Cornea Transplantation
- Article Author:
- Panayiotis Maghsoudlou
- Article Author:
- Gitanjli Sood
- Article Editor:
- Hossein Akhondi
- Updated:
- 7/31/2020 3:20:12 PM
- For CME on this topic:
- Cornea Transplantation CME
- PubMed Link:
- Cornea Transplantation
Introduction
Corneal disease ranks as the fifth leading cause of blindness in the world.[1] Keratoplasty is the most common and successful transplantation in humans with the first transplant completed in 1905.[2]
History of Corneal Transplantation
Modern corneal transplantation techniques represent the culmination of centuries of ideas, experimentation, and perseverance. The French surgeon Pellier de Quengsy was the first to suggest the use of a transparent material to replace an opaque cornea in 1789.[3] Transplantation with xenografts was first postulated by Karl Himley in 1813 and attempted, experimentally and without success, by his student Franz Reisinger in 1824. Richard Kissam performed the first therapeutic corneal xenograft with a porcine cornea in 1838. The first successful human allograft and penetrating keratoplasty (PK) followed developments in anesthetics and antiseptic surgery and was performed by Eduard Zirm in December 1905 on a 45-year-old farm laborer with lime burns.[4][5]
Recent Developments
Scientific advances in immunology, surgical technique, and tissue banking have shaped corneal transplantation into the field it is today.[6][7] The last 20 years have brought significant developments in selective endothelial replacement that have brought about considerable shifts in the field.
Gerrit Melles described a posterior lamellar keratoplasty (PLK), whereby only a portion of the cornea was transplanted. Following an incision at the limbus, the endothelium, Descemet’s membrane (DM) and posterior stroma were dissected out and replaced by a donor button consisting of the same corneal layers that were held in place by an air bubble.[8] Mark Terry modified the PLK in 2001, including the use of viscoelastic material instead of an air bubble and renamed the procedure deep lamellar endothelial keratoplasty (DLEK).[9] In 2004 Gerrit Melles modified the technique further by only removing the host endothelium and DM (i.e., descemetorhexis), obviating the need for stromal dissection, and replacing with a donor button of endothelium, DM and stroma (Descemet’s stripping endothelial keratoplasty; DSEK) with further modification for automated donor dissection using a microtome (Descemet’s stripping automated endothelial keratoplasty; DSAEK).[10][11][12] In 2006 the technique was further developed by only transplanting a donor button of endothelium and DM without the posterior stroma (Descemet’s membrane endothelial keratoplasty; DMEK).[13] Minor modifications include automated posterior lamella dissection similar to DSEK (Descemet’s membrane automated endothelial keratoplasty; DMAEK).[14]
A selective keratoplasty technique that relates to the anterior cornea is the deep anterior lamellar keratoplasty (DALK), whereby a donor button replaces the epithelium, Bowman's layer, and stroma.[15]
Anatomy and Physiology
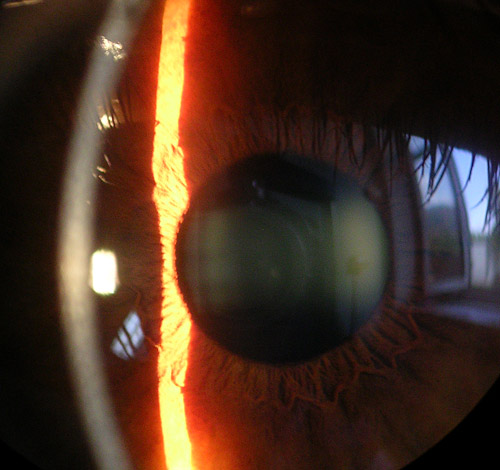
Macroanatomy
The cornea is a transparent avascular structure that protects structures inside the eye and contributes to two-thirds of its refractive power. The cornea is convex, has a diameter of approximately 11.5 mm, and increases in thickness from the center (550-565 μm) to the periphery (610-640 μm).[16] The cornea is densely innervated by long ciliary nerves that originate in the ophthalmic division of the trigeminal nerve.
Microanatomy
The layers anteroposteriorly include the epithelium, Bowman’s layer, stroma, Descemet’s membrane, and endothelium.[17]
The epithelium is the main barrier to the eye, provides a smooth optical surface and performs immunological functions. It consists of 5 to 7 cell layers in the center and 7 to 10 cell layers in the periphery, with an approximate thickness of 50 μm. The limbal stem cell hypothesis suggests the proliferation of stem cells and transient amplifying cells in the periphery with central migration to replace cells lost on the surface.[18]
Bowman’s layer is a tough tissue composed of primarily type I and V collagen and is an acellular condensate of the stroma. It contributes to the corneal shape.
The corneal stroma provides mechanical strength and refractive power and consists of regularly arranged collagen fibers, glycosaminoglycans, and interconnected keratocytes, in packed layers or lamellae. At the corneal center, there are 200 lamellae, with a much higher packing density and interconnectivity in the anterior area compared to the posterior. In DSEK/DSAEK, when the air bubble is introduced to separate the endothelium and DM part of the posterior stroma adheres to the DM, suggesting a natural cleavage plane in the stroma ten μm above the DM.[19] There have been suggestions that this area of the posterior stroma is anatomically distinct and has been named pre-Descemet’s layer or Dua’s layer.[20]
DM is a 7-10 micrometer structure that consists of Type IV collagen and laminin and is secreted by endothelial cells continuously.[21] The corneal endothelium is a simple cuboidal monolayer of cells that are rich in mitochondria and are responsible for maintaining transparency.
