Endometrioma
- Article Author:
- Abigail Hoyle
- Article Editor:
- Yana Puckett
- Updated:
- 6/12/2020 9:45:34 PM
- For CME on this topic:
- Endometrioma CME
- PubMed Link:
- Endometrioma
Introduction
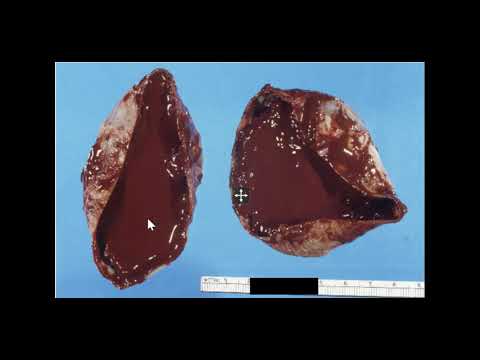
Endometriosis is a common, estrogen-dependent, inflammatory, gynecologic disease process in which normal endometrial tissue is abnormally present outside of the uterine cavity. Endometriomas are cystic lesions that stem from endometriosis. Endometriomas are most commonly found in the ovaries. Affecting approximately 10% of reproductive-aged women, endometriosis is a common cause of chronic pain, dyspareunia, dysmenorrhea, and infertility. Most commonly, endometriosis is found within the pelvis, specifically on the ovaries.[1] Endometriomas are the most common manifestation of endometriosis on the ovary. However, implants can also be found throughout the abdomen, such as on the bowel, within prior surgical incisions, and even in rare cases in distant locations of the body such as the cerebellum.[2] Approximately 17-44% of women diagnosed with endometriosis will experience an endometrioma. These lesions are commonly referred to as chocolate cysts, due to the thick dark brown appearance of the fluid that is contained within them.[3] Endometriomas indicate a more severe disease state in patients with endometriosis and can lead to specific issues in these patients, such as decreased ovarian reserve.[4]
Etiology
Endometriomas are most commonly thought to be caused when a seeding of ectopic endometrial tissue, most often present on the ovary, bleeds, causing a hematoma. This commonly occurs with the natural menstrual cycle of a woman, due to the fact that the ectopic endometrial tissue is still hormonally active. Therefore, this tissue will naturally shed with the withdrawal of progesterone after the breakdown of the corpus luteum.[5] However, unlike normal hematomas, such as those seen in the ovary with ovulation, these are lined with sticky endometrial stroma and glands and contain more fibrous tissue. Therefore, these are more commonly seen with adhesions present to surrounding areas, which can cause significant pain for the patient and can create various challenges for the surgeon during surgical resection of an endometrioma.[6]
When discussing the etiology of endometriomas, it is always appropriate to mention the etiology of endometriosis as well, since this is the foreshadowing condition to an endometrioma. However, the etiology of endometriosis is a controversial discussion in the medical community. The oldest and most widely accepted theory for the development of endometriosis is retrograde menstruation. This theory suggests that endometriosis develops from the endometrial tissue traveling in a retrograde manner through the fallopian tubes and into the pelvis during a woman’s natural menstrual cycle. This tissue then travels and seeds in different areas, creating the endometriosis lesions. Some of these lesions may seed to an ovary and begin the process for an endometrioma, as discussed above.[7]
This theory of retrograde menstruation is likely a contributing factor to the development of endometriosis. However, most people in the medical community feel that it is more of a multifactorial development. For instance, it is difficult to believe this theory in women who have distant endometriosis lesions, or pre-pubescent females with endometriosis. Therefore, other theories that have been suggested include the theory of metaplasia. This theory suggests that extrauterine cells undergo metaplasia and transdifferentiate into endometrial cells. Another prominent theory is that viable endometrial cells get seeded via hematogenous and lymphatic spread. No one theory has been fully proven, and it is likely a combination of these theories mentioned above.[8]
Epidemiology
Endometriosis, in general, has been found to affect approximately 10% of women of reproductive age. However, only about 3% of reproductive-aged women have clinically significant disease.[9] Among this 3%, there are specific populations in which endometriosis is quite prevalent. For example, endometriosis has been found in nearly 50% of women experiencing issues with infertility, and nearly 70% of women with pelvic pain.[10][11]
There is limited data when looking specifically at the prevalence of endometriomas. However, it is estimated that 17-44% of women with endometriosis experience an endometrioma,[12][13] and 28% of these women will have bilateral endometriomas.[14] In the specific population of subfertility, approximately 17% of these women are found to have endometriomas.[15]
There is also limited data to suggest specific risk factors for endometriomas alone.[16] However, there are known risk factors for the development of endometriosis in general.
