Autologous Fat Grafting For Facial Rejuvenation
- Article Author:
- Advait Vasavada
- Article Editor:
- Blake Raggio
- Updated:
- 5/17/2020 11:41:44 AM
- For CME on this topic:
- Autologous Fat Grafting For Facial Rejuvenation CME
- PubMed Link:
- Autologous Fat Grafting For Facial Rejuvenation
Introduction
Fat grafting is a technique where the harvested adipose tissue is injected into various compartments underneath the skin. The term autologous fat grafting refers to the procedure where the source of fat is the same person on whom it is to be used. For many years this technique has been used for a variety of different purposes. Autologous adipose tissue is considered by many to be an ideal filler material for facial rejuvenation, as it represents one of the most biocompatible dermal fillers with low allergenicity, produces a soft and natural result, and may have semi-permanent to permanent effects. This article is focused on the utility of this procedure for facial rejuvenation.[1]
Anatomy and Physiology
As the human body ages, there are several age-related changes that occur to the face. Gravity causes descent of the facial soft tissues and creates unpleasing folds and shadows (e.g., nasolabial folds, tear troughs, marionette lines, etc.) often associated with an aged appearance. Moreover, patients experience a decrease in facial volume secondary to a combination of dermal thinning, muscular atrophy, fat volume loss, and reduction in girth of bones.[2] While gravity-related changes are traditionally addressed with "lifting" procedures such as facelift, browlift, and neck-lift, to name a few, the loss of facial volume can be addressed with various filler materials (e.g., fat grafting) and has recently gained popularity as an adjunctive target for those who perform facial rejuvenation procedures.[3]
The study of facial anatomy and its structural relationships is necessary for performing this procedure well and limiting the complications.[4]
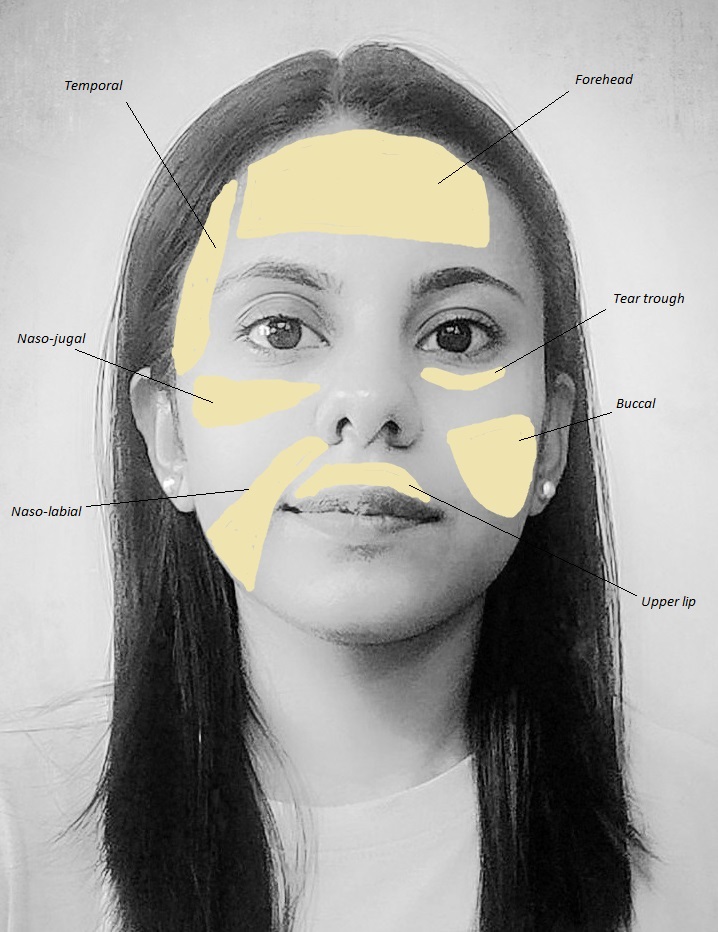
The harvested fat, often taken from the flank, inner thigh, or abdomen, has to be injected into the selected tissue planes only after careful planning. Identifying the proper location and depth of the fat compartment to be addressed is paramount. The major compartments of the face for the purpose of rejuvenation include the following:[5]
- Superficial fat space
- Superficial musculoaponeurotic system
- Deep fat space
Each of these spaces can be further divided into units on the same plane. It requires considerable experience to understand the outcome of injecting into the different spaces. The reader is directed to further review of the various compartments of the face and their relation to aesthetic procedures.[6]
Lastly, the face can be divided into several units to plan facial rejuvenation. Understanding of these units enables the surgeons to select appropriate sites of fat transfer as well as the required volume and techniques. Also, several complications can be avoided with the knowledge of working with different facial units. While a detailed description of the anatomy of the face, particularly in regard to aging, is beyond the scope of this paper, the reader is directed to further reading.[2]
Indications
Facial rejuvenation, in its essence, represents any procedure (surgical and non-surgical) employed to make the face look younger. Autologous fat grafting intended for facial rejuvenation not only restores volume to the face but also can revitalize skin by improving tone and texture.
