Anatomy, Bony Pelvis and Lower Limb, Calf Deep Peroneal (Fibular) Nerve
- Article Author:
- Alexandrea Garrett
- Article Editor:
- Zachary Geiger
- Updated:
- 8/10/2020 5:46:41 PM
- For CME on this topic:
- Anatomy, Bony Pelvis and Lower Limb, Calf Deep Peroneal (Fibular) Nerve CME
- PubMed Link:
- Anatomy, Bony Pelvis and Lower Limb, Calf Deep Peroneal (Fibular) Nerve
Introduction
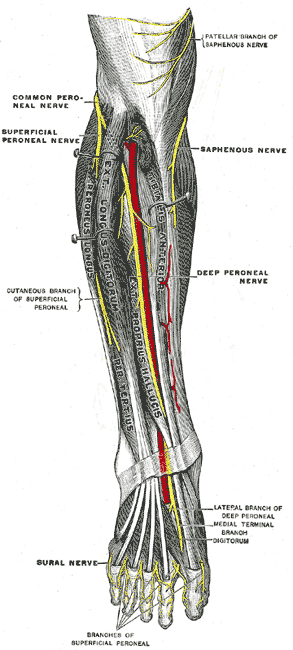
The deep peroneal nerve is also known as the deep fibular nerve. It originates after the bifurcation of the common peroneal nerve between the upper segment of the peroneus longus and the head of the fibula.[1] The common peroneal nerve (spinal nerves L4 through S1) itself originates from the bifurcation of the sciatic nerve (spinal nerves L4 through S3) which terminates at the apex of the popliteal fossa into the common peroneal and the tibial nerve after wrapping around the neck of the fibula.[2],[3] After bifurcation from the common peroneal nerve, the deep peroneal nerve then traverses deep to the extensor digitorum longus and runs on the anterior surface of the interosseous membrane.[1] In the middle of the leg, it is in close association with the anterior tibial artery and then descends with the artery to lie in front of the ankle joint. Here, it gives off the lateral and medial terminal branches. The medial terminal branch accompanies the dorsalis pedis and runs on the dorsum of the foot reaching the first interosseous space where it divides into digital nerves that supply the side of the great and second toes. The lateral terminal branch runs beneath the extensor digitorum brevis and gives off interosseous branches that supply the tarsal and metatarsophalangeal joints.[1]
Structure and Function
The deep peroneal nerve has both motor and sensory components. The motor component is responsible for innervating the anterior compartment of the lower leg which includes the tibialis anterior, extensor hallucis longus, extensor digitorum longus, and peroneus tertius muscles.[1] Activation of these muscles by the deep peroneal nerve is primarily responsible for dorsiflexion of the foot, the extension of the toes, and assists the dominating tibialis anterior with inversion of the foot.[2] There is also a lateral terminal branch of the nerve that terminates into the dorsal interosseous nerves that provide motor innervation to the extensor digitorum brevis and extensor hallucis brevis muscles which assist in extending all toes except the smallest toe.[1]
The deep peroneal nerve has 2 sensory components that innervate small portions of the dorsal foot. An articular branch of the lateral terminal branch is responsible for providing sensory information to the ankle joint and the sinus tarsi. The medial terminal branch of the deep peroneal nerve provides sensory information to the web space between the first and second toes.[1]
Blood Supply and Lymphatics
The deep peroneal nerve travels in an inferomedial direction in the anterior compartment of the leg to run along with and be supplied by the anterior tibial artery.[2] Unlike the sciatic or tibial nerves, which are supplied by numerous arterial branches of different origins, the deep peroneal nerve has little variation in its blood supply.[4] The susceptibility of the nerve to injury and lack of response to operative treatment may be explained by the fact that the nerve is most often only supplied by one blood vessel in contrast to the sciatic and tibial nerves.[5]
Muscles
The deep peroneal nerve supplies the following muscles:
- Tibialis anterior
- Extensor digitorum longus
- Peroneus tertius
- Extensor hallucis longus (propius)
- Extensor digitorum brevis
- Extensor hallucis brevis
Physiologic Variants
The accessory deep peroneal nerve may supply motor innervation to the extensor digitorum brevis and some sensory innervation to the lateral ankle and foot. However, this nerve is derived from the superficial peroneal nerve or its branches rather than the deep peroneal nerve which normally supplies the extensor digitorum brevis exclusively. The accessory deep peroneal nerve may develop in as many as 28% of patients, and it has been suggested that this anomaly may be inherited in an autosomal dominant fashion. [6]
Surgical Considerations
If divided into four zones, the tibia has been used to identify deep peroneal nerve injury risk during ankle external fixator placement. Zone 1 includes where the nerve courses around the fibular neck and lies on the interosseous membrane at the proximal portion of the tibia. Zone 2 includes where the nerve still lies on the interosseous membrane but remains at the posterior edge of the lateral tibia. Zone 3 includes where the nerve moves away from the membrane and lies directly in contact with the tibia. Finally, zone 4 includes where the nerve lies on the anterior portion of the distal tibia. Deep peroneal nerve injury was found to be most at risk for injury in zones 2 and 3 when placing an external fixator. [7]
Clinical Significance
Direct injury to the deep peroneal nerve (during surgery) or lateral injury to the knee can result in a foot drop in which the patient is unable to dorsiflex their foot and/or the patient may have some weakness on inversion of the foot. The deep peroneal nerve may also be affected in people with diabetes, lower motor neuron disease, infectious disorders, and ischemia. Injury to the deep peroneal nerve is a common cause of mononeuropathy of the lower leg. In people who perform repetitive motions, the deep peroneal nerve can become entrapped at the ankle beneath the extensor retinaculum which is referred to as anterior tarsal tunnel syndrome.[8] Here, the nerve is compressed by the extensor hallucis longus tendon, osteophytes, bony prominences, or exostosis. Occasionally, ganglia may also be the cause of nerve compression.[9]
Women who wear high-heeled shoes or individuals who sit for a prolonged period with the feet plantar flexed can also develop neuropathy of this nerve. Other causes of deep peroneal nerve entrapment include space-occupying lesions, surgery on the lateral knee, and chronic compartment syndrome. Ganglion cysts may also cause peripheral neuropathies in the common peroneal nerve and its branches which typically occur at the level of the fibular neck. [10]
Patients with deep peroneal nerve neuropathy may present with vague pain, a burning sensation, or a cramp over the dorsum of the foot that may or may not involve the web-space between the first and second toes. Other individuals may present with nocturnal foot pain. Symptoms may worsen with a certain type of shoe or a particular activity. When there is more proximal involvement, it may present with tripping or foot drop due to a weakness of the extensor hallucis longus muscle.