These include:
- Nulliparity
- Early menarche (typically before 11-13 years old)[17]
- Late menopause, short menstrual cycles (less than 27 days)[18]
- Heavy menstrual bleeding[18]
- Mullerian anomalies[19]
- Height greater than 68 inches[20]
- Low body mass index (BMI)[18]
- Consumption of high amounts of trans unsaturated fat[21]
- Exposure to diethylstilbestrol in utero[22]
In addition to risk factors for endometriosis, there are also certain things that having endometriosis puts you at an increased risk for. Many of these have been previously discussed, such as infertility, chronic pelvic pain, dyschezia, dyspareunia, and dysmenorrhea. However, it has also been found that women with endometriosis have an increased risk for certain types of ovarian cancer. The overall risk of ovarian cancer remains low. However, multiple studies have demonstrated women with endometriosis having a higher incidence of clear cell and endometrioid ovarian cancer.[23] There was one study in particular from Finland, which only found this increased risk in women who had endometriomas.[24]
Pathophysiology
The pathophysiology of endometriomas is the same as endometriosis in general, due to the fact that endometriomas are a subset of this larger medical condition. The pathway for this disease process occurs with the hormonal response of the ectopic endometrial tissue. This tissue responds to the cyclical hormonal changes of a woman’s menstrual cycle in just the same way that the intrauterine endometrium does. It will become proliferative, secretory, and slough just as it would if it were within the uterus. With these fluctuations comes varying concentrations of cytokines and prostaglandin molecules.
Cytokines and prostaglandins are signaling molecules for the creation of an inflammatory response, and thus generate inflammation in the area of the endometriotic implantation. This inflammatory response then lays the foundation for the production of new vascularization and new fibrous tissue formation. This snowball effect then creates the adhesions and pain that are commonly associated with this disease process. These issues also lead to the main complications of this disease, such as infertility and chronic pelvic pain. Patients with endometriomas have a more severe disease state, and therefore typically experience this on a more significant scale than those with stage 1 or 2 endometriosis.[9][25][26]
Histopathology
The only way to confirm the diagnosis of endometriosis, including endometriomas, is to surgically diagnose it with direct visualization and tissue samples. In order to confirm the presence of endometriosis in the tissue, the biopsy must contain both endometrial glands and stroma.[27]
History and Physical
History
In general, patients with symptomatic endometriosis are frequently nulliparous females of reproductive age with a chief complaint of heavy or painful menses. Their periods will often last longer than 7 days. They may complain of chronic pelvic pain, pain with sexual intercourse, or defecation (see a full list of symptoms below). Their periods are typically regular in nature, though they may have shorter menstrual cycles (less than 27 days). The onset of pain for these patients is typically 2-3 days prior to the onset of their menses, and the pain typically begins to resolve a couple of days after their menses has started.[1]
Endometriomas can cause severe pain. They are most commonly found on the ovaries, and the pain is typically isolated to the side of the lesion. However, depending on the extent of their disease and the laterality of their lesions, patients may experience bilateral or generalized pain. If an ovarian endometrioma ruptures, the thick endometrial fluid can spill throughout the abdomen and cause significant pain and inflammation. These patients often present with an acute surgical abdomen.[28]
Although endometriomas are most commonly found on the ovaries, it is important to remain vigilant with patients that come in with complaints of pain. Endometriomas have been found in other unsuspecting places. For example, there are many documented cases of endometriomas being present within abdominal surgical incision scars. Endometrial implants have also been documented within the lung parenchyma and the brain. Therefore, if a patient is complaining of pain that is cyclical in nature with their menstrual cycles, endometriosis is something to keep in mind, regardless of where the pain is located.[2][29]
Symptoms
- Pelvic pain
- Heavy menses
- Painful menses
- Back pain
- Painful sexual intercourse (dyspareunia)
- Painful defecation (dyschezia)
- Painful urination (dysuria)
- Urinary frequency
- Nausea/vomiting
- Bloating[30]
Physical
