Burn Evaluation And Management
- Article Author:
- Timothy Schaefer
- Article Editor:
- Karen Szymanski
- Updated:
- 8/10/2020 9:26:34 PM
- For CME on this topic:
- Burn Evaluation And Management CME
- PubMed Link:
- Burn Evaluation And Management
Introduction
A variety of factors guides the evaluation and management of burns. First is the type of burn such as thermal, chemical, electrical or radiation. Second is the extent of the burn usually expressed as the percentage of total body surface area (%TBSA) involved. Next is the depth of the burn described as superficial (first degree), partial (second degree) or full thickness (third degree). Finally, other factors include specific patient characteristics like the age of the patient (< 10 or > 50 years old); other medical or health problems; if there are specialized locations of the burn (face, eyes, ears, nose, hands, feet and perineum); and if there are any associated injuries, particularly smoke inhalation and other traumatic injuries.[1][2][3][4]
Etiology
Burns may be caused by:
- Abuse
- Chemicals such as strong acids, lye, paint thinner or gasoline
- Electric currents
- Fire
- Hot liquid
- Hot metal, glass or other objects
- Steam
- Radiation from x-rays
- Sunlight or ultraviolet light
Epidemiology
Approximately 86% of burns are caused by thermal injury, while about 4% are electrical and 3% are chemical. Flame and scald burns are the leading cause of burns in children and adults. More adults are injured with flame burns while children younger than five years old are more often injured with scald burns. Burn injuries more commonly affect people of low and middle income and people in low-income countries.
Pathophysiology
Burns are injuries of the skin involving the two main layers - the thin, outer epidermis and the thicker, deeper dermis. There are various types of burns. Chemical burns are divided into acid or alkali burns. Alkali burns tend to be more severe causing more penetration deeper into the skin by liquefying the skin (liquefaction necrosis). Acid burns penetrate less because they cause a coagulation injury (coagulation necrosis). Electrical burns can be deceiving with small entry and exit wounds, however, there may be extensive internal organ injury or associated traumatic injuries. Thermal burns are the most common type of burn. Most burns are small and superficial causing only local injuries. However, burns can be larger and deeper, and patients can also have a systemic response to severe burns.[5][6]
History and Physical
Because most burns are small and classified as minor burns, the history and physical can proceed as usual. If the patient appears to have burns classified as severe, then the approach should be like that of a major trauma patient (see Burns, Resuscitation, and Management chapter). Key factors in the history include the type of burn, possible inhalation injury, and possible associated traumatic injuries. If possible, ask prehospital emergency services providers if the patient had prolonged smoke exposure (consider carbon monoxide poisoning, cyanide poisoning, lung injury) or might have other injuries from explosions, falls or jumping to safety. Examination of the burn can be done in the patient's secondary survey. The patient's clothing should be removed, and the patient should be examined from head to toe in a warm room.
Evaluation
The major factors to consider when evaluating the burned skin are the extent of the burns (usually calculated by the percentage of total body surface area (% TBSA) burned) and the estimated depth of the burns (superficial, partial thickness or full thickness).[7][8][9][10][11]
Extent of the Burn
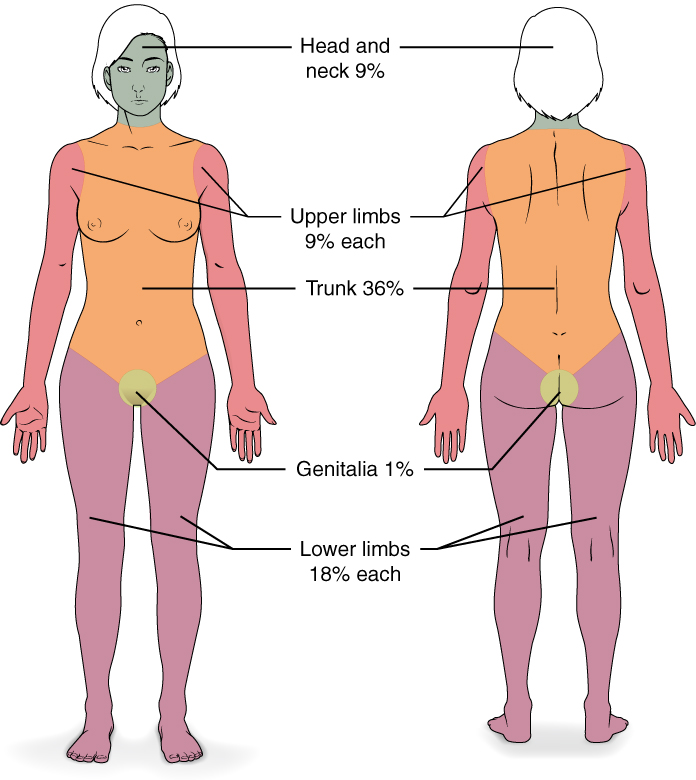
Several methods are available to estimate the percentage of total body surface area burned.
- Rule of Nines - The head represents 9%, each arm is 9%, the anterior chest and abdomen are 18%, the posterior chest and back are 18%, each leg is 18%, and the perineum is 1%. For children, the head is 18%, and the legs are 13.5% each.
- Lund and Browder Chart – This is a more accurate method, especially in children, where each arm is 10%, anterior trunk and posterior trunk are each 13% and the percentage calculated for the head and legs varies based on the patient’s age.