The age-related changes in the face that can be addressed and/or camouflaged with autologous fat grafting include:
- Forehead hollowing
- Deep rhytides, particularly forehead and glabellar
- Temporal hollowing
- Supraorbital hollowing
- Increased vertical length of the lower lid
- Tear trough deformity and/or deep nasojugal groove
- Malar bags
- Nasolabial fold
- Marionette lines
- Jowls
- Deflated lips
- Weak chin
- Poor jawline contour
Apart from treating the aging face, autologous fat grafting has utility for several other problems that can be performed either alone or in conjunction with facial rejuvenation.[7] The indications concerning the face include:
- Rhinoplasty
- Scars
- Burns
- Radiation dermatitis
- HIV-associated lipodystrophy
- Facial deformity - congenital, acquired or traumatic
- Facial asymmetry
- Flap augmentation
Contraindications
There are instances where fat grafting may not be the ideal rejuvenation procedure and could be unsafe in certain scenarios, particularly if a general anesthetic is to be employed. Hence, it may be contraindicated for the following reasons:
- Extensive burn scars
- Lid retractions
- History of keloid formation
- Coagulopathy
- Lipid metabolic disorders
- Severe chronic disease
- Deep vein thrombosis
- Pulmonary embolism
Equipment
Fat grafting requires the following equipment:
- Wetting solution - 500 mL normal saline, 25 mL of 1% to 2% lidocaine, 0.5 ml epinephrine (1:100,000 or 1:200,000)
- Local anesthetic
- Infiltration needle or cannula - used to administer local anesthesia (to cannula entry sites) and the wetting solution (to graft donor sites)
- Fat harvesting and donor cannulas - The Coleman type II (side-port cannula) is the most commonly used cannula. The length of this instrument should be 5 cm to 9 cm when used on the face. The choice of this instrument, including gauge and length, depends largely upon the graft recipient area as well as upon the experience and comfortability of the surgeon.
- Luer-lock syringes - large syringes (10 cc or 20 cc) for harvesting, and several 1 mL syringes for injecting
- Scalpel - to create an entry site for cannulas
- Sterile markers
- Gauze
- Compression garment
- Closed suction machine (low power suction may be used if harvesting large amounts of fat, though this may be traumatic and affect the integrity of the harvested fat)
- Plug that seals the Luer-Lok
- Leur-to-Leur connector for micro-fat and nano-fat (for skin regeneration) processing
Based on the method of fat processing (e.g., sedimentation, filtering, washing, and centrifugation), the following may be required:
- 1 cc syringes with absorbent material (e.g., gauze) to soak up supernatant oil
- commercial fat grafting preparation kits (multiple available)
- Strainer and saline
- Centrifuge (recommended setting per Coleman is 3000 rpm for 3 min to isolate the fat with minimal trauma)
Personnel
The team performing a fat grating may include attending and resident surgeons, anesthesiologists, nursing staff, and operative room technicians.
Preparation
Informed consent should be obtained. The patient should understand all of the risks and benefits and alternatives to the procedure. It is important to manage the expectations of the patient and address any questions about the procedure he/she may have. Also, the possibility of revision procedures has to be explained as a sizeable fraction of the patients may need augmentation in the future.
Pre-operative evaluation and consultation with a physician are required to obtain the clearance for the surgery. This is important as certain medical conditions like bleeding disorders, anemia, and certain drugs like NSAIDs may affect the outcome of the surgery. A patient on aspirin or NSAIDs may have to stop taking the medication 2 weeks before the surgery.
Pre-operative photographs should be obtained. The selection of potential fat donor sites should be discussed beforehand. Also, the recipient site is carefully examined to determine the amount of fat needed for the procedure.
Before the surgery, the necessary donor and recipient sites have to be prepared. In men, facial hair may need to be removed for better visualization. The zones of adherence (ZOA) are areas of increased fibrosis that should be avoided as liposuction to these regions increases the risk of trauma and/or contour irregularities. Hence, these areas should be marked in advance to avoid them.[8]
At the time of surgery, a general anesthetic procedure may require repeat evaluation by the anesthesiologist. After transfer onto the table, the patient may be given the anesthesia. For local anesthesia, it is recommended to use a nerve block rather than local infiltration as lidocaine can affect the fat graft viability.
Technique
There are three stages involved in fat grafting:[9][10][11][12]
- Fat harvesting
- Fat processing
- Fat transfer
Fat Harvesting
Fat is retrieved from the donor sites, which have a rich fat reservoir. The most common donor sites are the abdomen, periumbilical area, buttocks, medial, lateral, and anterior thigh.
The first step in harvesting fat is to use a wetting solution for adipose tissue suspension. The composition of the wetting solution for facial rejuvenation cases, which are often smaller than other fat grafting cases (e.g., breast reconstruction) and may be performed under local anesthesia, the composition of the wetting solution may resemble the following ratio: 500 mL normal saline, 25 mL of 2% lidocaine, 0.5 mL epinephrine (1 to 100,000). The solution is then infiltrated to the area from where the fat has to be retrieved, usually in a 1:1 ratio to the amount of fat planning to be harvested (i.e., if 50 cc of fat is to be harvested, then 50 cc of the wetting solution should be injected).
