Campylobacter
- Article Author:
- Greg Fischer
- Article Editor:
- Elizabeth Paterek
- Updated:
- 8/11/2020 11:34:08 AM
- For CME on this topic:
- Campylobacter CME
- PubMed Link:
- Campylobacter
Introduction
Campylobacter species represent one of the most common causes of bacterial diarrheal illness worldwide. According to the United States Centers for Disease Control, there are about 1.3 million cases of Campylobacter infection each year in the United States alone. This leads to an economic cost between $1.3 to 6.8 billion dollars annually in the United States.[1] Campylobacter infection is associated with the consumption of raw milk, undercooked poultry, and contaminated water. Patients typically experience a self-limited diarrheal illness lasting 5 to 7 days. Immunocompromised and elderly patients are at the highest risk for morbidity, mortality and prolonged illness. Despite having treatment and eradication modalities in place in animal reservoirs, there has been a dramatic increase of cases in developed and underdeveloped regions of the world.[1]
Etiology
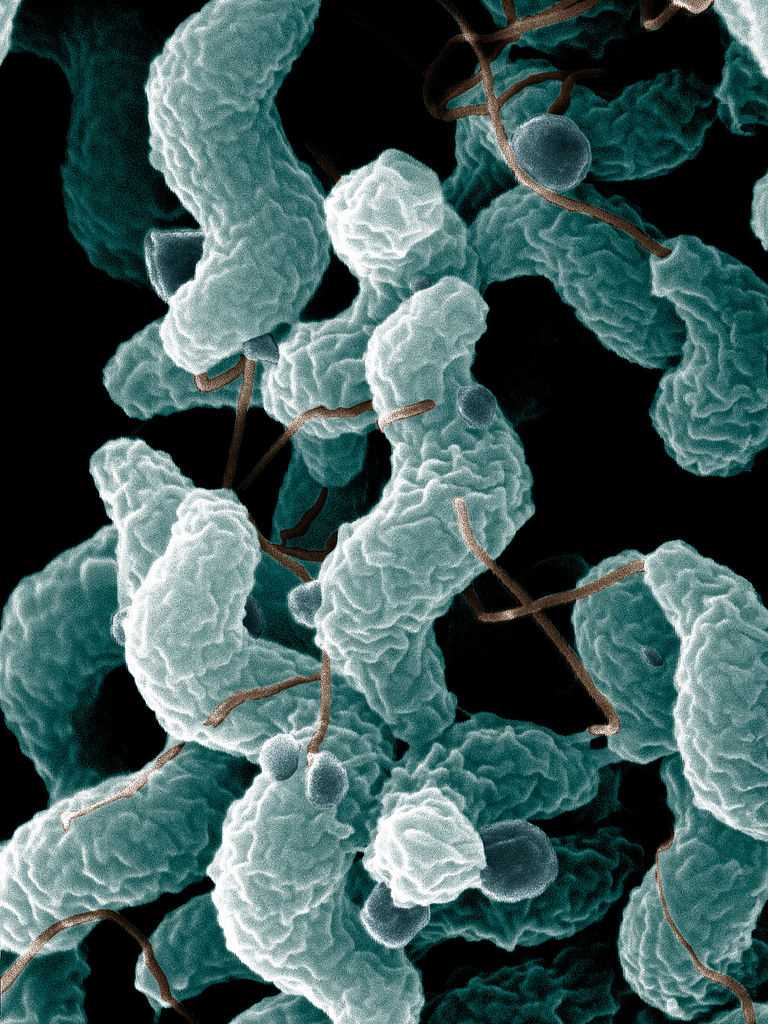
Campylobacter bacteria is a motile, corkscrew-shaped gram-negative rod. They range in size from 0.5 to 5 microns in length by 0.2 to 0.9 microns in width. While there are dozens of species, 3 represent the main sources of human infection: Campylobacter jejuni, Campylobacter coli, and Campylobacter lari. C. jejuni is the most commonly implicated species.[1]
Volunteer controlled studies have highlighted the relative virulence of Campylobacter. Infection with doses as low as 800 CFU can cause symptoms.[2] This virulence highlights the need for cleanliness in those who are in contact with reservoirs of infection such as poultry, contaminated water, and raw dairy.
