
Brow Ptosis
- Article Author:
- Russell De Jong
- Article Editor:
- Marc Hohman
- Updated:
- 8/10/2020 10:51:57 PM
- For CME on this topic:
- Brow Ptosis CME
- PubMed Link:
- Brow Ptosis
Introduction
Brow ptosis is an abnormal descent of the brow from its anatomical position to the point that a patient becomes uncomfortable with the brow's appearance or visual field deficits develop. The normal adult upper lid lies 1.5 mm below the superior corneal limbus. Ptosis can be congenital or acquired.[1] Most commonly, it is seen in the elderly due to age-related involutional change of the facial soft tissues.[2] The commonest cause of congenital ptosis is myogenic due to the abnormal development of the levator muscle. However, a full evaluation is still required to exclude more dangerous etiologies and select the correct treatment for each patient.
Etiology
Brow ptosis is almost always acquired. Congenital brow ptosis is rare, and causes include underdevelopment of the facial nerve and mimetic muscles.
Acquired cases may arise in a variety of ways:
- Age-related: This is the most common form and is associated with changes in the soft tissues of the brow. Increased laxity of the connective tissue, skin, and frontalis muscle lead to drooping in the lateral third of the eyebrow first and may advance to the medial two thirds if left untreated.[3]
- Traumatic: Damage to the intracranial, intratemporal, or extratemporal facial nerve can result in ptosis of the brow. If the damage is anywhere from the facial nerve nucleus proximally to the pes anserinus distally, a hemifacial palsy will be seen. Damage specific to the frontal branch will denervate the ipsilateral frontalis muscle and parts of the corrugator supercilii, procerus, and orbicularis oculi muscles.[4] Fracture of the temporal bone is one of the most common causes of traumatic facial palsy. Other causes include trauma to the parotid gland, zygomatic arch, and mandibular body.
- Myogenic: Myopathy specific to the facial musculature and systemic myopathy can contribute to brow ptosis via atrophy or denervation of the frontalis muscle. Examples include myasthenia gravis, myotonic dystrophy, and oculopharyngeal muscular dystrophy.[5]
- Infectious: Ramsay Hunt syndrome is a reactivation of the varicella-zoster virus that leads to facial paralysis and a herpetic rash of the ear canal, auricle, scalp, or oropharyngeal mucous membranes. This condition causes an ipsilateral full facial palsy that includes brow ptosis.[6] Many other infectious agents can lead to central or peripheral facial nerve dysfunction, including but not limited to herpes simplex virus, Lyme disease, tertiary syphilis, West Nile virus, HIV, and polio.
- Spasm-induced: Congenital or acquired spasms of the orbicularis oculi can pull the brow down and away from its anatomic position, eventually causing a permanent change. Examples include blepharospasm and facial dystonias.[7]
- Neoplastic: Neoplasms of, or infiltrating into, the facial nerve affect its function and cause brow ptosis. Some of the most common include cancer of the overlying skin like a basal cell or squamous cell carcinoma, or more proximal masses like acoustic neuromas.
- Iatrogenic: Operations in the area of the brow pose a significant risk to the innervation and structural integrity of the brow. Overall, the procedures that pose the highest risk for postoperative facial nerve palsy are acoustic neuroma resection and temporomandibular joint procedures. Operations to improve brow and overall facial cosmesis such as endoscopic and open facelift procedures can cause facial nerve palsy and exacerbate the problem they were attempting to correct, but this occurs in less than 1% of procedures. Botulinum toxin injection also carries a risk of brow ptosis; overzealous or misplaced injections effectively denervate the brow elevators.[8]
Epidemiology
Anecdotally, it would appear that the bulk of cases are associated with the natural aging process, although literature definitively investigating the epidemiology of brow ptosis is lacking. Congenital brow ptosis is rare; only 4.9% of facial palsy cases are congenital.[9] The small proportion of remaining cases can be attributed to the other acquired etiologies discussed above.