Endometriosis, including those with endometriomas, typically has minimal findings on physical exam. Endometriomas, if large enough, could be felt on a bimanual exam. However, apart from this, there are few abnormal findings in these patients. You will often find generalized pelvic tenderness or tenderness to the affected area. However, this can also be sensitive to the timing of the exam with respect to the patient’s menstrual cycle. The patient will often have more pain if the exam is completed just before the onset of her menses in comparison to if it was done just after her menses completed. Other possible findings on the bimanual exam include a fixed or retroverted uterus, suggesting scarring secondary to endometriosis. At times, nodularity of the uterosacral ligaments can also be palpated.[31][32][33]
However, if a patient presents after the rupturing of an endometrioma, the patient could have an acute abdomen upon evaluation. These findings include peritoneal signs, which commonly present as abdominal rigidity, rebound pain, and involuntary guarding.[28]
Evaluation
Endometriomas can often be visualized on imaging. However, they appear similar to other cystic lesions on imaging, and final pathology is only discovered through surgery. If these findings are not seen on imaging, then the diagnosis becomes even more elusive. It is important to remember that the definitive diagnosis of endometriosis is done through surgical visualization of the lesions. Therefore, there is no diagnostic test that can be done. However, there are a limited number of tests that can be used as a tool to assist with the diagnosis.
Laboratory evaluations that can be considered for these patients include a complete blood count (CBC), cancer antigen (CA)-125, CCR1, urinalysis, and sexually transmitted infection (STI) testing. The CBC can help guide the concern for infection and anemia. If there is an elevated white blood cell count, the suspicion for an infectious cause of the patient’s pelvic pain would be higher. The hemoglobin can also help guide you to the level of blood loss, as these patients typically have heavier periods and may be anemic as a result. CA-125 can be elevated in women with endometriosis. However, this is a non-specific marker, and it is not routinely ordered.[1] CCR1 is a new lab marker that has been shown to be higher in peripheral blood leukocytes of women with endometriosis. This is not yet commonly ordered as a standard practice but could be a test to consider in these patients while completing their work-up.[34] It is also important to complete a urinalysis to rule out a UTI from the differential diagnosis, as well as STD testing such as cervical cultures for gonorrhea and chlamydia in order to rule out these infections.
When it comes to imaging, a transvaginal ultrasound is commonly ordered for these patients to determine if there is a cause for their pelvic pain that can be visualized. Superficial implants of endometriosis cannot be seen on ultrasound, nor any other imaging modality. However, ultrasound is often where endometriomas are found. Endometriomas typically appear as simple cysts. However, they can also be seen as multi-loculated cysts or cystic-solid lesions. The typical appearance of these lesions on ultrasound shows low-level homogenous echos, otherwise described as ground-glass appearance. This is consistent with old hemorrhagic debris. These lesions are also typically devoid of any vascularity when examined with doppler flow.[35][36]
Other imaging modalities that can be considered are magnetic resonance imaging (MRI) and computed tomography (CT). MRI has actually been shown to have a higher sensitivity for detecting a pelvic mass than ultrasonography. However, due to the cost of an MRI, the benefit does not outweigh the financial burden, and thus ultrasound is more commonly used. Like ultrasound, MRI is limited in detecting diffuse pelvic endometriosis, and may only be beneficial for finding endometriomas.[36] CT scan exposes the patient to radiation, and although it may identify a pelvic mass, the characteristics of the mass on CT scan do provide good clues as to the type of mass it is. Therefore, a CT scan is not the ideal imaging modality in these patients.
The gold standard for the diagnosis of endometriosis is via laparoscopy. Due to the fact that imaging and laboratory studies are of limited benefit in the diagnosis of endometriosis, direct visualization through surgery is the standard. During laparoscopy, endometriosis lesions will typically appear blue or black in color. However, they can be seen as red, white, or non-pigmented lesions. At this time, severity of the disease can also be evaluated. If there are significant adhesions, peritoneal defects, or endometriomas present, this is indicative of more severe disease. The visualized lesions can then be biopsied and evaluated by pathology for endometrial glands and stroma.[37] If the patient is also experiencing infertility issues, chromotubation can also be completed at this time to assess tubal patency.