Epidemiology
Campylobacter is a leading cause of diarrhea in both the developing and the developed world that has become increasingly prevalent. In March 2013, the CDC reported a 14% increase in C. jejuni cases in the United States. One percent of the human population of Europe is affected yearly by campylobacteriosis. In developing countries, Campylobacter isolation rates for food-borne illness are between 5% to 20%. Campylobacteriosis can occur in all age groups though it affects predominately pediatric patients in developing countries. In the developed world, 90% of cases occur during the summer months which is believed to be related to under-cooked meat at outdoor facilities. The condition most commonly affects children under 4 years old and young adults between 15 to 44 years of age.[3]
The worldwide prevalence of the disease highlights the ability of Campylobacter to survive in a wide range of environments. Routes of transmission to humans include consumption of contaminated food and water, contact with animals, and person-to-person contact.[4] With the increasing popularity of international travel of both livestock and humans, the spread of Campylobacter is difficult to control. The CDC has made efforts to educate the public about the signs and symptoms of disease and disease prevention for those traveling to countries that pose a high risk of contact with infected sources. These efforts include hand hygiene, separating raw meats from other food when cooking, the thorough cooking of food and avoidance of raw dairy and untreated water.
History and Physical
Infection from Campylobacter typically manifests as enteritis with voluminous diarrhea. Individuals may experience a prodromal phase of symptoms lasting 1 to 3 days. Symptoms of the prodromal phase include high fever, rigors, dizziness and body aches. This prodromal phase is associated with a more severe disease course. The onset of symptoms typically occurs 24 to 72 hours following ingestion of the bacteria; though it may take longer to develop in individuals infected with smaller amounts of bacteria. The peak of illness generally lasts 24 to 48 hours. The average time for the acute diarrheal phase of Campylobacter enteritis is approximately 7 days. It is not uncommon for symptoms of abdominal pain to persist for days to weeks after resolution of diarrhea.[5] Patients may continue to excrete organisms in the feces for several weeks following clinical improvement though patients receiving antimicrobial therapy appear to have a reduced likelihood of continued excretion.[6]
During the acute phase of the illness, abdominal cramping and multiple episodes of diarrhea are common. Greater than 10 stools per day may occur. Bloody and mucous-like stools are common and result from the of the invasion of the epithelium by the bacteria in the intestine. This leads to inflammatory lesions and mucosal damage. Abdominal pain may mimic appendicitis due to acute ileocolitis.[7] Though pathogenesis is poorly understood, the plasmid pVir is associated with more invasive disease and increased likelihood of bloody diarrhea.[8]
Evaluation
Stool culture, enzyme immunoassay (EIA) or PCR can diagnose Campylobacter infection. For a stool culture, colonies of Campylobacter species are grown using selective culture techniques designed to improve isolation of C. coli and C. jejuni. Both C. jejuni and C. coli are thermophilic, growing best at 42 degrees Celsius and are microaerophilic, growing best in an environment containing 5% to 10% oxygen.[3] EIA and PCR have shown increased sensitivity as compared to stool culture.[9] Recent developments using reverse transcription-polymerase chain reaction (RT-PCR), have allowed for the development of more sensitive tests in screening potentially infected food sources.[10]
Treatment / Management
Infection with Campylobacter is typically self-limiting and mild. The focus of interventions in healthy patients are hydration and electrolyte repletion. Hydration may be oral or parenteral depending on the severity of illness and degree of dehydration. Avoid anti-motility agents as they can impede the resolution of the infection.[11] Antibiotics are not a mainstay of treatment in healthy patients. Consider antibiotics for high-risk patients such as the immunocompromised and the elderly. Those with more severe disease such as fever, bloody stools, or severe abdominal pain may also warrant antibiotics. Immunocompromised patients may require multiple courses of antibiotics.[12]
