Carpal Tunnel Syndrome
- Article Author:
- Justin Sevy
- Article Editor:
- Matthew Varacallo
- Updated:
- 8/10/2020 5:20:26 PM
- For CME on this topic:
- Carpal Tunnel Syndrome CME
- PubMed Link:
- Carpal Tunnel Syndrome
Introduction
Carpal tunnel syndrome (CTS) is an entrapment neuropathy caused by compression of the median nerve as it travels through the wrist's carpal tunnel. It is the most common nerve entrapment neuropathy, accounting for 90% of all neuropathies. Early symptoms of carpal tunnel syndrome include pain, numbness, and paresthesias. These symptoms typically present, with some variability, in the thumb, index finger, middle finger, and the radial half (thumb side) of the ring finger. Pain also can radiate up the affected arm. With further progression, hand weakness, decreased fine motor coordination, clumsiness, and thenar atrophy can occur.
In the early presentation of the disease, symptoms most often present at night when lying down and are relieved during the day. With further progression of the disease, symptoms will also be present during the day, especially with certain repetitive activities, such as when drawing, typing, or playing video games. In more advanced disease, symptoms can be constant.
Typical occupations of patients with carpal tunnel syndrome include those who use computers for extended periods of time, those who use equipment that has vibration such as construction workers, and any other occupation requiring frequent, repetitive movement. [1] [2] [3]
Etiology
Carpal tunnel syndrome results from increased pressure carpal tunnel pressure and subsequent compression of the median nerve. The most common causes of carpal tunnel syndrome include genetic predisposition, history of repetitive wrist movements such as typing, or machine work as well as obesity, autoimmune disorders such as rheumatoid arthritis, and pregnancy. [4]
Epidemiology
In the United States, carpal tunnel syndrome has an incidence of 1 to 3 persons per 1000 per year, with a prevalence of 50 per 1000, with similar incidence and prevalence in most developed countries. It most commonly affects whites, has up to a 10 to 1 predominance in females, and has a peak age of 46 to 60. [5]
Pathophysiology
Carpal tunnel syndrome (CTS) is multifactorial and often results from multiple patient-specific, occupational, social, and environmental risk factors. A single, specific cause is not always determined unless there is, for example, a space-occupying lesion that can be attributable to patient-reported symptoms. While this can be appreciated in select medical conditions (e.g., gout), these relatively straightforward clinical presentations are relatively uncommon in comparison to most presentations of CTS.
In general, the pathophysiology of CTS results from a combination of compression and traction mechanisms. The compressive element of the pathophysiology includes a detrimental cycle of increased pressure, obstruction of overall venous outflow, increasing local edema, and compromise to the median nerve's intraneural microcirculation. Nerve dysfunction becomes compromised, and the structural integrity of the nerve itself further propagates the dysfunctional environment-- the myelin sheath and axon develop lesions, and the surrounding connective tissues become inflamed and lose normal physiologic protective and supportive function. Repetitive traction and wrist motion exacerbates the negative environment, further injuring the nerve. In addition, any of the nine flexor tendons traveling through the carpal tunnel can become inflamed and compress the median nerve. [6]
History and Physical
Patients often report numbness, tingling, and pain that increase at night. Weakness, clumsiness, and temperature changes also are common complaints. The thumb, digits 2 and 3, and the radial half of digit 4 are typically affected. Patients with carpal tunnel syndrome often will have a positive "flick sign," meaning that symptoms improve when they flick their hand and wrist. Patients often find some relief with ice, rest if provoked by repetitive activity, and night splints.
Evaluation
Electromyography and nerve conduction studies are the basis for carpal tunnel syndrome diagnosis. Other clinical or special exams do not confirm carpal tunnel syndrome but do assist in ruling out other diagnoses. These findings can prompt electromyography and nerve conduction studies.
The clinical physical exam may include testing for sensory and motor deficits and evidence of thenar wasting. There are several special tests with varying degrees of sensitivities and specificities.
- The best of these include the carpal compression test. This is done by applying firm pressure directly over the carpal tunnel for 30 seconds. The test is positive when paresthesias, pain, or other symptoms are reproduced.
- The square sign test is an evaluation to determine the risk of developing carpal tunnel syndrome. The test is positive if the ratio of the thickness of the wrist divided by the width of the wrist is great than 0.7.
- Another test is a palpatory diagnosis. In this test, the health care provider examines soft tissue over the median nerve for mechanical restriction.