Laparoscopy is an important procedure in patients with endometriosis, because although it is diagnostic, it is also therapeutic, especially in cases with endometriomas. This is an important part of treatment for these patients with refractory endometriosis or patients with symptomatic endometriomas.
Treatment / Management
Treatment of endometriosis mainly consists of hormonal medications or surgical treatment. Milder forms of endometriosis can be treated with oral contraceptive pills, various forms of progesterone (oral pill, intrauterine device), gonadotropin-releasing hormone (GnRH) agonists (such as leuprolide), or androgens (such as danazol.[38][39][40] However, once a patient’s endometriosis has become severe enough to have the presence of an endometrioma, surgical management is typically preferred. GnRH agonists have been shown to decrease the size of endometriomas. However, patients have not reported any difference in their pain.[41][42][43][44] Therefore, this option is typically abandoned for patients with endometriomas.
Surgical treatment of endometriosis can range from more conservative approaches to more radical approaches based on the patient’s symptoms and desire for future fertility. Conservative surgery consists of the destruction of endometrial lesions (typically with laser or cautery), drainage of the endometrioma, and removal of the cystic capsule.[45] However, if a patient’s pain is severe, and they do not desire future fertility, some patients undergo total hysterectomy with bilateral salpingo-oophorectomy as a more definitive treatment.
Surgeries, especially more conservative options, are typically completed laparoscopically. In surgical resection of an endometrioma, it is important to strip the cyst wall during the procedure instead of simply draining the cyst. This has been shown to decrease recurrence rates.[45] If a patient is having difficulties with fertility, resection of an endometrioma has been shown to improve natural pregnancy rates.[46]
The main issue with surgical endometrioma resection, especially in women experiencing infertility and considering IVF, is the question of whether it affects the amount of ovarian reserve. Women have been shown to have a lower AMH (anti-mullerian hormone) level after cystectomy, which is a hormone used by fertility specialists to measure ovarian reserve.[47] There has also been a reported 2-3% of patients having ovarian failure after resection of bilateral endometriomas.[48] Therefore, these are important risks to consider when choosing whether surgery is appropriate for each patient, given their fertility desires. Due to this limited data, if patients are already being seen by a fertility specialist, and IVF is being considered, endometriomas are most often managed expectantly. The exception to this is in cases of severe symptoms or issues with egg retrieval caused by the endometrioma.[49]
After surgery, some providers place patients on medical therapy to attempt to prevent a recurrence. There have been studies that show a 6-month course of oral contraceptive pills helps to prevent recurrence. However, this treatment option again depends on the patient and whether or not they are trying to conceive.[50][51]
Differential Diagnosis
When evaluating patients that have suspected endometriomas, it is important to consider all possible conditions. Given the ambiguous presentation of endometriomas and endometriosis in general, it can present similarly to other conditions.[18]
Often times, these patients present with ambiguous pelvic pain. Therefore, important conditions to keep on your differential are other sources of pelvic pain. These include:
- Ectopic pregnancy
- Appendicitis
- Pelvic inflammatory disease
- Ovarian torsion
- Diverticulitis
- Urinary tract infection
- Ovarian cyst (other than endometrioma)
- Sexually transmitted infections (gonorrhea, chlamydia)
If an adnexal mass is present and known from imaging, there are characteristics of the mass that can indicate what kind of adnexal mass it is. Endometriomas, as discussed in the evaluation section above, have a characteristic ground glass appearance on ultrasound. These findings are also similarly seen in hemorrhagic cysts, and often the diagnosis between the two is not made until the time of surgery. Therefore, when dealing with imaging evidence of endometriomas, it is important to consider hemorrhagic cysts on the differential diagnosis.[52]
Also, when a patient is presenting with an acute abdomen, and there is concern for a ruptured endometrioma, the most important things to keep in mind are ruptured ectopic pregnancy and ovarian torsion. These are all surgical emergencies that must be taken to the operating room as soon as possible.
Surgical Oncology
Endometriomas carry a small risk of upgrading to malignancy specifically to epithelial ovarian cancers. However, that risk appears to be low. A meta-analysis of 13 studies and approximately 9000 women with epithelial ovarian cancers showed that a self-reported history of endometriosis was three times as high.[53] There may be a gene activation of KRAS and PI3K associated with ovarian cancer and history of endometriomas. In addition, genes such as PTEN and ARID1A have been implicated in the pathogenesis of cancer in such lesions as well.[54] However, on their own, these lesions are not considered premalignant, and no staging workup or screening is required.
