Empty Sella
- Article Author:
- Peter Ucciferro
- Article Editor:
- Catherine Anastasopoulou
- Updated:
- 8/10/2020 4:42:18 PM
- For CME on this topic:
- Empty Sella CME
- PubMed Link:
- Empty Sella
Introduction
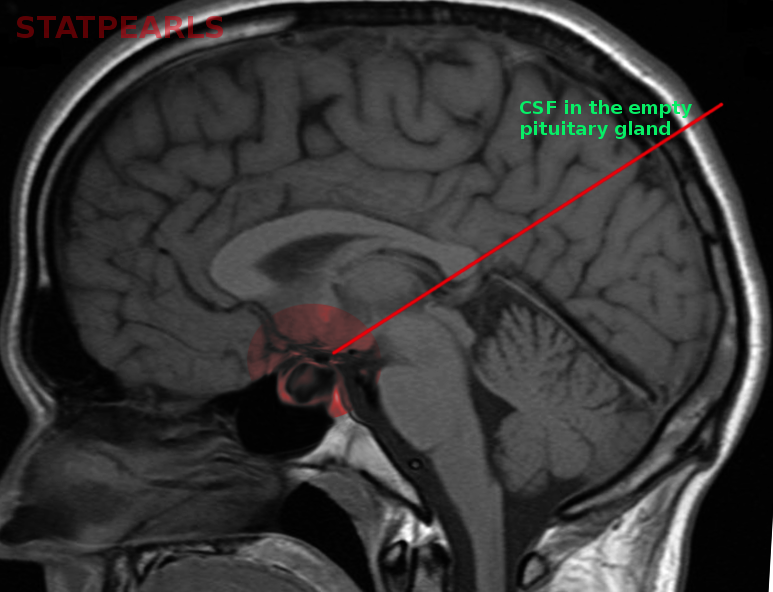
Empty sella syndrome (ESS), also known as arachnoidocele, is a disorder in which the subarachnoid space herniates into the sella turcica causing compression and flattening of the pituitary gland and stretching of the pituitary stalk. There is still some debate as to who first coined the term “empty sella”; W. Bush vs. Sheehan and Summer. Both used this term around the 1950s to describe a phenomenon recognized in cadavers in which there was an empty appearance of the sella turcica and flattened pituitary gland. Over the following years, the term was adapted further by radiologists observing a similar phenomenon in computed tomograms (CTs) and magnetic resonance imaging scans (MRIs) of the brain.
Etiology
Regarding pathophysiology and etiology, empty sella syndrome (ESS) subdivides into two categories: primary empty sella syndrome (PES) and secondary empty sella syndrome (SES). Although this will use this distinction, it is worth noting that both primary and secondary empty sella can be thought of and treated as one entity: ESS.
PES is a disorder caused by the incompetence of the diaphragma sellae and resultant herniation of CSF into the sella turcica. There is no clear genetic association known to predispose someone to develop PES, but the incompetent diaphragma sellae is likely to present at birth. SES results from surgery, radiation, hemorrhage, or infarction of the pituitary gland and it can happen at any time in a person's life.
Epidemiology
Empty sella syndrome is considered to be a rare entity, but research reports its incidence as present in 5.5 to 12% of autopsy cases, and it is also estimated to be present in around 12% of patients undergoing neuroimaging.[1] Some reports note an even higher incidence in clinical practice with estimates of up to 35%.[1] It demonstrates a female predilection with a ratio of 4 or 5 to 1 over males, and it is more common in obese patients. The incidence of ESS peaks in the fourth to the sixth decade.[1][2] Although more common in women, the pituitary hormonal dysfunction appears to occur at higher rates in men with empty sella.
Pathophysiology
As stated above, empty sella syndrome falls into two categories: primary empty sella syndrome and secondary empty sella syndrome.
PES is the less common of the two entities. Currently, its cause is not entirely understood, but researchers have proposed several mechanisms including incompetence or complete absence of the diaphragma sellae, chronic intracranial hypertension, and temporary expansion followed by regression of the pituitary gland.
Incompetent diaphragma sellae has been the finding in the vast majority of PES at autopsy reports. The anomalous diaphragma sellae allows the accumulation of cerebrospinal fluid (CSF) into the sella turcica causing remodeling and enlargement of the sella turcica as well as flattening of the pituitary gland.
Intracranial hypertension is also thought to increase the likelihood of herniation of CSF into the sella turcica especially if the diaphragma sellae is already compromised. The most common neuroimaging finding in patients with idiopathic intracranial hypertension (also known as pseudotumor cerebri) is empty sella.[3] Many different pathologies causing increased CSF pressures have correlations with PES including brain tumors, idiopathic intracranial hypertension (pseudotumor cerebri), intracranial thrombosis, and hydrocephalus. The resolution of empty sella on imaging after treatment of intracranial hypertension illustrated further evidence that intracranial hypertension can cause empty sella.[4]
The last proposed mechanism causing empty sella involves an initial enlargement of the pituitary gland followed by a later decrease in gland size which creates an empty space in which CSF can accumulate. Examples of this include a normal increase in pituitary volume during pregnancy and lactation and then spontaneous regression in pituitary volume during menopause in women.
SES, on the other hand, is much more common than PES. It could be the result of the treatment of a pituitary adenoma (by either drugs, surgery, or radiotherapy), spontaneous regression of the pituitary gland under different circumstances, postpartum pituitary necrosis (also known as Sheehan syndrome) or lymphocytic hypophysitis.[2]
History and Physical
History and physical exam are typically normal in patients with empty sella syndrome because the endocrine function is usually intact. The most common symptom associated with ESS is a headache. There is lack of evidence to support ESS as the cause of the headache and many experts believe that the association exists because the headache of any unrelated cause prompted imaging of the head to be done leading to the incidental discovery of the empty sella. Other authors consider the possibility that increased intracranial pressure and possible herniation is the cause of the headaches; however, no confirmation of this theory exists either.