Pathophysiology
Several soft tissue layers comprise the brow. From superficial to deep, they include the skin, subcutaneous fat, and the frontalis muscle; deep to this; there are the periosteum and skull.[10] The frontalis is the sole elevator of the brow.[11] The depressors of the eyebrow include the orbicularis oculi, procerus, and depressor supercilii muscles (the latter some consider to be a segment of the orbicularis oculi).[12] The facial nerve innervates all muscles of facial expression. The frontal branch innervates the frontalis and the lateral portion of the orbicularis oculi while the zygomatic branch innervates the procerus, corrugator, medial part of orbicularis oculi, and depressor supercilii.[13]
Aging or malfunction of any of the above units may lead to brow ptosis. As mentioned earlier, age-related changes in the brow elevators and the soft tissue overlying them are the most common cause of brow ptosis. Sun exposure, gravity, and the natural involutional degeneration of the skin and soft tissues are the main causative agents. Denervation of the brow elevators, whether via trauma, surgery, botulinum toxin treatment, or disease process, will lead to brow ptosis. Long-term spasm of the brow depressors can also lead to brow ptosis. Spasm may come about via spastic dystonia after facial denervation, facial tics in conditions like Tourette syndrome, or spastic diseases like blepharospasm.
History and Physical
The historical evaluation of a brow ptosis patient is key to determining the underlying etiology.
- History of present illness should be focused on the onset and progression of symptoms. A long term onset in an older patient clues the provider into an age-related case. In contrast, patients with more rapid onset may be suffering from Bell palsy, trauma, neoplasm, or other more unusual causes. A waxing and waning course with accompanying fatigability could be clues for myotonic dystrophy, myasthenia gravis, or oculopharyngeal dystrophy.
- The medical history should specifically evaluate for past instances of facial paralysis of any etiology, even cases long in the past.
- Chemotherapy and radiation should be asked about, as they can speed cutaneous and soft tissue aging.
- The surgical/procedural history must reveal all surgeries in the area of the brow and along the course of the facial nerve, including any neuro-otologic or neurosurgical procedures. Botulinum toxin injections must be inquired about.
- The social history should reveal sun exposure, smoking, and drug use as they can all speed involutional changes.
The physical exam should follow a formulaic, stepwise approach that is generalizable to all periorbital aging.[10]
- Neutral brow position should be evaluated by having the patient close his or her eyes and relax the facial muscles, then open the eyes as gently as possible without raising the brows.
- Brow versus lid pathology should be differentiated via manual elevation of the brow to the neutral position. A lid that is still ptotic after brow elevation indicates true blepharoptosis, rather than pseudoptosis caused by a drooping brow.
- Blepharoptosis should be thoroughly evaluated. Margin-reflex distance (MRD) is recorded. This is the distance measured from the corneal light reflex to the upper lid margin (MRD-1) or lower lid margin (MRD-2). MRD-1 less than 2-3 mm is indicative of blepharoptosis. The distance also needs to be measured between the upper eyelid margin and the superior palpebral crease. More than 8-10 mm often indicates blepharoptosis due to levator aponeurosis dehiscence. Brow asymmetry must also be noted if present. An asymmetric brow with symmetric eyelids may be masking ptosis on the side of the elevated brow due to excessive frontalis contraction in an attempt to compensate for a ptotic eyelid. Finally, the patient must be evaluated for the Hering phenomenon. If the elevation of a ptotic lid - or the lid on the side of the elevated brow - produces drooping of the contralateral upper eyelid, the patient may have bilateral but asymmetric blepharoptosis. Brow height asymmetry is also commonly caused by hemifacial microsomia, more frequently on the right than on the left.