- The Phalen's test or ‘reverse prayer’ is performed by having the patient fully flex their wrists by placing dorsal surfaces of both hands for one minute. A positive test is when symptoms (numbness, tingling, pain) are reproduced.
- The reverse Phalen's, or ‘prayer test,’ is done by having the patient extend both of their wrists by placing palmar surfaces of both hands together for 1 minute (as if praying). Again a positive test is with the reproduction of symptoms.
- Although a low sensitivity and specificity, the Hoffmann-Tinel sign is another test commonly performed. In this test the healthcare professional taps immediately over the carpal tunnel to stimulate the median nerve. Like the above tests, a positive test is when symptoms are reproduced.
Treatment / Management
If carpal tunnel syndrome is identified early, conservative treatment is recommended. Initially, the patient should be instructed in modifying symptom provoking wrist movement. This can be through proper hand ergonomics such as placing the keyboard at a proper height and minimizing flexion, extension, abduction, and adduction of the hand when typing. It should be recommended to decrease repetitive activities if possible. Counseling on weight loss and increased aerobic activity also can be beneficial. A properly fitted nighttime wrist splint can be offered. An occupational therapist trained in hand therapy also may be a beneficial referral. Combined therapy may be more beneficial than any single treatment. A short course of nonsteroidal anti-inflammatory medication can relieve symptoms but some do not feel it of adequate benefit.
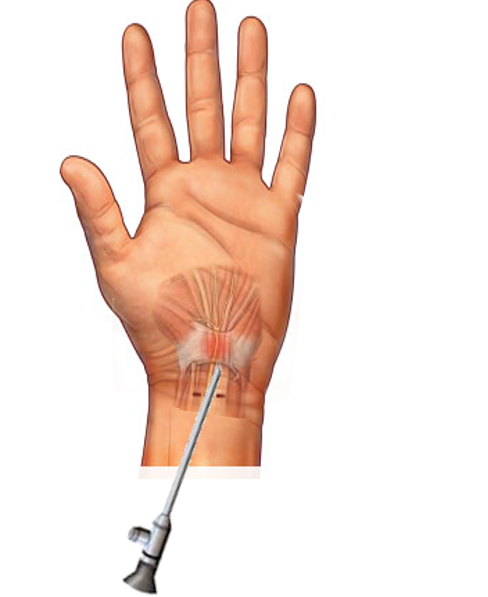
If conservative treatments are not successful, an oral or local glucocorticoid could be offered. The definitive treatment for persistent carpal tunnel syndrome is a surgical intervention with carpal tunnel release after nerve conduction studies showing significant axonal degeneration. Carpal tunnel release typically is performed by a neuro/orthopedic/plastic surgeon or hand surgeon. This procedure can be performed either open or endoscopically. Carpal tunnel release is considered a minor surgery in which the transverse carpal ligament or flexor retinaculum is cut, opening more space in the carpal tunnel and decreasing pressure on the median nerve. It does not typically require overnight hospitalization. [7] [8] [9]
Differential Diagnosis
- Cervical radiculopathy
- Neuropathies
- Tendonitis
- Tenosynovitis
Pearls and Other Issues
The carpal tunnel includes the median nerve and nine flexor tendons. The flexor tendons include the four tendons from the flexor digitorum profundus, four tendons from the flexor digitorum superficialis, and one tendon from the flexor pollicis longus. The transverse carpal ligament (flexor retinaculum) makes up the superior boundary, and the carpal bones form the inferior border.
Enhancing Healthcare Team Outcomes
The diagnosis and management of carpal tunnel syndrome are done with an interprofessional team that includes the primary caregiver, nurse practitioner, physical therapist, neuro/orthopedic/plastic surgeon, and the emergency department physician. The initial treatment is usually conservative combined with limiting repetitive activities. A properly fitted nighttime wrist splint can be offered. An occupational therapist trained in hand therapy also may be a beneficial referral. Combined therapy may be more beneficial than any single treatment. A short course of nonsteroidal anti-inflammatory medication can relieve symptoms but some do not feel it is of adequate benefit.
Many other treatments are available to treat carpal tunnel syndrome including surgery. An orthopedic specialty nurse can assist at all phases of care, regardless of whether treatment is conservative or surgical. While surgery can relieve symptoms, recurrence is not uncommon. The patient must be fully educated about the potential complications of surgery which should only be undertaken after conservative treatments have failed. An interprofessional team approach will lead to better outcomes for patients with CTS. [Level 5][10][11] (Level V)