Deep Vein Thrombosis
- Article Author:
- Sheikh Waheed
- Article Author:
- Pujitha Kudaravalli
- Article Editor:
- David Hotwagner
- Updated:
- 8/10/2020 9:05:41 PM
- For CME on this topic:
- Deep Vein Thrombosis CME
- PubMed Link:
- Deep Vein Thrombosis
Introduction
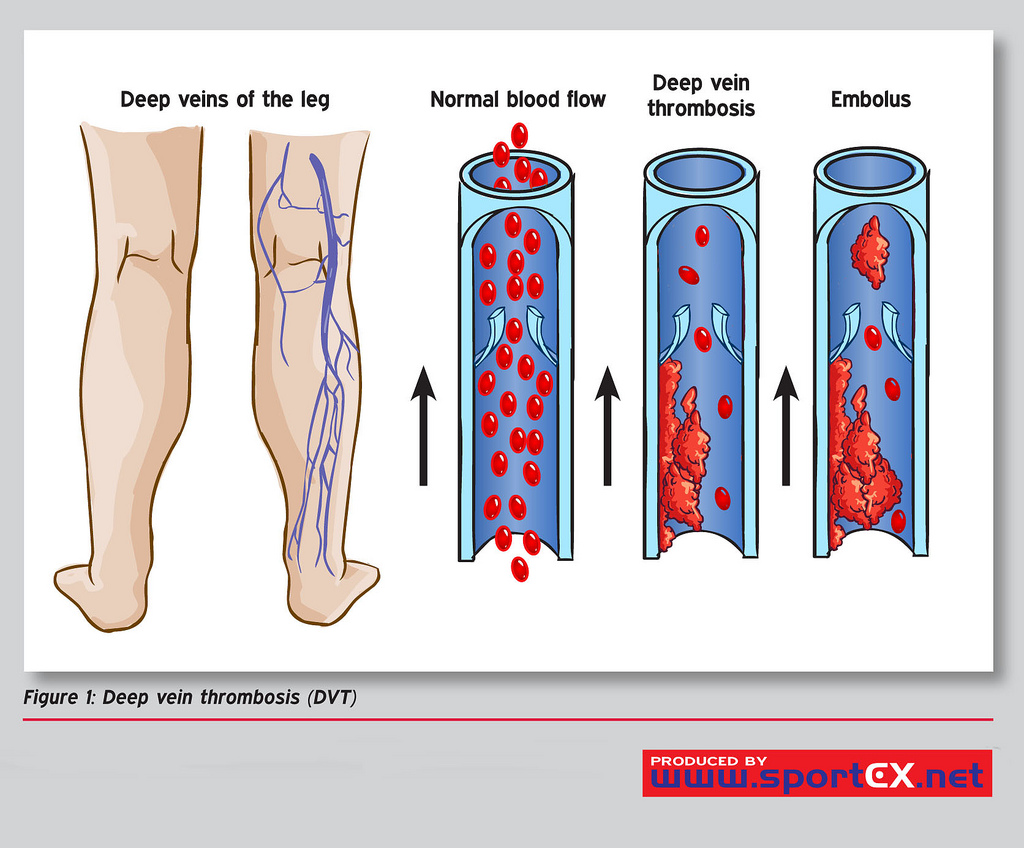
A deep-vein thrombosis (DVT) is a blood clot that forms within the deep veins, usually of the leg, but can occur in the veins of the arms and the mesenteric and cerebral veins. Deep-vein thrombosis is a common and important disease. It is part of the venous thromboembolism disorders which represent the third most common cause of death from cardiovascular disease after heart attacks and stroke. Even in patients who do not get pulmonary emboli, recurrent thrombosis and "post-thrombotic syndrome" are a major cause of morbidity.[1][2][3]
DVT is a major medical problem accounting for most cases of pulmonary embolism. Only through early diagnosis and treatment can the morbidity be reduced.
Etiology
Risk Factors
Following are the risk factors and are considered as causes of deep venous thrombosis:
- Reduced blood flow: Immobility (bed rest, general anesthesia, operations, stroke, long flights)
- Increased venous pressure: Mechanical compression or functional impairment leading to reduced flow in the veins (neoplasm, pregnancy, stenosis, or congenital anomaly which increases outflow resistance)
- Mechanical injury to the vein: Trauma, surgery, peripherally inserted venous catheters, previous DVT, intravenous drug abuse.
- Increased blood viscosity: Polycythaemia rubra vera, thrombocytosis, dehydration
- Anatomic variations in venous anatomy can contribute to thrombosis.