Spontaneous cerebrospinal fluid rhinorrhea is possible as is visual field impairment; however, both of these presentations are rare.[5]
Endocrine abnormalities are present in less than 20% of cases of the empty sella. If the pituitary function is compromised, history and physical exam can be consistent with any, or all, of the pituitary hormone deficiencies.
Evaluation
Testing of the entire pituitary axis is appropriate and highly recommended in patients with empty sella syndrome after diagnosis; however, there is currently a lack of society based guidelines.[6][7][8] In most cases, the pituitary function is normal (despite the abnormal appearance of the pituitary gland), but in some cases (around 20%) any, or all, of the pituitary hormone levels can be affected. Hyperprolactinemia and growth hormone deficiency appear to be the two most common findings in empty sella.[2][9] Hyperprolactinemia is present in 10 to 17% of cases and may result from a microprolactinoma or functional hyperprolactinemia.[1][9] Growth hormone deficiency presents in 4 to 60% of cases, but its clinical significance in adults is unclear.[1][6] Gonadotropin deficiency is seen in 2 to 32% of cases while adrenocorticotropin, thyroid-stimulating hormone, and antidiuretic hormone deficiencies are seen less frequently, around 1% each.[6]
The following labs are necessary for the evaluation of pituitary function in any patient found to have empty sella:
-
Adrenal axis: An early morning, fasting cortisol levels are a screening option for adrenocorticotropin (ACTH) deficiency and overtly low levels of cortisol less than 3.0 mcg/dL are consistent with adrenal insufficiency. Morning cortisol levels greater than 11.0 (some authors suggest 14.0) mcg/dL make adrenal insufficiency very unlikely, while morning cortisol levels of 3.1 to 11.0 (14.0) mcg/dL are indeterminant and can warrant further testing such as cosyntropin (ACTH) stimulation testing. If morning cortisol level is low, an ACTH level should be obtained and correlated to the low am cortisol level to help differentiate primary from secondary/central adrenal insufficiency. Metyrapone testing can also assist in this diagnosis. If corticosteroid excess is suspected, an ACTH level again needs to be correlated with cortisol level, and a workup for Cushing disease should be the next step.
-
Thyroid axis: thyroid-stimulating hormone (TSH) level with free thyroxine (T4) level at the same time should be checked.
-
Reproductive axis: In premenopausal women with regular menses, gonadotropin, and estradiol levels are not necessary. If menses are irregular or absent, then follicle-stimulating hormone (FSH) and luteinizing hormone (LH) with estradiol levels should be checked. Postmenopausal women most likely do not need FSH, LH, or estradiol levels checked. In men, a testosterone level with simultaneous LH and FSH levels should be obtained.
-
Prolactin (PRL): PRL levels should be obtained. Hyperprolactinemia is much more common than PRL deficiency. PRL elevations can be seen in many conditions not related to ESS (ex. drugs, pregnancy, etc.) and thus abnormalities must be correlated with the clinical presentation.
-
Growth Hormone (GH), excess or deficiency: GH has a short half-life and is pulsatile throughout the day, so measuring serum levels is not a common practice. Insulin-like growth factor 1 (IGF-1) can be used instead as a screening measure. However, normal levels of IGF-1 do not rule out GH deficiency. Stimulation testing is recommended by some experts to rule out the possibility of GH deficiency.[6] The gold standard testing for GH deficiency is the insulin tolerance test. Other options are GHRH plus arginine test, glucagon stimulation, or macimorelin test.
-
Antidiuretic hormone (ADH): ADH levels are not typically measured, but the clinicians should inquire about the frequency of urination, including nocturia, to rule out the possibility of diabetes insipidus. If suspicious of diabetes insipidus, serum sodium, serum osmolality, and urine osmolality should be obtained.
-
Oxytocin levels are not a routine lab for screening in ESS.
Treatment / Management
In most instances, no treatment is necessary for empty sella syndrome. If there is hormone deficiency or excess, treatment is individualized towards the hormone derangements present.
Differential Diagnosis
Empty sella is a radiologic finding and diagnosis. Differentials relating to this entity stem from each specific cause (ex. intracranial hypertension would have many differentials). Please see the pathophysiology section for further details.
Prognosis
The presence of empty sella syndrome does not change life expectancy, and it is usually a benign condition. In cases where a specific hormone deficiency or excess is present, that specific hormone abnormality and its treatment determine the prognosis.
Complications
Possible complications of empty sella include the development of partial, or complete, hypopituitarism, or hormone hyperfunctioning as noted above. Additionally, there is an association of worse outcomes for patients undergoing pituitary surgery with known primary empty sella (ex. Cushing's disease).[10]
Deterrence and Patient Education
There is nothing in particular that patients can do to avoid this phenomenon, but they should be aware of the need for evaluation of hormone levels at diagnosis. If initial hormone levels are all within normal limits, no additional testing is required.
Enhancing Healthcare Team Outcomes
Empty sella syndrome is a rare entity that is usually found incidentally during evaluation of headache or other complaints leading to imaging of the brain/head. Although only a small fraction of these patients have associated hormone deficiencies, a full pituitary hormone workup is the indicated screening approach at diagnosis, and the patients should receive an endocrinologist referral. The optimal management approach an interprofessional team of specialty-trained nurses and clinicians providing regular follow up, education of the patient and family, coordination of care, and laboratory evaluation. [Level 5]