital tissues contribute to the changes seen in aesthetic patients and the degree to which the field may become obstructed in reconstructive patients.
International Frequency
There are regional and racial differences in the degree to which the forehead, the brows, and upper eyelids affect patients aesthetically and functionally. In Africans, brow ptosis is not common. Even dermatochalasis seems to be much less common in these patients, even though in many of these countries, patients live and work outdoors, usually with no protection from the sun.
In the Eastern races, the naturally low eyelids with the low insertion of the orbital septum and low skin crease mean that these patients will have apparent dermatochalasis and ptosis from a young age. Many will seek cosmetic creation of skin creases. But most patients who age naturally are not troubled by the obvious dermatochalasis and apparent ptosis until they are much older than Caucasians. Furthermore, brow ptosis is also less of an issue in Eastern races.
In the modern world, where people feel judged by their outward appearance and expression, the impression created by the face is important. For example, in Southern Korea, applicants for jobs to companies always have to send their facial photographs with their job applications. In visits to South Korea, visiting clinicians have been informed that company psychologists reject many applicants even before interviewing the candidates because the face was not considered pleasing.
A recent study showed areas of the face that most impacted the perception of age in order of importance:
- Full face aging
- Middle-third facial aging
- Lower-third facial aging
- Upper-third facial aging
- Vertical lip rhytids
- Horizontal forehead rhytids
Brow shape is used by professionals to convey moods by relatively minor movements and changes in shape: low lateral eyebrows denote sadness or concern, lower medial brows indicate anger, flat or low brows may denote tiredness, and appropriately arched brows would indicate vitality and happiness.
Similarly, temporal hooding and upper eyelid dermatochalasis may indicate tiredness, but when combined with frontalis overaction because of the heavy upper eyelids, the appearance of tiredness becomes multiplied. It is well known that if upper blepharoplasty and ptosis repair take place without addressing any low brows, the brows will appear lower after surgery because the impetus to keep the frontalis tonically active is taken away once the visual fields are improved.
Overview of indications for performing any brow lift:
It is well-recognized that brow elevation is helpful for patients with significant brow ptosis, which leads to a visual field constriction and secondary dermatochalasis. In some patients, the brow droop may be limited to the tail of the brow, which gives secondary temporal hooding with lash ptosis. Cosmetically, brows are a powerful indicator of mood, and some patients will benefit from changing the shape and curve of the brow to make the face look less tired, angry, sad, or quizzical. Patients with facial palsy will have denser brow ptosis, which also interferes with vision. Finally, there will be patients who will have undergone upper lid surgery with ptosis repair or blepharoplasty but still have underlying brow ptosis, which may be exposed by the lifting of the lids.
Some specific patients benefit from mid-forehead brow lifting. The deep forehead lines in men are particularly useful for the placement of incisions. In some patients, by using a mid-forehead incision and appropriate dissection, the frontal hairline can be lowered. Finally, physician and patient preferences are taken into account, especially in men with a high hairline, where incisions for endoscopic brow lifts or coronal lifts may leave more prominent marks or depressions than is desirable. Some patients welcome a mid-forehead incision and do not mind the scar as long as it is not prominent.
Contraindications
Midforehead brow lifts are carried out via midforehead incisions. Even with the best closure, some degree of scarring is inevitable. It is crucial to avoid this approach in patients where it is absolutely contraindicated or where the scarring would be perceived to be unacceptable even if minimal.
Absolute Contraindications
- Patients without forehead furrows: Here, even mild scars would be obvious to the patient.
- Women: In ladies, there are other better ways to address the forehead and the brow position and curve. The exception is a patient with dense facial paralysis.
- Some patients absolutely do not want a visible scar on the forehead: this may apply even to patients with deep midforehead furrows where the scars could be minimized. Surgeons should show patients before-and-after photographs and close-up photographs to ensure that they are fully informed of what to expect, within reason. A truism in plastic surgery is that one cannot make an incision on the body and NOT have a scar; this should be stressed to every patient, even to patients undergoing just upper blepharoplasty, where the scars are rarely visible to the patient.