- While not directly applicable to the evaluation of brow ptosis, the points mentioned here are essential to a thorough periorbital examination: festoons and fat pseudoherniation should be evaluated with digital pressure on the globe while visualizing the upper and lower lids. The former will not enlarge, but the latter will. Festoons will also contract with effortful eye closure. Lower lid laxity should be evaluated via the snap test. This is performed by distracting the lid from the globe, then releasing and observing lid recoil, which should take no longer than 2 seconds and should occur without the patient blinking. The lower eyelid vector should be evaluated via observation of the relationship between the cornea and cheek with the patient in the Frankfort horizontal position. If the cornea is anterior to the cheek skin at the infraorbital rim, the vector is negative. This is associated with aging and increased risk of ectropion if lower lid blepharoplasty is performed. Finally, tear production should be evaluated via the Schirmer test. Filter paper is inserted into the fornix of the lower eyelid; if there is less than 10 mm of dampness after 5 minutes, tear production is not adequate, and the surgeon must adjust the surgical plan accordingly.
- The hairline position and shape of the forehead must be visually evaluated to inform the surgeon’s choice of operative approach.
- A thorough cranial nerve exam should be carried out, especially if damage to the facial nerve is suspected.
Evaluation
Evaluation of brow ptosis outside of thorough history and physical is rarely necessary. However, there are some cases in which imaging and labs are beneficial or even diagnostic. Myogenic causes have lab tests specific to them; for example, suspected myasthenia gravis may be diagnosed via serologic testing for acetylcholine receptor antibodies.[14] Brow ptosis caused by neoplasm will need a full workup of the mass. These evaluations vary widely based on the suspected type of neoplasm, including anything from shave biopsy to MRI to PET scanning.
Treatment / Management
The treatment of brow ptosis [15] is dependent on brow morphology, ptosis etiology, severity, and, most importantly, patient goals. Surgical management is required for the resolution of age-related causes. It is also indicated in some traumatic, neoplastic, or iatrogenic causes. Those surgeries may include nerve decompression, removal of neoplasm, or nerve reconstruction, and are outside the scope of the current discussion. More common procedures used to treat brow ptosis are discussed below. Many of these procedures are combined with other rejuvenation procedures such as upper blepharoplasty, botox injection, or skin resurfacing.
The endoscopic brow lift also called the endobrow procedure, is the most common approach.[16] Dissection is carried forward from the median, paramedian, and temporal incisions in the subperiosteal plane (within the central forehead) and a plane along the fascia of the temporalis muscle (laterally) until the periosteum around the superior and lateral orbit is released at the arcus marginalis. Then the periosteum is lifted and fixated to the skull; this is often accomplished with resorbable implants, but may also be performed with screws and staples or a drill and suture. The endoscopic brow lift is best suited for patients with low or average brow height, defined as six or fewer centimeters from the brow to the hairline, and those without significant curvature or bossing of the forehead. A major benefit of this procedure is that it can address glabellar rhytides, a common comorbidity of brow ptosis, through the division of the corrugator supercilii or procerus muscles. Some limitations include only about 5 mm of lift, risk of damage to the frontal branch of the facial nerve which would exacerbate brow ptosis, risk of damage to the supratrochlear and supraorbital nerves that would cause forehead numbness, and difficulty in correcting brow asymmetry.
Open coronal approaches are named based on the location of the initial incision. Pretrichial incisions are placed at or just in front of the hairline, while trichophytic incisions are hidden within the hairline; the classic coronal incision passes directly over the vertex of the scalp. Dissection is carried forward in the subgaleal plane until diving subperiosteally 1-2 cm superior to the orbital rim. The flap is elevated, the excess skin and soft tissue are excised as necessary, and the incision is closed. These procedures allow for better visualization of critical structures like the frontal branch of the facial nerve and can achieve a higher lift than the endoscopic option. However, they result in significant scars that may be revealed by balding and more commonly cause minor complications like forehead numbness, pruritus, and alopecia.
The direct brow lift is performed through an incision just above the hair-bearing brow. Excess skin and soft tissue are excised to create a considerable amount of lift with a relatively minor procedure, one that can easily be done in the clinic under local anesthesia. This procedure is the most effective option for heavy lateral hooding and is the most straightforward procedure with which to correct brow asymmetry. Its drawbacks include the risk of visible scarring and an increased chance of excessive elevation that may result in a surprised look.