- Palmar Surface - For small burns, the patient's palm surface (excluding the fingers) represents approximately 0.5% of their body surface area, and the hand surface (including the palm and fingers) represents about 1% of their body surface area.
Depth of the Burn
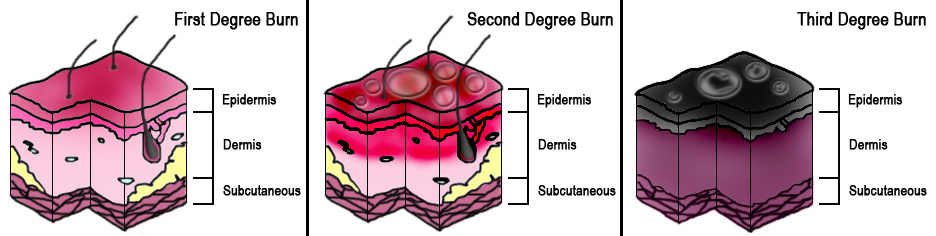
Burn depth is classified into one of three types based on how deeply into the epidermis or dermis the injury might extend.
- Superficial burns (First Degree) involve only the epidermis and are warm, painful, red, soft and blanch when touched. Usually, there is no blistering. A typical example is a sunburn.
- Partial thickness burns (Second Degree) extend through the epidermis and into the dermis. The depth into the dermis can vary (superficial or deep dermis). These burns are typically very painful, red, blistered, moist, soft and blanch when touched. Examples include burns from hot surfaces, hot liquids or flame.
- Full-thickness burns (Third Degree) extend through both the epidermis and dermis and into the subcutaneous fat or deeper. These burns have little or no pain, can be white, brown, or charred and feel firm and leathery to palpation with no blanching. These occur from a flame, hot liquids, or superheated gasses.
When calculating the extent of burn, only partial thickness and full thickness burns are considered, and superficial burns are excluded.
Treatment / Management
The American Burn Association recommends burn center referrals for patients with:
- partial thickness burns greater than 10% total body surface area
- full thickness burns
- burns of the face, hands, feet, genitalia, or major joints
- chemical burns, electrical, or lighting strike injuries
- significant inhalation injuries
- burns in patients with multiple medical disorders
- burns in patients with associated traumatic injuries
Patients being transferred to burn centers do not need extensive debridement or topical antibiotics before transfer. Whether transferring or referring to a burn center, you should contact them before beginning extensive local burn care treatments.[12][13]
Minor burns which you plan to treat can be approached using the “C” of burn care:
- Cooling - Small areas of burn can be cooled with tap water or saline solution to prevent progression of burning and to reduce pain.
- Cleaning – Mild soap and water or mild antibacterial wash. Debate continues over the best treatment for blisters. However, large blisters are debrided while small blisters and blisters involving the palms or soles are left intact.
- Covering – Topical antibiotic ointments or cream with absorbent dressing or specialized burn dressing materials are commonly used.
- Comfort – Over-the-counter pain medications or prescription pain medications when needed. Splints can also provide support and comfort for certain burned areas.
For burns classified as severe (> 20% TBSA), fluid resuscitation should be initiated to maintain urine output > 0.5 mL/kg/hour. One commonly used fluid resuscitation formula is the Parkland formula. The total amount of fluid to be given during the initial 24 hours = 4 ml of LR × patient’s weight (kg) × % TBSA. Half of the calculated amount is administered during the first eight hours beginning when the patient was initially burned. For example, if a 70 kg patient has a 30% TBSA partial thickness burn they will need 8400 mL Lactated Ringer solution in the first 24 hours with 4200 mL of that total in the first 8 hours [(4 mL) × (70 kg) × (30% TBSA) = 8,400 mL LR]. Remember that the fluid resuscitation formula for burns is only an estimate and the patient may need more or less fluid based on vital signs, urine output, other injuries or other medical conditions (see Burns, Resuscitation, and Management for discussion of the management of severely burned patients).
In patients with moderate to severe flame burns and with suspicion for inhalation injury, carboxyhemoglobin levels should be checked, and patients should be placed on high flow oxygen until carbon monoxide poisoning is ruled out. If carbon monoxide poisoning is confirmed, continue treatment with high-flow oxygen and consider hyperbaric oxygen in select cases (see Hyperbaric, Carbon Monoxide Toxicity chapter). Cyanide poisoning can also occur from smoke inhalation and can be treated with hydroxocobalamin (see Inhalation Injury chapter).
Differential Diagnosis
- Aqueous deficiency
- Blepharitis/ Meibomian gland dysfunction
- Goblet cell deficiency/ Mucin deficiency
- Exposure related DTS
Enhancing Healthcare Team Outcomes
The management of burn patients is with an interprofessional team that consists of a surgeon, intensivisit, burn specialist, dietitian, physical therapist, nurses, wound care specialists, pulmonologist and plastic surgeon. Burn patients are best looked after a burn team in a specialized center. The key is to prevent complications and restore functionality. The outcomes of burn patients depends on the degree and extent of the burn. Most second and third degree burns require prolonged admission and recovery is slow. Because cosmesis is significantly altered in burn patients a mental health consult should be made prior to discharge. [14][15]
(Click Image to Enlarge)