Relative Contraindications
- Low anterior hairline
- Young men
- Where alternative approaches are available and are likely to succeed with reduced scarring. With advances in minimally invasive techniques and the use of the endoscope, functional, and cosmetic procedures are now possible to achieve desired results with minimal scarring.
Equipment
A basic plastic surgery set which has retractors of various kinds is needed. Sewell retractors and double-pronged rakes are especially useful. No other specialized instrumentation is necessary.
Preparation
When performing brow ptosis repair of any kind, it is crucial to obtain a detailed history, including the specific complaint and duration of the problem from the patient. Besides the clinical examination, a surgeon should have a basic psychological examination system, especially in cosmetic cases, but sometimes even in functional cases. The surgeon and patients should have a detailed discussion of the proposed surgery, together with a discussion of the possible outcomes and complications.
Patient Consultation
Cosmetic patients are interviewed and counseled differently from reconstructive patients.
Showing the patient the changes the physician sees and aims to rectify is vital. Always illustrate the differences and goas with the patient standing in front of a large mirror. Point out asymmetry, discuss findings, stress aims objectives, and address concerns.
Point out desired brow height and curve and discuss surgical incisions, advantages, and disadvantages, as well as limitations and scarring. Before-and-after photographs of other patients are useful in showing patients the sort of results one aims to get but also to encourage them to ask questions based upon what they see. Photographs of scars are always shown to the patients. Take photographs with and without a flash and at different angles. On rare occasions, a willing previous patient may be made available for the patient to meet and examine physically.
Informed consent for a midforehead browlift should include the following points:
- The brow height will not be absolutely symmetrical as no person has perfectly symmetrical brows.
- The brow arches will not be absolutely symmetrical.
- Over the first few weeks, it is normal for the brow to "settle," and therefore, the initial brow height, as seen by the patient, is not the final brow position.
- The aim is to create a natural-looking brow height and curve.
- With modern surgery, brow motility is retained, so some degree of mobility of the corrugator and procerus muscles are expected.
- Some degree of numbness always occurs, and in the majority of patients, it decreases over weeks but sometimes takes months.
- The brows WILL droop again with age and with time.
- No surgery lasts forever, including mid-forehead lifting.
- Risks of infection, wound dehiscence, asymmetry, and need for adjustment require discussion.
Various types of "brow design" have been proposed. In practice, there are so many variables (age, gender, cultural, environmental, occupational, among others) that each patient is approached individually with the goal to "design" a specific position, arch, and look. The "look" is not just dependent upon the brow, but a combination of what else is performed as brow lifts frequently accompany other procedures.
Preoperative Preparation
Forehead surgery, in general, and mid-forehead surgery, in particular, will cause impressive bruising. Therefore, aspirin and aspirin-containing products, as well as anti-inflammatory medications, are stopped one week before surgery, including all vitamins, oral supplements, and garlic supplements. The list of drugs containing aspirin and aspirin-like products is so long that patients must either read the medication bottles or to bring them in so staff may guide them as to whether they may take the particular supplements.
Patients must remove all makeup the night before and come in without false eyelashes. The skin is cleansed by the patient the night before and again, the morning of surgery, to ensure the removal of all makeup products.
Clinical photographs are obtained using the following positions:
- Full face straight
- Full face 45 degrees right
- Full face 45 degrees left
- Full face 90 degrees right
- Full face 90 degrees left
- Close up of both eyes, forehead, brows, and upper and lower lids at similar angles
The same set of clinical photographs are taken two months or more after surgery and shared with the patient.
It is advisable to interview each patient at least twice before scheduling surgery. This approach allows the patient sufficient time to express desires and concerns. Furthermore, and just as importantly, this allows the surgeon to get to know the patient. Especially in cosmetic surgery, certain patients are not suited to surgical intervention, and this may become apparent during subsequent interviews. Patients should understand that they always have the final choice of undergoing or not undergoing surgery, be it functional or cosmetic.
Technique
Please see the attached composite illustration for an explanation of the following technique.