For significant brow asymmetry, particularly for patients with facial paralysis and very dense soft tissues, unilateral suture suspension of the ptotic brow to a titanium miniplate fixated to the frontal bone at the level of the hairline may be effective. As a side benefit, the sutures can potentially be tightened under local anesthesia in the future if the brow ptosis recurs or worsens.
The transblepharoplasty browpexy is a way to combine treatment of upper lid dermatochalasis or blepharoptosis with the treatment of brow ptosis. These conditions are often comorbid, so this approach is becoming more common. An upper eyelid blepharoplasty is performed first, then dissection is carried superiorly, along the orbital septum, until the pericranium above the supraorbital rim is reached. The periosteum can then be used as an anchor to suspend the brow from its deep surface.
The mid-forehead brow lift is mostly a procedure of historical interest, in which an incision is hidden within a deep, transverse forehead rhytid. The excess skin and soft tissue are excised, and the incision is closed like the direct brow lift. It has been largely abandoned because the scars are very hard to hide, and other options allow for a similar amount of lift.
Nonsurgical treatment may be pursued in particular cases. Botox injections effectively treat spastic brow ptosis or even elevate the brow slightly by weakening the depressor supercilii muscle; more systemic etiologies like myasthenia gravis need specialized medical therapy.
Differential Diagnosis
Brow ptosis is a fairly straightforward and well-defined diagnosis but may be confused with or obscured by other periorbital pathology. Asymmetric brow ptosis can seem like unilateral pathology unless a thorough physical exam reveals that the more ptotic side was masking the appearance of the less ptotic side. Severe dermatochalasis or blepharoptosis may distract the physician from identifying concomitant brow ptosis. A thorough history and physical examination will reveal whether a patient’s brow ptosis is age-related, traumatic, myogenic, spasm-induced, infectious, neoplastic, or iatrogenic.
Prognosis
Prognosis is highly dependent on etiology and the patients' primary concerns. For those who are mainly focused on the visual field deficits caused by their ptotic brows, full resolution and patient satisfaction can usually be achieved. [17] Patients whose concerns are primarily cosmetic have higher dissatisfaction rates. Patients with non-age-related etiologies have more varied prognoses.
Complications
Brow ptosis itself rarely progresses to more serious pathology. Its most notable sequela is visual field obstruction, progressing from lateral to medial.
Brow ptosis correction surgery complications include patient dissatisfaction (7.4%), numbness of the forehead due to supratrochlear and supraorbital nerve damage (5.5%), alopecia (2.8%), and brow asymmetry (1.7%).[8]
Nonsurgical brow rejuvenation complications are very rare. The most common complication of Botox treatment is periorbital bruising in 1.7% of patients.
Deterrence and Patient Education
Patients should be educated to their desired level of detail on the pathophysiology of the cause of the brow ptosis. Once sufficient understanding of the pathology is achieved, surgical and nonsurgical treatment options should be explained in order to inform a decision. A thorough discussion of both common and rare complications of the chosen treatment method is required.
Enhancing Healthcare Team Outcomes
Brow ptosis is a relatively common problem, but one that is often misdiagnosed or overlooked due to more apparent upper eyelid pathologies. Patients almost always first present to their primary care providers, who must refer to the appropriate facial plastics, general plastics, or oculoplastics specialist for definitive treatment. Once patients are directed to the correct subspecialist, close coordination among nurses, physicians, case managers, and others in direct contact with the patient is key to a timely and satisfactory outcome. Cases that are not age-related may require further consultation with neurosurgery, neurology, infectious disease, rheumatology, or other specialties.
