
Anatomy, Head and Neck, Eye Ciliary Muscles
- Article Author:
- Ibraheem Rehman
- Article Author:
- Navid Mahabadi
- Article Editor:
- Tayyeba Ali
- Updated:
- 8/10/2020 5:48:45 PM
- For CME on this topic:
- Anatomy, Head and Neck, Eye Ciliary Muscles CME
- PubMed Link:
- Anatomy, Head and Neck, Eye Ciliary Muscles
Introduction
Vision is perhaps the most useful of the senses for humans. More than 50% of the sensory receptors in the human body are located in the eyes, and a significant portion of the cerebral cortex is devoted to interpreting visual information. The eyes are responsible for detecting visible light, with wavelengths ranging from 400 to 700 nanometers. As objects absorb and reflect various wavelengths of light, they appear as they reflect. For example, an object appears white if it reflects all wavelengths of light, and it appears black if it absorbs all wavelengths of light. The ciliary muscle is an important part of the eye that contributes to a person's ability to view objects clearly at varying distances.[1][2][3][4]
Structure and Function
The middle layer of the eyeball, called the vascular tunic, is composed of the choroid, ciliary body, and iris. In the anterior section of the vascular tunic, the choroid becomes the ciliary body. It extends from a jagged margin of the retina to a point just behind the junction of the sclera and the cornea. The jagged anterior portion at which the ciliary body begins is called the ora serrata. The ciliary body appears as dark brown because of the melanocytes that it produces. Furthermore, it consists of ciliary processes and ciliary muscles. The ciliary processes are protrusions on the internal surface of the ciliary body. These protrusions, or folds, contain blood capillaries that secrete aqueous humor. Extending from the ciliary processes are zonular fibers. These fibers act as suspensory ligaments that attach to the lens. The zonular fibers are in contact with the ciliary muscle, which is a circular band of smooth muscle that controls the tightness of the zonular fibers. The ciliary muscle alters the tightness of the zonular fibers by contracting and relaxing, thereby altering the shape of the lens and leading to the adaptation to near or far vision.[5][6][7][8]
Embryology
Eye formation begins approximately three weeks into human embryonic development and continues through the tenth week. Cells from ectodermal and mesodermal tissues contribute to this development. Specifically, the eye is derived from the neuroepithelium, the surface ectoderm, and the extracellular mesenchyme (neural crest and mesoderm). The neural tube ectoderm gives rise to the ciliary body, including both the ciliary processes and ciliary muscle.
Blood Supply and Lymphatics
Various branches of the ophthalmic artery provide the eye's blood supply, including the central artery of the retina, short and long posterior ciliary arteries, and the anterior ciliary arteries. Six to 12 short posterior ciliary arteries arise from the ophthalmic artery as it crosses the optic nerve. They supply blood to the ciliary processes. Two long posterior ciliary arteries pass through the posterior portion of the sclera at a close distance to the optic nerve. They supply blood to the choroid and ciliary muscle. Seven anterior ciliary arteries supply the conjunctiva, sclera, and rectus muscles. Six extrinsic eye muscles move each eye: the superior rectus, inferior rectus, lateral rectus, medial rectus, superior oblique, and inferior oblique. These muscles are important for moving the eyes as they place an image on the fovea to get maximum resolution.
The ciliary muscle also contracts and relaxes its longitudinal fibers to increase and decrease the size of the pore in the trabecular meshwork. The trabecular meshwork is responsible for aqueous humor drainage in the anterior portion of the eye. Changing the pore size can impede or facilitate aqueous humor flow in the canal of Schlemm.
Nerves
Short ciliary muscles that arise from the ciliary ganglion innervate the ciliary muscle. The ciliary ganglion is a parasympathetic ganglion that is located behind the eye and contains about 2500 neurons. These parasympathetic fibers arise from cranial nerve V, also known as the nasociliary nerve of the trigeminal. Activation of the M3 muscarinic receptors, acetylcholine receptors that are formed by G-protein complexes, trigger the contraction of the ciliary muscle and reduce the diameter of the ciliary muscle ring. Contraction allows the zonular fibers to relax and the lens becomes more spherical to improve near vision.