Campylobacter infections are best treated with macrolide antibiotics.[13] This is due to multiple patterns of antibiotic resistance that have emerged in recent years. Antibiotic use in farm animals is believed to be the source of resistant strains. Campylobacter strains in Canada previously showed an 8.6% resistance to tetracyclines in 1981; this has increased to 56% in more recent studies.[8] Significant resistance pattern to fluoroquinolone therapy has emerged. While in the early 1990s there was almost no fluoroquinolone resistance described in the literature, more recent data in the United States shows 40% fluoroquinolone resistance at one site in the Pennsylvania region.[14] While resistance to macrolide antibiotics has remained low at 1% to 3% in the United States, there is a concern of the eventual development of resistant strains.[14] Patients failing antibiotics therapy require drug susceptibility testing. Research suggests that the emergence of resistant strains comes from widespread antibiotic use in farm animals. Advocacy for judicious antibiotic usage in large-scale farming environments has increased in efforts to control antibiotic resistance.[15]
Differential Diagnosis
The differential diagnosis includes other sources of infectious bacterial diarrhea such as Salmonella, Shigella, Escherichia coli, Listeria, and Clostridium difficile. Viral gastroenteritis such as norovirus may also present similarly.[16] Toxin-mediated food poisoning can present with similar symptoms. Parasitic causes of diarrhea including Giardia lamblia, Cryptosporidium parvum, and Entamoeba histolytica may cause prolonged diarrhea in travelers and immunocompromised patients mimicking Campylobacter.[17]
The abdominal pain from Campylobacter may mimic appendicitis and require advanced imaging such as ultrasound, CT scan, or MRI to differentiate. Inflammatory bowel disease, Crohn's and ulcerative colitis, may also present with abdominal pain and bloody stools. Stool culture, diagnostic imaging, biopsy, and colonoscopy diagnose these chronic conditions.[18]
Prognosis
The overall mortality for Campylobacter infection is 24 per 10,000 culture-confirmed cases. In healthy patients, Campylobacter infections have a self-limited course with excellent clinical outcomes. These patients require supportive care such as electrolyte repletion, oral and parenteral rehydration. Antibiotics should be considered in immunocompromised patients and those with fever, bloody diarrhea, numerous stools or worsening symptoms. Approximately 10.8% of patients require hospitalization, making it the third most common cause of hospitalization for gastroenteritis. Immunocompromised and elderly patients have the highest risks of prolonged and fatal illness. Most patients experience a resolution of illness without complications.[12]
Fewer than 1% of patients experience transient bacteremia, which occurs during the acute infection. Bacteremia is associated with mortality between 2.5 to 12.5%.[19] Immunocompromised and elderly patients are more likely to experience bacteremia.[20] HIV/AIDS patients have an increased incidence of infection with Campylobacter and a more virulent course. These patients may require multiple doses of antibiotic therapy. They are more likely to experience extraintestinal symptoms and have higher mortality.[21]
Complications
There are numerous medical complications associated with Campylobacter infection, many of which have a worse prognosis than the acute infection itself. Campylobacter infections can cause extraintestinal diseases involving the neurologic, pulmonary, immunologic and cardiac systems.
In 1859, the French scientist, Jean-Baptiste Octave Landry, first reported the disease known today as Guillain-Barre syndrome (GBS). GBS is an autoimmune disease that presents with symmetrical ascending flaccid paralysis due to demyelination of peripheral nerves. It was not until the 20th century that a strong association between GBS and Campylobacter was made. Today, it is estimated that Campylobacter, particularly C. jejuni provoke approximately 30% of all GBS. Approximately 1 in every 1000 people infected with Campylobacter will develop GBS. It occurs 1 to 3 weeks after infection with Campylobacter. The mechanism of the autoimmune disease is thought to be through molecular mimicry creating autoantibodies that react with peripheral nerves. The clinical course for those who suffer from GBS varies. Approximately 20% of patients with GBS have a complicated clinical course requiring prolonged intensive care. Despite the advances in the critical care management of GBS, it has mortality between 3% to 7%.[10]
Case reports have emerged of Campylobacter-associated myocarditis and pericarditis. This is most commonly described in young, healthy males with a history of traveling associated diarrheal illness. Patients may experience symptoms ranging from mild chest discomfort to severe pain that mimics myocardial infarction. Laboratory testing often shows elevated Troponin, CK, BNP, and CRP. Increased levels of Troponin T have been associated with a worse prognosis. However, a normal value does not exclude the diagnosis of myocarditis. Echocardiography is used to identify associated pericardial effusions and wall motion abnormalities associated with the condition. In most patients, clinical evolution of symptoms and outcomes are benign. Approximately 30% of those affected develop dilated cardiomyopathy. In severe cases, life-threatening arrhythmias and cardiovascular collapse requiring extracorporeal membrane oxygenation (ECMO) have been described.[22]
