
Eyelid Myokymia
- Article Author:
- Abd Alkader Jafer Chardoub
- Article Editor:
- Bhupendra Patel
- Updated:
- 8/15/2020 12:38:12 AM
- For CME on this topic:
- Eyelid Myokymia CME
- PubMed Link:
- Eyelid Myokymia
Introduction
Eyelid myokymia is the commonest type of facial myokymia.[1][2] It is a condition that consists of spontaneous, gentle, constant, rippling contractions that spread through the affected striated muscle. The orbicularis oculi is the most affected muscle (Video).[3] This condition is likely to be unilateral, affecting the lower eyelid more frequently than the upper eyelid.[4] These contractions are self-limited, periodic, and lasting seconds to hours. Occasionally, the contractions become chronic and continue for several days or even a few weeks before resolving.[4] Female gender and cold weather are risk factors for chronic eyelid myokymia.[5] In rare cases, ipsilateral upper and lower eyelids involvement can occur at the same time.[4]
Anatomy of the Eyelid
The eyelid consists of three lamellae (Fig). The anterior lamella consists of the skin and orbicularis oculi muscle. The middle lamella is a combination of the orbital septum, suborbicular fibro adipose tissue, and orbital fat. Lastly, the posterior lamella includes the tarsal plate, the retractors, and the conjunctiva.[6]
The orbicularis oculi ( OO ) muscle is a superficial striated muscle (Fig). It is directly responsible for eyelid closure. Its fibers interlock with a fibrous aponeurotic system that is directly attached to the dermis of the lid skin. The orbicularis oculi muscle has three portions, a pretarsal portion directly in front of the tarsal plates, a pre-septal portion over the orbital septum, and the orbital portion which extends to the eyebrow superiorly and the cheek inferiorly. It gets nerve supply from the temporal and zygomatic nerves, which are branches from the facial nerve. The medial upper and lower eyelid orbicularis oculi muscle receives innervation by the terminal superior branches of the buccal branch of the facial nerve.
The facial nerve originates from the brain stem (the pons). It divides within the parotid gland into the temporofacial and cervicofacial divisions. The temporal and zygomatic nerves (terminal branches from the temporofacial division) make upper and lower nerve plexuses that innervate the orbicularis oculi muscle.[7] The terminal branches of the buccal facial nerve supply the medial upper and lower eyelid orbicularis muscle (Fig).
Etiology
The etiology of eyelid myokymia is not entirely understood.[8][5] However, it usually occurs in healthy persons and is precipitated by fatigue, anxiety, stress, exercise, and caffeine consumption.[2][4]
Medications like topiramate, clozapine, gold salts, and flunarizine can trigger eyelid myokymia. Nonetheless, medication-induced myokymia is uncommon.[9] Other reported causes include multiple sclerosis, autoimmune diseases, and brainstem pathology such as pontine glioma.[4]
Epidemiology
Current literature regarding the prevalence and incidence of eyelid myokymia is scarce. However, it tends to affect healthy young subjects.[10] It is sometimes called the "medical students' disease" because of the frequency with which it seems to affect medical students, especially at times of stress.
Pathophysiology
The pathophysiology of eyelid myokymia remains incompletely understood. Electrophysiologically, a single motor unit discharges rhythmic or semi-rhythmic spurts at a rate of 3 to 8 Hz, although rates as high as 60 Hz have been noted. These discharges are separated by intervals of 100 to 200 millisecond and are not synchronized in muscles. Although spontaneous discharges may increase with voluntary movements, they do not initiate from such activities.[9]
History and Physical
History
The most common symptom of eyelid myokymia is lower eyelid twitching. Clinical evaluation of individuals with the symptoms mentioned above includes a full medical history and include questions about precipitating factors like smoking, caffeine intake, lifestyle, and medications.