Clinical Significance
The eyeball is a complex structure with many small organs that are essential for vision and movement of the eye. An injury to any part of the eye can result in discomfort, reduced vision, and in some cases blindness. The eye is a source of injury, infection, and multiple medical diseases. It is important for all health practitioners to be able to identify and describe the anatomical features of the eye. The ciliary muscle is an important part of the eye that controls aspects of near and far vision.[9][10]
Glaucoma is an eye disease that damages the optic nerve and can eventually lead to blindness. Increased ocular pressure often causes the damage to the optic nerve. A clear fluid constantly flows out of the anterior chamber of the eye to maintain intraocular pressure. The drainage occurs at the angle where the cornea and iris meet. In open-angle glaucoma, the drainage angle is open, but the fluid is passing through the meshwork too slowly, resulting in increased pressure. It is important to understand that an increase in intraocular pressure does not always lead to glaucoma because certain individuals can tolerate higher pressures. Also, the increased intraocular pressure is not necessary for developing glaucoma. It is possible through increased blood pressure. Individuals most at risk for glaucoma are African Americans above the age of 40, all individuals over the age of 60, and anyone who has a family history of the condition.
In angle-closure glaucoma, the iris presses against the meshwork and inhibits drainage of the aqueous humor out of the anterior chamber of the eye. This causes a rapid increase in intraocular pressure. Both open-angle and closed-angle glaucoma can be treated with muscarinic receptor agonists, such as pilocarpine, that cause the ciliary muscle to contract and leads to the opening of the trabecular meshwork. Once the pores in the trabecular meshwork have opened, the aqueous humor can flow through the canal of Schlemm and eventually lead to a decrease in intraocular pressure.
The contraction of the ciliary muscle can lead to relief in both open-angle and closed-angle glaucoma, making it a target for drugs like pilocarpine.
(Click Image to Enlarge)
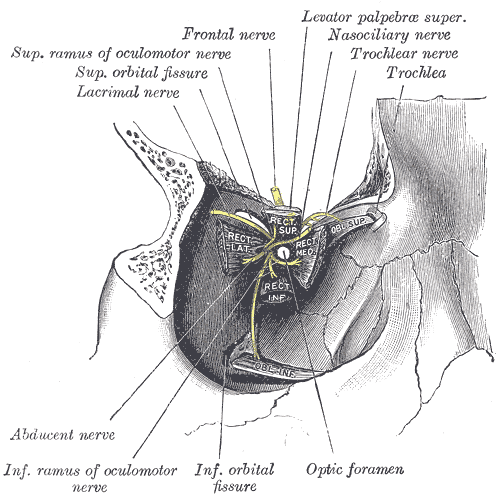
The Accessory Organs of the Eye, Dissection showing origins of right ocular muscles, and nerves entering by the superior orbital fissure, Superior Ramus of Oculomotor nerve, Superior Orbital fissure, Lacrimal nerve, Frontal nerve, Levator palpebrae superior, Nasociliary nerve, Trochlear nerve, Trochlear, Abducens nerve, Inferior ramus of oculomotor nerve, Inferior orbital fissure, Optic foramen
Contributed by Gray's Anatomy Plates
(Click Image to Enlarge)
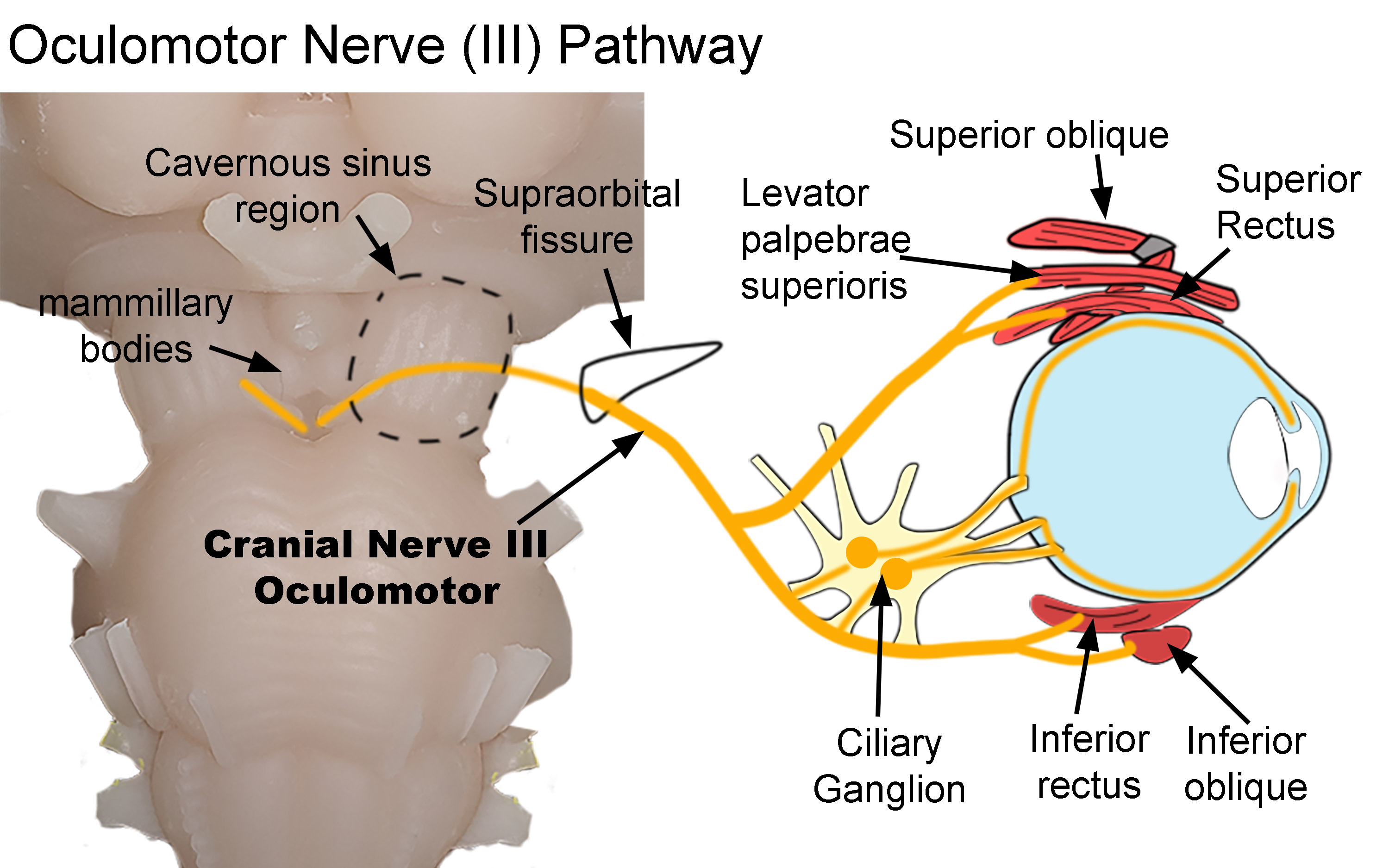
Pathway of the Oculomotor Nerve (III). Diagram shows the pathway of the oculomotor nerve as it exits the brainstem and terminates within the orbit. After exiting the brainstem, it traverses both the cavernous sinus (dotted line) and supraorbital fissure (black line) before entering the orbit. Parasympathetic nerves synapse within the ciliary ganglion. Postganglionic nerves then innervate the sphincter papillae and ciliary muscles. Somatic nerves innervate the superior oblique, levator palpebrae superioris, superior rectus, inferior rectus, and inferior oblique muscles.
Created by Diana Peterson, Ph.D. for use with StatPearls.