Approximately 1% to 5% of patients will experience acute reactive arthritis with an annual incidence of 4.3 per 100,000. Young adults are the most commonly affected group. Both C. jejuni and C. coli are associated with the condition. Symptoms begin within the 4 weeks following acute infection, and predominant symptoms are a sterile joint inflammation. Symptoms vary from mild oligo-arthralgia to disabling polyarthritis. Musculoskeletal symptoms are the most common presentation though patients can also have ocular, dermatological and urinary symptoms. While symptoms most commonly affect the knees and ankles, small joints and tendons involvement is also seen. The duration of symptoms in acute reactive arthritis is variable. Patients may experience symptoms lasting several months to a year. There is no association with HLA B27 on a population level.[23][24]
In the gastrointestinal (GI) system, there has been an increased association of esophageal and colorectal diseases with Campylobacter infections. In the acute phase of the disease, severe infections can manifest as colitis which can lead to significant morbidity occasionally requiring surgical intervention. Toxic megacolon is a rare complication of Campylobacter colitis and should be considered in critically ill patients. Patients that develop toxic megacolon have high morbidity and mortality despite interventions.[25]
Multiple other gastroenterological manifestations are associated with Campylobacter including, gastroesophageal reflux disease (GERD), Barrett's esophagus (BE), and esophageal adenocarcinoma. Research has also shown there an increased risk for colorectal carcinoma and irritable bowel disease following Campylobacter infections.[26]
A form of lymphoma, immunoproliferative small intestinal disease, has shown an association with Campylobacter infections. Biopsy specimens several patients noted the presence of C. jejuni and antimicrobial therapy targeting this organism lead to the rapid remission of the immunoproliferative small intestinal disease.[27]
Deterrence and Patient Education
The most commonly reported sources for Campylobacter infections are under-cooked poultry in the developed world and contaminated water in the developing world. Ensuring poultry and meat is thoroughly cooked at 70 C before ingestion decreases the risk of infection. The CDC recommends, washing items that come into contact with raw poultry. They also recommend separate cutting boards for raw meat and cleaning utensils after they contact raw meat.[1] Unpasteurized milk and cheese should be avoided. Untreated water should not be consumed. Practicing basic hand hygiene decreases the risk of infection.[28]
Pearls and Other Issues
- Campylobacter is a leading cause of food-borne illness worldwide. C. jejuni is most identified as being the most common culprit in human infections
- Campylobacter is a robust species of bacteria that can survive over a wide range of environments. Small numbers of the bacteria can cause infection.
- Those who are at greatest risk for infection include international travelers, people who come in frequent contact with livestock, particularly poultry, and consumers of untreated water or unpasteurized milk.
- Clinically, Campylobacter infection typically manifests as diarrhea (sometimes bloody) that typically peaks 1 to 2 days following onset. The acute enteritis phase of the infection is typically self-limiting and resolves after 7 days.
- Stool culture, PCR, or EIA establishes the diagnosis.
- Campylobacter is typically self-limiting, and some cases require supportive fluid and electrolyte replenishment. When antibiotics are needed, macrolides such as azithromycin are the treatment of choice.
- There are multiple complications related to Campylobacter infection; most notably, there is an associated with infection and Guillain-Barre syndrome.
Enhancing Healthcare Team Outcomes
Recent outbreaks of campylobacter underline the importance of epidemiologic reporting and preventative measures. In 2018, there was a multi-state outbreak of Campylobacter with a reported 113 laboratory-confirmed cases spanning over 17 states. This outbreak led to 23 hospitalizations with no reported deaths. During interviews with the patients, those affected answered a survey of questions regarding recent contact with animals and food. Questionnaires revealed that 87% of those affected reported contact with a puppy from the same branch of stores. Using a method of gene sequencing called Whole Gene Sequencing, biologists isolated genetic sequences that proved the samples were related. This established a common source. Isolates were tested for antibiotic sensitivities, and a pattern of resistance was identified. The infection was contained using practices of identifying the pathogen, tracing its source, and providing recommendations for treatment.