Intraoperatively, a support staff made up of specialty-trained nurses who are familiar with the equipment and selected procedure in conjunction with a properly subspecialized and experienced surgeon is imperative to a safe and effective procedure. [Level 5]
(Click Image to Enlarge)
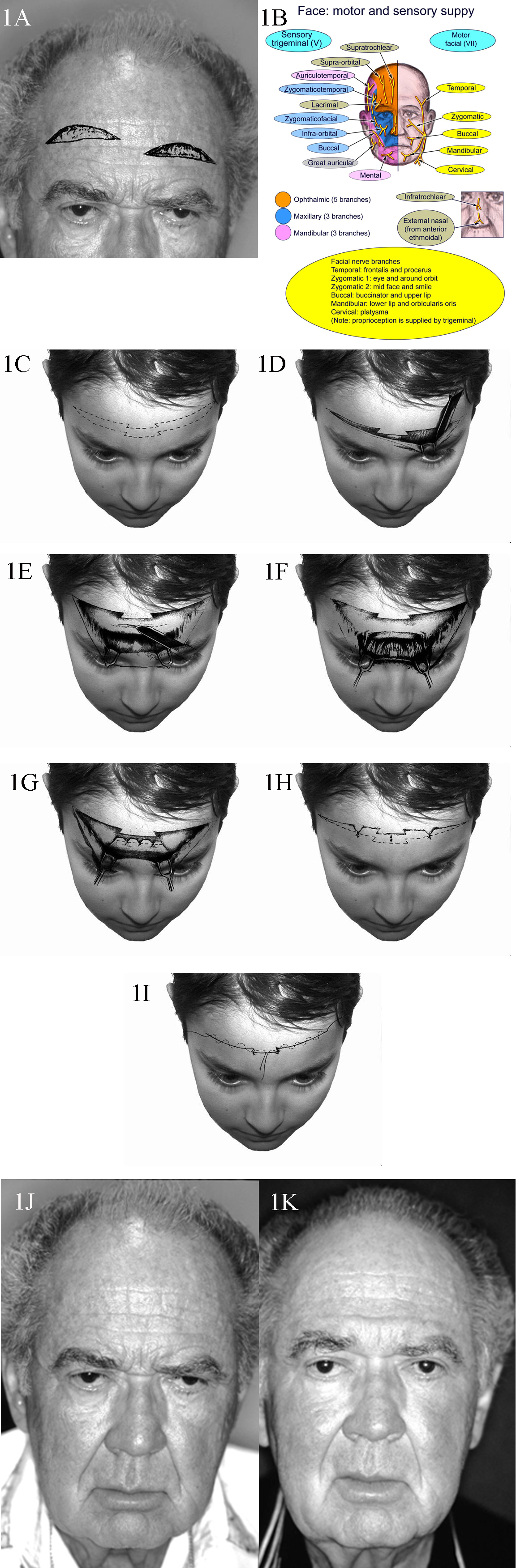
1A. Patient with typical upper lid ptosis and severe brow ptosis. Incisions for midforehead lift may be staggered as shown here to prevent a long horizontal scar. 1B. Sensory and motor nerve supply of the face. 1C. Transverse forehead incisions may be staggered or be broken up as shown to improve the final scar. 1D. Dissection performed in the subcutaeneous plane. 1E. Transverse incisions are made in the galea to access the corrugator and procerus muscles. These incisions are kept in the middle to prevent injury to the supraorbital nerve branches. 1F. Once exposed, the corrugator and procerus muscles are attenuated. 1G. The galea is shortened as desired and sutures placed. 1H. Elevation of the cutaneous structures is obtained and relevant trimming performed. 1I. Meticulous subcuticular closure is performed with no tension on the skin edges. 1J. A 68-year-old man with markedly overactive corrugator and procerus muscles. 1K. A reasonable elevation of his brows has been achieved.
Contributed by Prof. Bhupendra C.K. Patel MD, FRCS
(Click Image to Enlarge)

The Frontalis Muscle: The angle of insertion of the frontalis muscle laterally as measured against the orbital orbicularis oculi varies: A. Large B. Intermediate C. Small It is thought that with aging the angle becomes smaller with less lateral support to the brow, thereby contributing to lateral brow ptosis
Contributed by Prof. Bhupendra C. K. Patel MD, FRCS
Contributed by Professor Bhupendra C. K. Patel MD, FRCS