Physical Examination
On examination, fine contractions of the orbicularis oculi muscle may be noticeable. These contractions are more apparent to the patient than visible to the spectator. When the eyelid is pulled manually, the symptoms often improve. Infrequently, the contractions may induce movement of the globe and cause mild nystagmus-like eye movements. When examing the patient, tapping on the area where the movements occur may reveal the myokymia.
Evaluation
IMAGING GUIDANCE
Selecting the proper imaging modality depends on the clinical presentation and the suspected underlying cause. Generally, routine neuroimaging studies for patients with chronic myokymia to rule out changes affecting the pons are unnecessary because of its low yield findings. According to an American study, 13 of 15 patients who underwent computed tomographic scans (CT) or magnetic resonance imaging (MRI) had no mass or other abnormalities disturbing the course of the facial nerve or the brainstem.[8]
When necessary, an MRI scan with intravenous gadolinium contrast is the optimal imaging modality because it images the whole facial nerve pathway.
The sequences of facial nerve imaging:
- MRI of the brain to show the central pathways of the nerve.
- MRI of the skull base and the parotid glands to detect masses associated with the extra-temporal facial nerve.
- MRI of the temporal bones to evaluate inflammatory lesions, meningeal abnormality, and perineural extent of disease along the nerve inside the temporal bones.
- CT scan in combination with MRI or as an alternative if there were contraindications or intolerance to MRI.
- Ultrasound can evaluate abnormalities within the parotid gland.[11]
Treatment / Management
Conservative management is the recommendation for patients with isolated eyelid myokymia. Rest, decrease or elimination of risk factors, such as alcohol drinking, smoking, and caffeine intake are effective ways to manage eyelid myokymia. In case of persistent myokymia for more than three months, more interventions may be necessary. Botulinum toxin injections are first-line treatment and have a high rate of success.[8]
Depending upon the extent of the fasciculations, between 5 and 20 units of botulinum toxin are administered. Other treatments for chronic eyelid myokymia have been suggested, such as tonic water, calcium, folic acid, phosphorus, potassium, and multi-vitamins. However, no objective evidence exists to support these treatments.[5] Orbicularis myectomy is very rarely if ever, indicated.
Differential Diagnosis
While eyelid myokymia refers to spontaneous, gentle, constant, rippling contractions, other conditions can also be mistaken for eyelid myokymia as they may present similarly such as:
- Hemifacial spasm
- Essential blepharospasm
- Meige syndrome
- Spastic–paretic facial contracture
Prognosis
Isolated eyelid myokymia has a good prognosis. It is a benign condition and is unlikely to develop into other facial movement disorders or to be related to other neurologic illnesses. Most patients will notice a spontaneous improvement in symptoms over a few months. Stress and anxiety reduction are often prescribed but of little scientific value. Most patients will obtain a complete resolution after just one injection with botulinum neurotoxin. However, it is difficult to determine if this outcome was a direct result of the management, or just coincident with the condition's nature.[8]
Complications
Although eyelid myokymia is a benign condition, it may be the initial presentation of other diseases which can affect other muscles on one or both sides of the face:
- Hemifacial spasm
- Essential blepharospasm
- Meige syndrome
- Spastic–paretic facial contracture[8]
Deterrence and Patient Education
Eyelid myokymia is a self-limited condition. Usually, it resolves within a few days or weeks with rest and avoiding triggering factors.[8]
A specialist referral is indicated in patients with myokymia if:
- The twitching does not resolve within a few weeks.
- Twitching develops in other parts of the face.
- There is difficulty opening the eye.
- There is complete eyelid closure with each twitch, which may indicate a hemifacial spasm rather than myokymia.
- Redness or swelling of the eyelid
- Drooping of the eyelid
Enhancing Healthcare Team Outcomes
Eyelid myokymia is often observed in clinical practice by eye care providers, emergency physicians, and nurses. Although this condition is best managed conservatively, a referral to the ophthalmologist is important in cases that persist or if there is a suspicion of an underlying problem and for proper management, if it becomes debilitating. Good communication between health care providers is required to improve patients outcomes.
