Endometrial Biopsy
- Article Author:
- Adam Will
- Article Editor:
- Kristian Sanchack
- Updated:
- 10/30/2020 8:45:03 AM
- For CME on this topic:
- Endometrial Biopsy CME
- PubMed Link:
- Endometrial Biopsy
Introduction
Endometrial biopsy is frequently used to evaluate abnormal uterine bleeding. It is a relatively quick and cost-effective way to sample the endometrium to allow for direct histological evaluation of the endometrium. It is essential to have as endometrial cancer is the fourth most common cancer among women. The American Cancer Society estimates that there will be 61880 new uterine cancer cases and 12,160 related deaths in 2019.[1] The patient does not need to undergo more invasive procedures as endometrial biopsies have a high sensitivity and specificity for detecting endometrial hyperplasia and endometrial malignancy that is equal to the diagnostic accuracy dilatation and curettage (D&C) procedure.[2]
Anatomy and Physiology
Uterus corpus: the body of the uterus that is located in a female’s lower abdomen, between the bladder and the rectum.
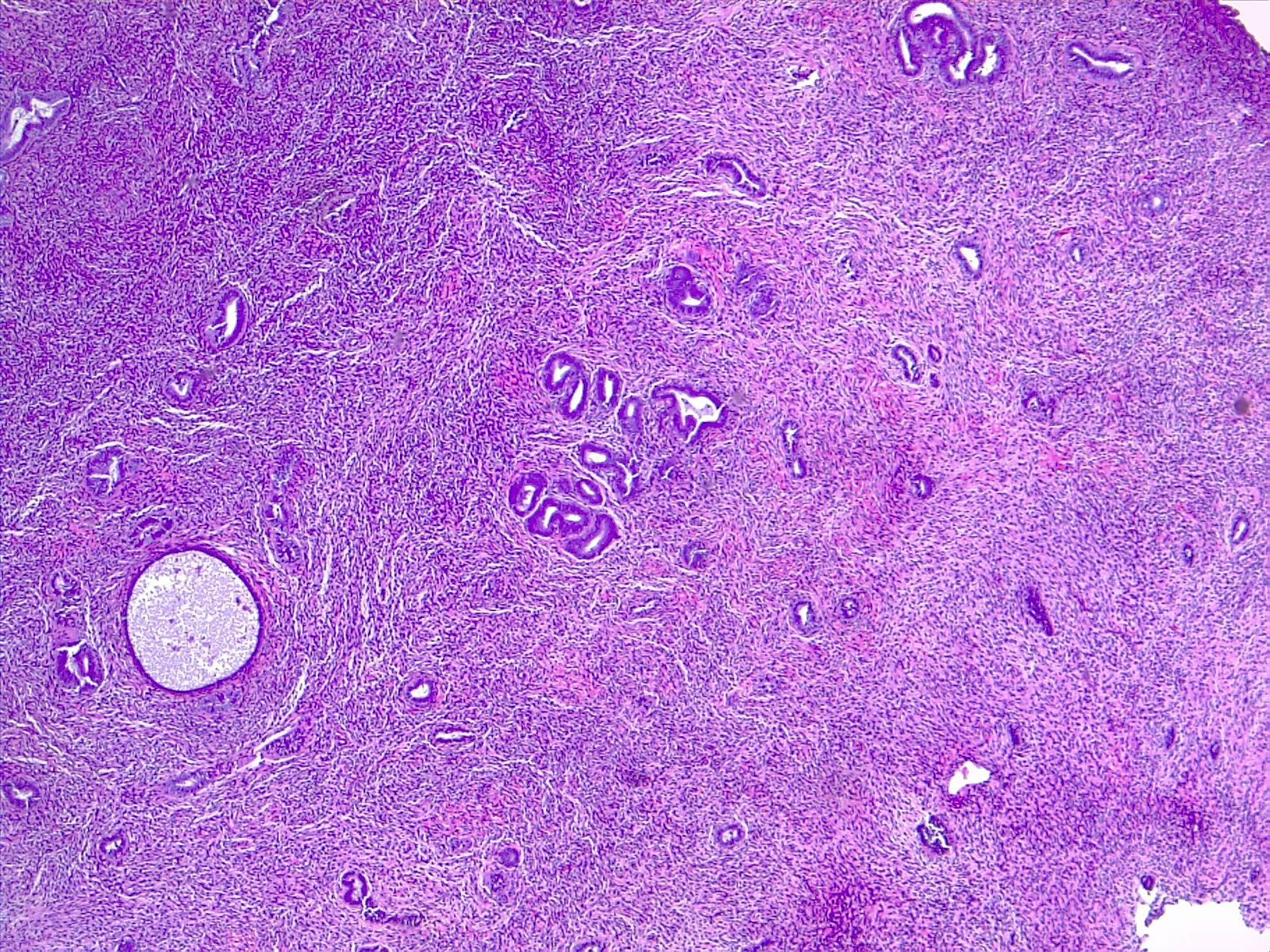
Endometrium: the lining of the uterine cavity. It is a layer of glandular epithelium and stroma that changes thickness during the cycle.