Indications
Penetrating keratoplasty indications include keratoconus, ectasias, corneas degenerations, dystrophies, keratitis, congenital opacities, chemical/mechanical corneal trauma, and re-grafts. The reported leading indications in a region are dependent on sociopolitical, geographical and economic factors and may not accurately reflect the most common aetiologies of corneal pathology.[22]
Endothelial keratoplasty (EK) includes PLK, DLEK, DSEK, DSAEK, DMEK, and DMAEK. EK procedures are not appropriate for patients with healthy corneal endothelium such as keratoconus. EK indications include: Fuch’s endothelial dystrophy, posterior polymorphous dystrophy, congenital hereditary endothelial dystrophy, bullous keratopathy, iridocorneal endothelial syndrome, and failed EKs.
Deep anterior lamellar keratoplasty (DALK) indications include those that relate to the pathology of the anterior cornea (epithelium, Bowman’s layer, and stroma), such as keratoconus and corneal scars.
Contraindications
There are absolute and relative contraindications for corneal transplantation in each country that are highly region-dependant. The National Health Services (NHS) Blood and Transplant Agency in the United Kingdom (UK) has the following absolute contraindications: transplant unlikely to restore corneal function or integrity or remove tissue that would otherwise have led to further damage to the eye.
Equipment
Basic operating room equipment is usually necessary with the arrangement for local anesthesia (e.g., retrobulbar block) alongside intravenous sedation or general anesthesia.
Personnel
Personnel involved consists of the operating surgeon, assistant, anesthesiologist, and nursing staff.
Preparation
The procedure must be described to the patient, with sufficient time provided to understand and weigh the risks and benefits, following which informed consent is sought. A history, including current medication and allergies, and ophthalmic examination is performed prior to the procedure. Many patients who are candidates for this procedure are older and have comorbid conditions and advice should be given to them regarding their anti-diabetic, anti-thrombotic, and other medication. Many health care organizations have guidelines, protocols or instructions regarding such medication and stopping/continuing them pre-operatively that patients can follow. Phone numbers should be given to contact in case there are any post-operative issues, and transport arranged with a next of kin for care following the procedure.
Technique
Penetrating Keratoplasty
Following the establishment of anesthesia, an eyelid speculum is inserted, and the patient’s eye is secured using a scleral fixation ring or sutures. The host corneal diameter is measured to determine the appropriate size for the donor button. The donor button is trephination aiming for 0.25-0.5 mm larger than the host trephination. A trephine is placed on the host’s cornea, and a button three-quarters through the stroma is excised, and a peripheral iridotomy/iridectomy is performed. The donor button is secured to the host corneal tissue using non-absorbable sutures, which are rotated to bury the knots. Viscoelastic hyaluronic acid may be used, if needed, to prevent the iris from sticking to the suture line. Antibiotic therapy is applied as per local protocols, and the eye is shielded.
Descemet’s Membrane Endothelial Keratoplasty
Following the establishment of anesthesia, an eyelid speculum is inserted, and the patient’s eye is secured using a scleral fixation ring or sutures. Two to four paracentesis sites and a temporal corneal incision are created, and the anterior chamber is filled with viscoelastic hyaluronic acid. A peripheral iridotomy is created to prevent pupillary block. The donor’s corneal epithelium with a circular ring to create a resection template and the DM is scored peripherally, peeled from the overlying stroma and removed. The donor button is stained with trypan blue solution to ensure visibility and inserted into the anterior chamber. An air or sulfur hexafluoride bubble is injected to ensure adhesion. Closure of the primary incision is with a buried non-absorbable suture. Antibiotic therapy is applied as per local protocols, and the eye is shielded.
Complications
Possible complications are divisible into early and late. Early complications, occurring within days to weeks post-operatively, include wound leakage, raised intra-ocular pressure, bleeding and infection. Late complications, occurring months to years postoperatively, include graft rejection, corneal swelling, cataracts, astigmatism and recurrence of the original disease. Reported 5-year and 15-year graft survival rates are approximately 70% and 50%, respectively.[23][24]
Clinical Significance
The first successful corneal transplant was more than 110 years ago. At the moment corneal transplants worldwide are one of the most common transplants performed. The US has the highest rates of corneal transplants worldwide, with an exponential increase of EK transplantations over PK, the former representing approximately 60% of all transplants.[25] The proportion of EK over PK is considerably lower outside the US with a third of all countries worldwide reporting no EKs completed.[25]
Selective keratoplasty techniques have revolutionized the corneal transplantation field with improvements in graft survival, refractive and visual outcomes.[26] With the advent of new techniques, the threshold for surgical intervention has lowered, increasing the demand for human cadaveric corneas, with only a 30 to 40% gap needed.
Corneal endothelial cells (CECs) cannot at present be expanded in laboratory conditions following biopsy. Recent work has focused on using alternative stem cells, such as mesenchymal stem cells,[27] or induced pluripotent stem cells that differentiate towards a neural crest and endothelial lineage following ROCK inhibition.[28] CEC generated in vitro have shown promise in large animal models.[29] This approach following optimization may represent a therapeutic option for endothelial replacement secondary to CEC dysfunction, such as in Fuchs’ endothelial corneal dystrophy.
Enhancing Healthcare Team Outcomes
an interprofessional approach that includes an ophthalmologist, nurse practitioner, and the primary care provider is required to ensure the best visual and health outcomes in an aging population with increasingly complex medical backgrounds. Clear communication with the patient or their caregivers is necessary for early identification of any complications and for time management.
Worldwide trends in corneal transplantation suggest a slow uptake of new procedures by ophthalmologists,[25] indicating the need for further training in a specialized center, locally or abroad. Appropriate incentives might enhance and fasten the adaptation of newer techniques.