Skin Markings
- A decision is made whether to use a horizontal incision across the mid-forehead or to step the incisions, where the incision is placed in a different groove from the opposite side. Whenever an incision is not made right across the forehead, always “step” the incisions.
- The incision lines stop at the temporal line of fusion, but in some cases, the incisions are carried further laterally.
Anesthesia
- Supraorbital and supratrochlear nerve blocks are administered under sedation, using 2% lidocaine and epinephrine mixed with sodium bicarbonate (9 to 1 respectively).
- Further injections are administered along the lines of the incision and also under the brow and in the glabellar region. The infratrochlear nerve is blocked. Adequate vasoconstriction occurs in 10 to 15 minutes, and cool compresses are applied at this stage and continued throughout the procedure.
- The local anesthetic injections are administered before the preparation and draping of the patient, allowing the anesthetic and vasoconstriction to take effect.
Incisions
- A No. 15 C-blade is used to make a skin incision down to the galea aponeurotica.
- Warning: Incisions carried laterally to the temporal line of fusion must be skin deep only.
Dissection and Procedure
- The plane of dissection is subcutaneous but on the galea, which is not entered. Elevating the inferior flap with rakes and performing a combination of sharp dissection and blunt separation with scissors is the most useful approach.
- There is a loose subcutaneous aponeurotic layer; dissection is performed in this layer all the way to the superior orbital rims.
- Access to the corrugator and procerus muscles is achievable by incising the galea horizontally (over a distance of 2 cm) about 3 cm above the nasal root; this is the subgaleal plane. Care is taken not to injure the supraorbital nerves laterally.
- Hemostasis is important throughout the procedure.
- After visualization of the supraorbital and supratrochlear neurovascular bundles, the corrugator and procerus muscles become weakened.
- The degree to which the corrugator and procerus muscles need to weaken requires an assessment before surgery. In some patients, partial removal of the muscles with clamping and cauterization is performed. In others, surgeons aim for minimal weakening. For more aggressive weakening, the muscles can be disinserted from the bony origins and dissected off while protecting the neurovascular bundles. Procerus removal is more aggressive in addressing horizontal nasal root creases.
- In the last few years, some surgeons have been grafting any fat removed (from upper eyelids or the SMAS if performing a facelift) to the area where the procerus and corrugator muscles are removed for two reasons: (1) to fill any hollows that may form and (2) to get filling of the preoperative rhytids which are inevitably present.
- As eversion of the skin edges is vital, the upper part of the incision is undermined for approximately 1 cm. Deep creases require partial-thickness horizontal cuts of the frontalis.
- The galeal incision is closed after the excision of the excess with 4-0 polydioxanone sutures. Then pull up the inferior flap and excise redundant skin created by the preferred degree of brow position.
- Some surgeons run horizontal and vertical sutures from the point of the incision to the orbital orbicularis and back again in the form of rectangles, which give frontalis tightening and support and reduces the tension placed on the skin closure. This approach is akin to the SMAS lift by imbrication that occurs in facelifts: we have found this to be especially effective in males where there is significant ptosis of the brows.
- Excess skin is removed after elevating the inferior flap to design the brow height and curve.
- The dermis is sutured with 5-0 polydioxanone to take up the tension. Skin closure is achieved with eversion performed during the deep closure, and skin closure is performed using 6-0 polypropylene suture.
- Steristrips and a soft pad are applied. Recently, we have begun to use Velcro-based forehead dressings, which pass under the chin, allowing the application of firm dressing on the forehead. This dressing may be removed and reapplied as desired.
Variations
Because the orbital orbicularis is a depressor of the brow, in some patients, surgeons weaken the orbital orbicularis muscle. Since some surgeons have started imbricating the frontalis muscle as described, they have found less of a need to suture the deeper brow tissues to the periosteum.
The dressing is removed the day after the surgery, and wound closure strips and sutures are removed after seven days. More wound closure strips are placed if needed.
Overcorrection of the brows is to be expected in the first few weeks. The forehead and the brows always relax by at least 25%. However, since the incision is closer to the brow than it is with the coronal lift or endoscopic brow lift, the descent of the brow after surgery is less than with those two approaches.
