Choroid Plexus Papilloma
- Article Author:
- Jijo Joseph
- Article Editor:
- Joe M Das
- Updated:
- 10/13/2020 11:38:44 AM
- For CME on this topic:
- Choroid Plexus Papilloma CME
- PubMed Link:
- Choroid Plexus Papilloma
Introduction
Choroid plexus papillomas (CPPs) are rare central nervous system tumors. They may be seen at any age, but are more common in infants. Their site of occurrence varies according to age. They usually present with the increasing head circumference or altered mental status in children; whereas in adults they present with signs of increased intracranial tension. Imaging shows intraventricular enhancing masses. Surgery is the therapeutic intervention of choice for these lesions. They have a good prognosis in spite of their size as they are benign. Improvements in surgical techniques and intensive care have improved survival.
Etiology
Studies have shown that Simian virus (SV) 40 has an association with the occurrence of choroid plexus tumors.[1] BK virus and John Cunningham (JC) viruses have also been implicated.[2] Binding of the large T antigen with both p53 and pRb tumor suppressor proteins, forming complexes, has been demonstrated in humans harboring choroid plexus tumors.[2] Current data do not, however, support a causative role. No other causative factor is presently under research.
Epidemiology
Choroid plexus papillomas are rare tumors of neuroectodermal origin. In the pediatric population, they form the third most common congenital brain tumors, after teratomas and gliomas, and account for 0.4 to 0.6% of all intracranial neoplasms.[3] This lesion is generally a disease of childhood, with a median age at diagnosis of 3.5 years. Typically in infants, their location is supratentorial, within the lateral ventricles (most commonly in the atrium).[4] In adults, the preferred site is the fourth ventricle.[5] The cerebellopontine angle is a rare location in adults.[5]
Pathophysiology
According to the 2016 World Health Organization classification,[6] choroid plexus tumors are classified as papillomas (grade I), atypical tumors (grade II), and carcinomas (grade III). Choroid plexus papillomas have less than two mitotic figures per 10 high power fields, atypical ones have two to five per 10 high power fields, and carcinomas have greater than five mitotic figures per 10 high power fields. Grossly, the tumors are soft, globular, friable pink masses with irregular projections and high vascularity.
Histopathology
Microscopy shows papillary fronds lined by bland columnar epithelium. Mitotic activity, nuclear pleomorphism, and necrosis are typically absent.[7]
On immunohistochemistry, tumors are positive for cytokeratin, vimentin, podoplanin, and S-100.[8][7] Glial fibrillary acidic protein (GFAP) may be positive in up to 20% of cases of choroid plexus papilloma.[9] Studies have shown that older patients (above 20 years) express more GFAP and transthyretin than younger patients and fourth ventricle tumors express more S100 than lateral ventricle tumors.[10]
Genetic analyses have reported germline mutations in the TP53 gene in some patients with choroid plexus papilloma.[11] Rarely these tumors show positive nuclear staining for p53 protein. Syndromic associations of choroid plexus papilloma include Aicardi syndrome, hypomelanosis of Ito, and 9p duplication.
History and Physical
Patients typically present with a history of gradual deterioration. Signs of raised intracranial tension, like vomiting, headache, lateral gaze palsies, homonymous visual field defects, reduced mentation, and so on are usually evident. Sometimes the patient may develop subarachnoid hemorrhage due to bleeding from the tumor. Infants present with increasing head circumference or poor feeding or both, along with upgaze palsy, reduced activity, and altered consciousness.
The clinical symptoms are predominantly due to hydrocephalus[12], as a result of direct mechanical obstruction to flow of cerebrospinal fluid (CSF) due to an arachnoid granulation blockage from hemorrhage or CSF overproduction.[13] Though benign, studies exist showing a rapid growth in tumor size.[14]
Evaluation
If fontanelles are not fused, neurosonogram (NSG) through the anterior fontanelle will demonstrate an echogenic lesion within the ventricles. This lesion continues to demonstrate bidirectional flow throughout diastole, indicating blood flow through vessels arranged chaotically.
Computerized tomography (CT) shows an isodense or slightly hyperdense lesion within the ventricles along with consequent ventriculomegaly.[15] Hydrocephalus is typical. About 25% of the patients have calcification. The lesions are lobulated with slightly irregular margins. They also show intense and somewhat heterogeneous contrast enhancement. Angiographic and cross-sectional imaging show enlargement of the choroidal artery.