Increased Risk of Coagulation
- Genetic deficiencies: Anticoagulation proteins C and S, antithrombin III deficiency, factor V Leiden mutation
- Acquired: Cancer, sepsis, myocardial infarction, heart failure, vasculitis, systemic lupus erythematosus and lupus anticoagulant, Inflammatory bowel disease, nephrotic syndrome, burns, oral estrogens, smoking, hypertension, diabetes
Constitutional Factors
Obesity, pregnancy, Increasing age, surgery, and cancer. [4][5][6]
Epidemiology
Incidence and prevalence: Deep-vein thrombosis and pulmonary emboli are common and often "silent" and thus go undiagnosed or are only picked up at autopsy. Therefore, the incidence and prevalence are often underestimated. It is thought the annual incidence of DVT is 80 cases per 100,000, with a prevalence of lower limb DVT of 1 case per 1000 population. Annually in the United States, more than 200,000 people develop venous thrombosis; of those, 50,000 cases are complicated by pulmonary embolism.[7][8][9]
Age: Deep-vein thrombosis is rare in children, and the risk increases with age, most occurring in the over 40s.
Gender: There is no consensus about whether there is a sex bias in the incidence of DVT.
Ethnicity: There is evidence from the United States that there is an increased incidence of DVT and an increased risk of complications in African Americans and white people when compared to Hispanics and Asians.
Associated diseases: In the hospital, the most commonly associated conditions are malignancy, congestive heart failure, obstructive airway disease, and patients undergoing surgery.
Pathophysiology
According to Virchow's triad, the following are the main pathophysiological mechanisms involved in DVT:
- Damage to the vessel wall
- Blood flow turbulence
- Hypercoagulability
Thrombosis is a protective mechanism that prevents the loss of blood and seals off damaged blood vessels. Fibrinolysis counteracts or stabilizes the thrombosis. The triggers of venous thrombosis are frequently multifactorial, with the different parts of the triad of Virchow contributing in varying degrees in each patient, but all result in early thrombus interaction with the endothelium. This then stimulates local cytokine production and causes leukocyte adhesion to the endothelium, both of which promote venous thrombosis. Depending on the relative balance between the coagulation and thrombolytic pathways, thrombus propagation occurs. DVT is commonest in the lower limb below the knee and starts at low-flow sites, such as the soleal sinuses, behind venous valve pockets. [10][11][12]
History and Physical
History
- Pain (50% of patients)
- Redness
- Swelling (70% of patients)
Physical Examination
- Limb edema may be unilateral or bilateral if the thrombus is extending to pelvic veins
- Red and hot skin, with dilated veins
- Tenderness
Evaluation
As per the NICE guidelines following investigations are done:
- D-dimers (very sensitive but not very specific)
- Coagulation profile
- Proximal leg vein ultrasound, which when positive, indicates that the patient should be treated as having a DVT
Deciding how to investigate is determined by the risk of DVT. The first step is to assess the clinical probability of a DVT using the Wells scoring system.
- For patients with a score of 0 to 1, the clinical probability is low, but for those with 2 or above, the clinical probability is high.
- If a patient scores 2 or above, either a proximal leg vein ultrasound scan should be done within 4 hours, and if the result is negative, a D-dimer test should be done. If imaging is not possible within 4 hours, a D-dimer test should be undertaken, and an interim 24-hour dose of a parenteral anticoagulant should be given. A proximal leg vein ultrasound scan should be carried out within 24 hours of being requested.
- In the case of a positive D-dimer test and a negative proximal leg vein ultrasound scan, the proximal leg vein ultrasound scan should be repeated 6 to 8 days later for all patients.
- If the patient does not score 2 on the DVT Wells score, but the D-dimer test is positive, the patient should have a proximal leg vein ultrasound scan within 4 hours, or if this is not possible, the patient should receive an interim 24-hour dose of a parenteral anticoagulant. A proximal leg vein ultrasound scan should then be carried out within 24 hours of being requested.
- In all patients diagnosed with DVT, treat as if there is a positive, proximal leg vein ultrasound scan.[13][14][15]
Treatment / Management
Treatment of DVT aims to prevent pulmonary embolism, reduce morbidity, and prevent or minimize the risk of developing post-thrombotic syndrome.
The cornerstone of treatment is anticoagulation. NICE guidelines only recommend treating proximal DVT (not distal) and those with pulmonary emboli. In each patient, the risks of anticoagulation need to be weighed against the benefits.[16][17][18]
- Anticoagulation
- Low-molecular-weight heparin or fondaparinux for five days or until INR is greater than 2 for 24 hours (unfractionated heparin for patients with renal failure and increased risk of bleeding)
- Vitamin K analogs for three months
- In patients with cancer, consider anticoagulation for six months with low-molecular-weight heparin
- In patients with unprovoked DVT consider vitamin K analogs beyond three months
- Rivaroxaban is an oral factor Xa inhibitor which has recently been approved by the FDA and NICE and is attractive because there is no need for regular INR monitoring
- If platelet count drops to less than 75,000, switch from heparin to fondaparinux, which is not associated with heparin-induced thrombocytopenia.