Cervix: the cervix is the most inferior part of the uterus. The cervical canal connects the uterus to the vagina.
Vagina: a passageway that connects the cervix and the vulva (the external genitalia).
Indications
- Abnormal uterine bleeding
- Evaluation for endometrial neoplasia or precancerous hyperplasia
- Surveillance of previously diagnosed endometrial hyperplasia or cancer
- Evaluation of uterine response to hormone therapy
Contraindications
Absolute Contraindications
- Pregnancy
- Acute pelvic inflammatory disease
- Acute cervical infection
- Acute vaginal infection
- Cervical cancer
Relative Contraindications
- Morbid obesity
- Cervical stenosis
- Clotting disorder or coagulopathy
Equipment
- Patient labels
- Biopsy container with formalin
- Speculum
- Lubricating gel
- Sterile and non-sterile gloves
- Uterine sound
- Cervical dilators
- Single-toothed tenaculum
- Ring Forceps
- Iodine swabs
- Topical benzocaine gel (20%) or benzocaine spray
- Endometrial suction catheter (pipelle) x2
- 4x4 gauze
- Silver nitrate
Personnel
A clinician in the outpatient setting can perform this procedure independently. However, it may be prudent to have an assistant to help in preparation and specimen handling.
Preparation
Minimal preparation is required for this procedure. The procedure should be discussed with the patient in detail to include the procedure's risks and benefits. Informed consent must be obtained before starting the procedure.
Any women of reproductive age or with the potential for pregnancy should have a documented negative pregnancy test prior to the procedure.
The patient can take an NSAID 30 to 60 minutes before the procedure to reduce the pain associated with cramping.
Prophylactic antibiotics are not necessary during endometrial sampling for the prevention of surgical site infection or bacterial endocarditis.[3]
Technique
The first part of the procedure is non-sterile. The patient is first placed in the lithotomy position, and a bimanual examination is done to determine the uterine size and position of the uterus. The speculum can now be inserted to allow for cervical visualization. Of note, if a Pap smear is necessary, this is an ideal time to obtain the appropriate samples before continuing the procedure. Once visualized, the cervix can be anesthetized and cleansed by spraying a 20 percent benzocaine spray for 5 seconds then applying an iodine solution. At this time, it is appropriate to wash hands and don sterile gloves.
The next step is to determine the depth of the uterus, which is done with a uterine sound. The first step is to stabilize the cervix. A tenaculum is placed on the anterior lip of the cervix and allows the provider to straighten the uterocervical angle. The uterine sound is then inserted to an average depth of 6 to 10 cm within the uterus. The provider can discern that the sound is fully inserted when feeling resistance from the fundus. One common complication at this step is that the uterine sound will not pass through the internal cervical os; this can be overcome by using cervical dilators. The smallest size is inserted, followed by successively larger dilators' insertion until the sound can reach the fundus.