Surgeons should obtain clinical photographs at two months and six months after surgery and observe these patients for up to a year.
Complications
Hematoma
The forehead is very vascular. The mid-forehead lift, in particular, is an “oozy” operation because of the plane of dissection. Meticulous hemostasis is crucial during the dissection. Surgeons generally will review the whole bed after irrigation with saline to spot any small bleeders, which are often present after such a maneuver. Any hematoma requires immediate drainage as this is a skin flap at risk of necrosis.
Facial Nerve Injury
The frontal branch of the facial nerve is at risk if the lateral end of the incision is extended and carried deeper than the skin. Local edema and tension can give rise to paresis, which will recover. Care is also necessary with the use of cautery to avoid thermal injury to the nerve.
Sensory Nerve Injury
- Hypesthesia: Most patients will experience temporary hypesthesia because of the raising of the skin flap; this usually recovers in a few days. When entering the galea, care is crucial to protect the sensory nerves.
- Paresthesia: Paresthesia commonly lasts several weeks but improves
- Neuralgia: Injury to the supraorbital nerves can cause neuralgia.
Incision Pruritus
This condition is to be expected for the first week to 2 weeks after surgery.
Depressed or Widened Scar
Forehead scars are very variable, even when closed with proper attention to eversion and closure with minimal tension. Where significant solar elastosis is present, the scar may become hypopigmented or hyperpigmented. Scarring is also variable: most patients do not mind the mild hypopigmentation that may occur, but any widening of the scar becomes more of a problem. Scars can improve with dermabrasion or the use of the carbon dioxide laser about 4 to 8 weeks after surgery. The presence of vessels, which can sometimes occur, especially in patients with marked solar elastosis, may be treated with one of the vascular lasers. Stepped incisions can lead to one scar being more obvious. Depression is a significant problem absent proper closure techniques.
Brow Asymmetry
Brows are, by their very nature, always somewhat asymmetric. Post-operative asymmetry should ideally not be more than that seen preoperatively. There is rarely sufficient asymmetry to require revision surgery.
Abnormal Soft Tissue Contours
Contour deformities were not uncommon with complete resection of the corrugator and procerus muscles. The modern approach is to modify but not to completely remove these muscles, leading to fewer contour deformities. We often use fat grafts during surgery to fill any undulations present before or during surgery.
Lagophthalmos
Brow lifts are often combined with upper eyelid surgery. Temporary lagophthalmos is almost universal, but only for a few days. The surgeon must pay attention to the preoperative examination of Bell’s phenomenon and lower eyelid position and tone.
Clinical Significance
All procedures seem to go through phases of popularity and then wane. Mid-forehead lifts were more popular before small incision procedures and endoscopic procedures were developed. However, there are specific patients where the mid-forehead brow lift is ideal: when chosen with care, the outcomes are effective, satisfying, and cosmetically very acceptable. The main advantages of this operation are that because the incision is closer to the brow than with coronal and endoscopic lifts, the brow height and curve can be manipulated more effectively and more reliably. Asymmetry is also addressable with greater ease.
Risks of brow lift, either alone or in combination with upper eyelid procedures, are very low.
Internal brow lifts seem to be performed more frequently of late; this may be because of the ease of performing these internal "brow lifts." Effectivity and longevity remain unproven. Anatomically, pushing a brow up makes little sense.
Important points about brow ptosis and mid-forehead brow surgery:
- The surface marking of the frontal branch is called Pitanguy's line, which starts 0.5 cm below the tragus and extends to are 1.5 cm above the lateral brow and 2 cm lateral to the lateral orbital rim.
- Surgical landmarks: Traditionally, the supraorbital nerve is marked 2.7 cm from the midline and the supratrochlear nerve 1.7 cm. As seen above, there will be variability within a population as well as between races.
- Anatomical landmarks: The superficial temporal fascia and the deep temporal fascia are adherents at the temporal crest as the temporal fusion line. Inferiorly this fusion is dense and is termed the conjoint fascia, which needs to be released to mobilize the lateral brow. The dissection is always carried under the superficial temporal fascia to the subperiosteal plane by dissecting through the temporal fusion line deep to the superficial temporal fascia and from the lateral to the medial direction.