- Thrombolysis: The indications for the use of thrombolytics include:
- Symptomatic iliofemoral DVT
- Symptoms of less than 14 days duration
- Good functional status
- A life expectancy of 1 year or more
- Low risk of bleeding
The use of thrombolytic therapy can result in an intracranial bleed, and hence, careful patient selection is vital. Recently endovascular interventions like catheter-directed extraction, stenting, or mechanical thrombectomy have been tried with moderate success.
- Compression hosiery: Below-knee graduated compression stockings with an ankle pressure greater than 23 mm Hg for two years if there are no contraindications
- Inferior vena cava filters: If anticoagulation is contraindicated or if emboli are occurring despite adequate anticoagulation
Newer drugs
Rivaroxaban, apixaban, dabigatran, edoxaban, betrixaban are relatively newer factor Xa inhibitors approved for prophylaxis of deep vein thrombosis.
The duration of treatment for DVT is for 3-6 months, but recurrent episodes may require at least 12 months of treatment. Patients with cancer need long term treatment.
Inferior vena cava filters are not recommended in acute DVT. There are both permanent and temporary inferior vena cava filters available. These devices may decrease the rate of recurrent DVT but do not affect survival. Today, only patients with contraindications to anticoagulation with an increased risk of bleeding should have these filters inserted.
Differential Diagnosis
Following are differential diagnoses of deep venous thrombosis:
- Cellulitis
- Post-thrombotic syndrome (especially venous eczema and lipodermatosclerosis)
- Ruptured Baker cyst
- Trauma
- Superficial thrombophlebitis
- Peripheral edema, heart failure, cirrhosis, nephrotic syndrome
- Venous or lymphatic obstruction
- Arteriovenous fistula and congenital vascular abnormalities
- Vasculitis
Staging
The severity of the disease is classified as:
- Provoked: Due to acquired states (surgery, oral contraceptives, trauma, immobility, obesity, cancer)
- Unprovoked: Due to idiopathic or endogenous reasons; more likely to suffer recurrence if anticoagulation is discontinued
- Proximal: Above the knee; affecting the femoral or iliofemoral veins; much more likely to lead to complications such as pulmonary emboli
- Distal: Below the knee
Prognosis
- Many DVTs will resolve with no complications.
- Post-thrombotic syndrome occurs in 43% two years post-DVT (30% mild, 10% moderate, and severe in 3%).
- The risk of recurrence of DVT is high (up to 25%).
- Death occurs in approximately 6% of DVT cases and 12% of pulmonary embolism cases within one month of diagnosis.
- Early mortality after venous thromboembolism is strongly associated with the presentation as pulmonary embolism, advanced age, cancer, and underlying cardiovascular disease.
Complications
The following are the two major complications of DVT;
- Pulmonary emboli (paradoxical emboli if an atrioseptal defect is present)
- Post-thrombotic syndrome
- Bleeding from the use of anticoagulants
Deterrence and Patient Education
- Ambulation
- Wear compression stockings
- Discontinue smoking
Enhancing Healthcare Team Outcomes
DVTs occur in many hospitalized patients, and one of the most feared complications is a pulmonary embolus. DVTs occur in many settings, and almost every medical specialty; failing to diagnose DVT can result in a pulmonary embolus, which can be fatal. DVTs also result in longer admission to the hospital and drug treatment that can last 3-9 months- all of which adds to the cost of healthcare. Thus its diagnosis and management are best done with an interprofessional team.
The focus is on the prevention of DVT. Besides physicians, both nurses and pharmacists are vital in educating patients about DVT prophylaxis. Nurses are the first professionals to encounter patients being admitted to the hospital, and it is here that the prevention of DVT starts. Nurses need to educate the patients on the importance of ambulation, being compliant with compression stockings, and taking the prescribed anticoagulation medications. In both the operating room and post-surgery, nurses play a key role in reminding physicians for the need for DVT prophylaxis. Each hospital has guidelines on DVT prophylaxis and treatment, and all healthcare workers should follow them. Once a DVT has developed, the pharmacist should be familiar with the current anticoagulants and their indications. Plus, the pharmacist must educate the patients on the need for treatment compliance and the need to undergo regular testing to ensure that the INR is therapeutic. [17][19](Level 5)
Once DVT is diagnosed, the treatment is with an anticoagulant for 3-6 months, and again, monitoring of the INR by a hematology nurse or pharmacist is necessary. Further, these patients need to be monitored for bleeding. Open communication between the interprofessional team is the only way to treat DVT and lower the morbidity of the drugs safely.
Outcomes
Close to 300,000 patients die from a pulmonary embolus each year in the US alone. Despite countless guidelines and education of healthcare workers, DVT prophylaxis is often not done. The fact is that DVT is preventable in the majority of patients, and the onus is on healthcare workers to be aware of the condition. For those who do develop a DVT and survive, post-thrombotic phlebitis is a lifelong sequela, which has no ideal treatment. [20][21] (Level 5)