(Click Image to Enlarge)
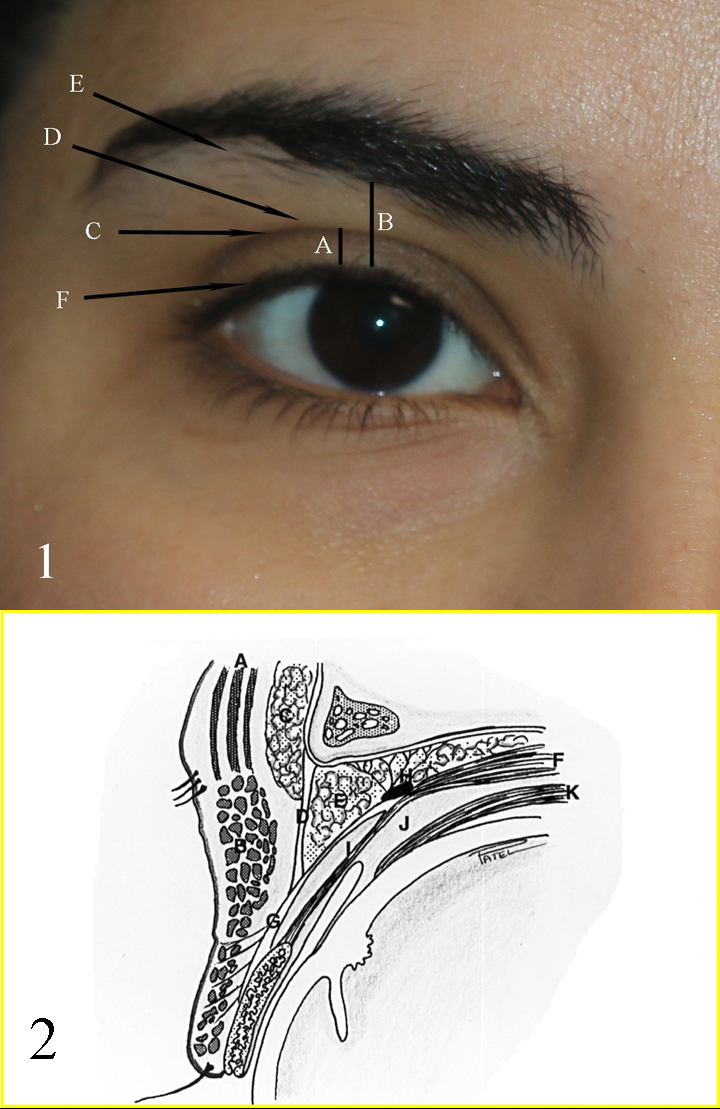
Fig 1: A: upper eyelid platform; B: Brow to Lid margin distance; C: Upper eyelid crease; D: Upper eyelid fold; E: Brow fatpad; F: Eyelid margin and eyelash curve Fig 2: A: Frontalis muscle; B: Orbicularis muscle; C: Brow fat pad; D: Orbital septum; E: Preaponeurotic fat pads; F: Levator muscle; G: Levator aponeurosis; H: Whitnall ligament; I: Muller muscle; J: Common sheath; K: Superior rectus muscle
Contributed by Professor Bhupendra C. K. Patel MD, FRCS
Contributed by Professor Bhupendra C. K. Patel MD, FRCS
(Click Image to Enlarge)
(Click Image to Enlarge)

Innervation of the Orbicularis Oculi Muscle: the temporal branch supplies the lateral and superior part of the orbicularis oculi (not shown). The lateral and lower eyelid orbicularis is supplied by branches of the zygomatic branches. The most medial lower and upper eyelid orbicularis muscle is supplied by the terminal buccal nerve branches
Contributed by Professor Bhupendra C. K. Patel MD, FRCS