Once achieving adequate os dilation and determining the uterus' depth, the sampling pipelle can be inserted. The pipelle should be advanced until encountering resistance. This resistance should be at the same depth as the sounding of the uterus. Once the pipelle is in the uterine cavity, the internal piston on the catheter is fully withdrawn, creating suction at the catheter tip. This suction, accompanied by moving the tip with an in and out motion, allows for sample collection. This motion should be completed with a 360-degree twisting motion to reach all four quadrants of the endometrium. The pipelle is now removed, and the collected tissue sample is placed into a formalin solution. A second pass into the uterus can be done to ensure the collection of adequate tissue. If a second pass is made, ensure the catheter is not contaminated when being emptied of the first specimen.
Gently remove the tenaculum to complete the procedure. Most bleeding will be controllable with pressure via cotton swabs or a sponge stick. If bleeding persists, use silver nitrate sticks to cauterize the site.
Complications
The most common side effect of an endometrial biopsy is cramping. This can be significantly reduced with the administration of pre-procedure NSAIDs. Once the procedure is completed, women may report light vaginal bleeding or spotting for several days. Less common side effects include uterine perforation, pelvic infection, and bacteremia. They are monitored for by instructing the patient with strict return precautions to include returning to the office for fever, cramping continuing for more than 48 hours, increasing pain, bleeding heavier than a normal menstrual period, or any foul-smelling discharge.
Clinical Significance
Endometrial biopsy is a safe and well-accepted method to evaluate abnormal or postmenopausal bleeding. As postmenopausal bleeding must always be investigated, this procedure becomes a valuable office-based diagnostic tool.[4] The Society of Radiologists in Ultrasound released a consensus opinion that states either endometrial biopsy or transvaginal ultrasonography are effective as a first diagnostic step in evaluating postmenopausal bleeding.[5] Other studies have shown that an endometrial biopsy is as effective as dilation and curettage in detecting endometrial cancer.[6] Endometrial biopsy should remain as a first-line diagnostic tool for abnormal uterine bleeding.
Enhancing Healthcare Team Outcomes
The female patient should be educated by the gynecologist, primary care provider, and the gynecology nurse that endometrial biopsy is a procedure that, without debate, has clinical importance when evaluating abnormal uterine bleeding or postmenopausal bleeding. This education is part of the collaborative, interprofessional healthcare team approach to preparing for and performing this procedure. However, there is currently a debate on whether an endometrial biopsy should be used to evaluate infertility. Chronic endometritis is a bacterial infection of the endometrium that causes an increased prevalence of immune cells in the endometrium, and this change in histology can adversely affect fertility. There is a prevailing opinion that because chronic endometriosis is often asymptomatic, it can only be diagnosed through an endometrial biopsy. Therefore endometrial biopsy should be performed in the evaluation of infertility.[7] [Level 1] However, the American Society for Reproductive Medicine and the Choosing Wisely Campaign recommend against endometrial biopsy in the evaluation of infertility. They cite evidence that the endometrium's histological dating does not determine infertility, and the presence of chronic endometritis does not affect the cumulative live birth rate.[8][9] [Level 1]
For abnormal uterine bleeding, the American College of Obstetricians and Gynecologists support recommendations that include differences in the indications for endometrial sampling in women based on age. In women younger than forty-five, an endometrial biopsy is only indicated if abnormal uterine is persistent. Endometrial biopsy should also be considered if there is a history of unopposed estrogen exposure, failed medical, or women at high risk of endometrial cancer. In women over the age of forty-five, any abnormal uterine bleeding should include an endometrial biopsy in the diagnostic workup.
There is another special subset of pre and postmenopausal women in whom the American College of Obstetricians and Gynecologists provide specific guidance in their recommendations for endometrial biopsy. This includes women who are on tamoxifen therapy. An endometrial biopsy should be performed for all postmenopausal patients on tamoxifen therapy who have abnormal uterine bleeding. It is common for premenopausal women to experience menstrual irregularities, most commonly amenorrhea while taking tamoxifen. The guidelines do not suggest routine endometrial biopsy in these women. Unless there are risk factors for endometrial cancer, premenopausal women treated with tamoxifen does not require any additional screening or workup beyond routine gynecologic care.[10]