Staging
There are 4 stages of endometriosis described by the American Society for Reproductive Medicine. The stages are minimal, mild, moderate, and severe. Staging is completed surgically, most commonly via laparoscopy.[25][26]
- Stage I (minimal): Small solitary lesions without significant adhesions
- Stage II (mild): Superficial lesions < 5 cm, without significant adhesions
- Stage III (moderate): Multiple deep implants, small endometriomas unilaterally or bilaterally on the ovaries, and thin adhesions
- Stage IV (severe): Multiple deep implants, large endometriomas unilaterally or bilaterally on the ovaries, thick adhesions
As can be seen by these descriptions, if an endometrioma is present, the patient is already a stage 3 or 4. Most patients are found to have stage 1 or 2 endometriosis. However, staging does not always coincide with the severity of symptoms.[26]
Prognosis
The overall prognosis for patients with endometriosis is favorable. This is a benign disease. However, it is a chronic condition and can be progressive. Patients with endometriomas signify those with more severe disease and thus can have more long term complications from the disease. Even if treatment is effective for patients for a time, it is, unfortunately, a condition that has a high level of reoccurrence. Therefore, the main issue of this disease is the lack of a truly definitive treatment and therefore, can cause long term issues such as pain and infertility. Thankfully, most women have an improvement in their symptoms once they become menopausal due to the lack of cyclical hormonal signaling.[1]
Complications
The two main complications of endometriomas are the same as endometriosis in general. These complications, as discussed previously in this article, include chronic pelvic pain and infertility. In addition, if the endometrioma is 6 cm or large, this puts the patient at increased risk for ovarian torsion, which is a surgical emergency and can lead to loss of the ovary.[9] Women with endometriosis have an increased risk for certain types of ovarian cancer, and endometriomas carry a small risk of upgrading to malignancy, although the risk of these is very low.
Deterrence and Patient Education
When caring for patients with endometriomas, it is important to discuss the expectations for treatment and possible complications of having endometriosis. Endometriomas are treated using laparoscopic surgery. Therefore, it is important that the patient is educated on the risks and benefits of laparoscopic surgery prior to undergoing a laparoscopic cystectomy. It is also important that the patient understand that endometriomas are developed from having endometriosis, which is a chronic condition. The patient should be advised that approximately 25% of women experience a reoccurrence of an endometrioma. Apart from reoccurrence, the patient may also experience issues with fertility and chronic pelvic pain related to their underlying endometriosis, and these issues may require further treatment.
Enhancing Healthcare Team Outcomes
Due to the fact that endometriosis and endometriomas are part of a chronic condition that has the potential to be widespread in the body, an interprofessional team approach is important. For patients with more mild forms of endometriosis, that do not yet have a cystic component to their disease or do not want surgery, medications are an important part of treatment. It is important to discuss these treatments with a pharmacist who can help determine the ideal length and methodology to provide these patients with the best relief.[38]
When initially evaluating these patients, most often, they will get a pelvic ultrasound. It is very important when looking at any adnexal masses to describe them appropriately. There are certain characteristics that endometriomas have that can make your suspicion higher when evaluating the images. Therefore, radiologists play an important role in diagnosis. This also helps answer the question of whether or not surgery is most appropriate for each patient. Radiologists can also help indicate whether or not other structures are involved, which is extremely important if surgery does, in fact, occur.[36]
Endometriosis can lead to multiple adhesions and endometriosis implants. These lesions can, at times involve the bowel or the bladder. In severe disease, there may be bowel obstructions or ureteral involvement.[55][56] In these cases, general surgery or urology may need to be involved in order to complete the necessary surgical procedures.
If patients do opt for surgical treatment, which is often the case for endometriomas, there are additional team members that come together to provide appropriate care for the patient. Anesthesiologist evaluation of the patient for appropriate anesthesia is important to assist with a smooth surgery and good post-operative pain control. Nursing care in both the pre-operative and post-operative period is important so that the patient is given the appropriate medications at the right time. Finally, pharmacy assistance for appropriate post-op pain control is also an important role for the ideal care of the patient.