Enhancing Healthcare Team Outcomes
Mid-forehead brow lifts are performed by experienced and skilled surgeons with an intimate knowledge of anatomy, physiology, and familiarity with preoperative and postoperative care.[7] [Level 5]
(Click Image to Enlarge)
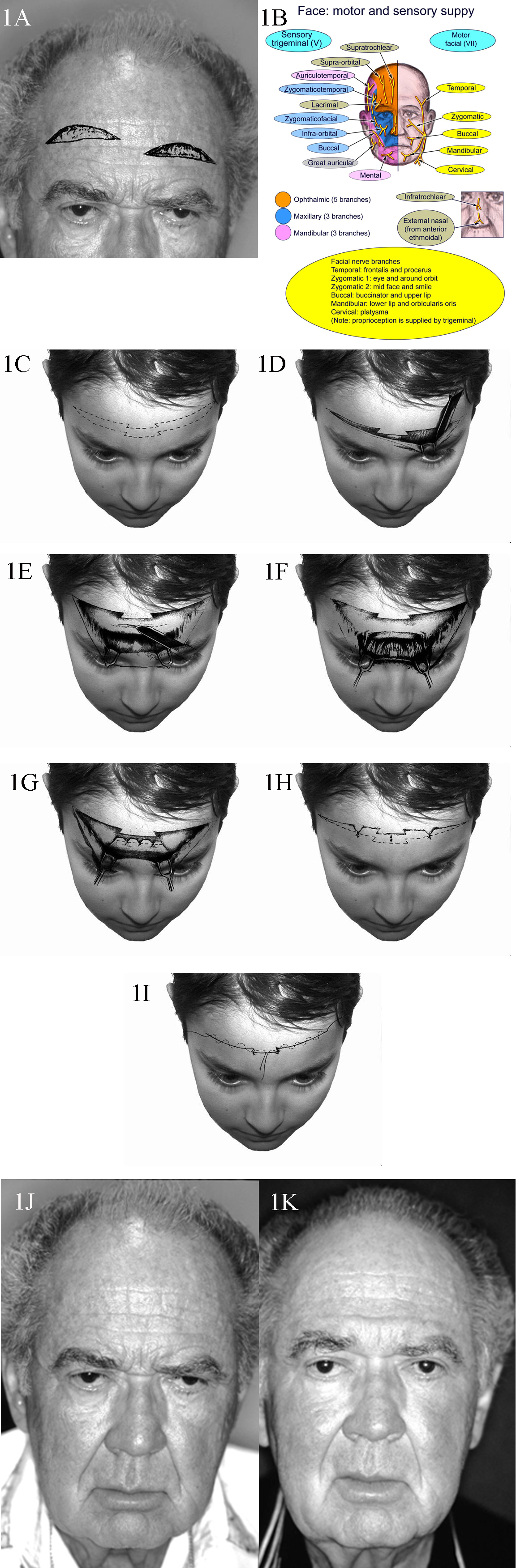
1A. Patient with typical upper lid ptosis and severe brow ptosis. Incisions for midforehead lift may be staggered as shown here to prevent a long horizontal scar. 1B. Sensory and motor nerve supply of the face. 1C. Transverse forehead incisions may be staggered or be broken up as shown to improve the final scar. 1D. Dissection performed in the subcutaeneous plane. 1E. Transverse incisions are made in the galea to access the corrugator and procerus muscles. These incisions are kept in the middle to prevent injury to the supraorbital nerve branches. 1F. Once exposed, the corrugator and procerus muscles are attenuated. 1G. The galea is shortened as desired and sutures placed. 1H. Elevation of the cutaneous structures is obtained and relevant trimming performed. 1I. Meticulous subcuticular closure is performed with no tension on the skin edges. 1J. A 68-year-old man with markedly overactive corrugator and procerus muscles. 1K. A reasonable elevation of his brows has been achieved.
Contributed by Prof. Bhupendra C.K. Patel MD, FRCS