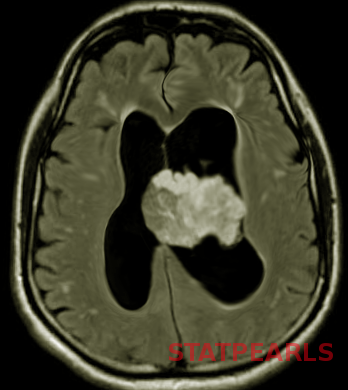
Magnetic resonance imaging (MRI) reveals the well–defined, frond-like intraventricular lobulated masses, which are hypointense on T1WI and hyperintense on T2WI.[16] Flow voids are seen, indicating active blood flow. The lesions are brilliantly enhancing, owing to rich vascularity. There are recent studies with the use of arterial spin labeling that can help distinguish choroid plexus papilloma from choroid plexus carcinoma.[17]
Treatment / Management
In incidentally detected tumors, there is controversy regarding the timing of surgery.[18] Prompt surgical removal may be one option, or surgery may be withheld until follow up imaging shows radiographic changes or hydrocephalus, or surgery may be an option once the patient becomes symptomatic. Once hydrocephalus develops it is easier to resect the tumor, as the length of the corridor to the ventricles reduces, and space around the tumor increases. The disadvantage of such a policy is that patients may develop focal deficits from mass effect, subarachnoid hemorrhage, or seizures. Also, as tumors grow patients tend to develop cognitive defects.[19]
In symptomatic patients, gross total resection (GTR) is the treatment of choice as these tumors are benign. Recent advances in imaging, surgical approaches, and quality of intensive care have improved surgical outcomes with the chances of a cure reaching almost 100%.[4] In the pediatric population, there is significant (12%) perioperative mortality, mainly from catastrophic blood loss.[20] Preoperative embolization can minimize this risk, along with optimization of the ability to resect the tumor completely.[21] Radiosurgery may be a possible treatment option, but further studies are required to determine its efficacy.[22] There have also been attempts at percutaneous stereotactic intratumoral embolization with a sclerosing agent, to reduce blood flow and improve tumor resectability.[23]
Adjuvant chemotherapy, though limited in use, can prevent recurrence and prolong survival.[24] A growing residual choroid plexus papilloma may be treated by irradiation, followed by subtotal resection, providing an even higher chance of success. Adjuvant therapy is also necessary for malignant tumors and those that have shown leptomeningeal spread.[25] Recent studies show an increasing role of bevacizumab in disseminated choroid plexus papilloma.[26]
Differential Diagnosis
Differentials for choroid plexus papilloma include[27]:
- Intraventricular tumors such as papillary ependymoma
- Central neurocytoma
- Subependymal giant cell tumor
- Subependymoma
- Choroid plexus tumors
- Medulloblastoma
- Meningioma
- Chordoid glioma
- Rosette-forming glioneuronal tumor
- Central nervous system lymphoma
- Metastasis
Prognosis
Improvements in surgical and intensive care techniques have vastly improved the prognosis of patients.[28] Maximum tumor resection correlates with an increase in both progression-free survival and overall survival.[29] Recurrences are rare. Suprasellar metastases and craniospinal seeding, though rare, have been reported.[30]
Complications
At presentation, children may have features of prolonged raised intracranial pressure such as papilledema, optic atrophy, and visual loss, which may not recover after surgery.[31] Some may develop cognitive defects, bleeding, and seizures that may persist postoperatively.[32][18]
Intraoperatively there are high chances for excessive blood loss due to rich vascularity.[21]
There have also been reports of postoperative CSF rhinorrhoea.[33]
Deterrence and Patient Education
Any child presenting with altered sensorium has to be evaluated for an intraventricular tumor and managed with surgery to improve survival.
Enhancing Healthcare Team Outcomes
Management of choroid plexus papilloma requires an interprofessional team that includes the neurosurgeon, various specialists (e.g., anesthetist, pediatrician, ophthalmologist, neurologist), and neuroscience specialty-trained nurses. It is vital to educate the parents that even though these lesions are benign, complications can occur during surgery. A thorough discussion between the neurosurgeon and family should take place on the optimal procedure for the child. With adequate preparation of the child, the outcomes are excellent.[34]