After 15 minutes of allowing the anesthetic to take effect, a stab incision is made with a scalpel. A blunt fat harvesting cannula attached either to a Luer lock syringe or a closed suction machine with low negative pressure is inserted into the donor site, and the fat is removed by a gentle back and forth movement. Appropriate care should be taken to adjust the technique so that there's minimal blood during this process, as blood may negatively affect the graft's viability. The plunger should be drawn back just 1 mL to 2 mL to create adequate negative pressure. If a suction machine is used, the machine should be set at the lowest tension to lessen the shear stress on the adipocytes and thus promote viability.
Fat Processing
Following the harvest of the fat, several redundant components like oil, dead adipocytes, blood, and local anesthetics are also present in the solution. The presence of any of these may compromise graft uptake by promoting graft necrosis, inflammation, and vasoconstriction. Fat processing, or refining, can be carried out by any of the following three processes:
- Sedimentation - Syringes are placed vertically for 45 minutes to use gravity to separate the different constituents. NOTE: This is the most cost-effective and causes minimal damage to the adipocytes, but is time-consuming.
- Centrifugation - Condensed fat can be obtained using 1 to 3 minutes of centrifugation at 3 rpm, as recommended by Coleman. NOTE: This is a quick and reliable method of separation of elements, though no standard centrifugation guidelines exist.
- Washing and filtering - Concentrates fat by the use of a strainer or gauze. NOTE: Cheap, relatively quick, and the adipocyte damage is minimal; once the extra material is removed, the fat is ready to be filled in the syringes for transfer.
The sedimentation and centrifugation lead to the formation of 3 layers. The middle layer contains the viable fat of interest. The uppermost layer contains oil and destroyed fat cells, which can be removed with absorbent material (e.g., gauze). The lowermost layer will have water, blood, lidocaine, and epinephrine, which should also be discarded, typical by draining the syringe containing the fat.[13]
Fat Transfer
The processed fat middle layer is transferred to multiple 1 mL syringes, and the placement of the graft is performed. Frequent hand passes of 0.1 mL are used to deliver the fat parcels. The fat should be delivered with withdrawing movements to deposit the fat with minimal resistance. The passes are also performed "3-dimensionally" in different pathways and levels, as placement in different tissue planes leads to better aesthetic outcomes. Overcorrection is a very common practice to take into account future resorption (up to 80%) of the fat, but the evidence regarding definitive survival rates is conflicting. In general, slight overcorrection (up to 30%) is acceptable. To avoid stress on the graft, compression garments are advised to be worn for 2-3 days after the procedure, though longer periods may prove useful.
NOTE: The use of platelet-rich plasma (PRP) is an emerging area where the blood of the patient may be used to extract the PRP, which is injected along with the fat to improve the chances of survival of the fat graft.[14]
Consideration of Facial Aesthetic Units
The injection of fat into the facial units is mandated by the surgeon's plan and keeping in mind the desired outcome. Every unit has its own approach with minor differences in techniques and instrument use. Here we elucidate a few general points for the more commonly injected areas of the face:[15]
- Forehead, brow, and temple: The injections given here are subcutaneous, intramuscular, or submuscular, usually accessed via the hairline or lateral brow. Any ridging during injections should be massaged out. Severely hollows temples may require up to 8 mL to 15 mL of fat.
- Glabella/Nose: the most common areas to be addressed in this region include the glabellar vertical rhytids ("11 lines") or a deepened radix or nasion (to camouflage dorsal hump). However, any contour irregularity of the nose may be addressed. The entry can be via forehead, medial eyebrow, cheek, alar base, nasal tip, or the upper cutaneous lip. Various cannulas may be employed, though the Coleman type III cannula of 19-gauge is commonly used to layer the fat from the periosteum to the intradermal layers. Fat can even be injected posterior to the cartilage for expansion of the nasal valve. For a more detailed review or non-surgical rhinoplasty maneuvers, the reader is directed to further study.[16] NOTE: Regarding the glabella, be careful to remain superficial (some advocate intradermally) to avoid intravascular injection and, thus, the risk of blindness and/or stroke.
- Periorbital area: This area is technically challenging, so a conservative approach is warranted for novice fat grafters. Take care not to place too many fat parcels at a time, going slow with a low amount of graft injected is critical. Initial infiltration is deep along the orbital rim, followed by another layer placed just above it. NOTE: To avoid palpable or noticeable bumps/lumps, stay superficial the thin skin of the eye and lack of superficial fat.
- Lips: The fat is inserted only into the most superficial level (just beneath the mucosa) to avoid the orbicularis oris muscle and superior and inferior labial arteries (branch of the facial artery). Again, cannula choice is dependent on injector preference; however, smaller cannulas (e.g., 22 gauge Coleman cannula) are preferred to inject into the lips.
- Cheek: Placement of fat in the malar, zygomatic, and infraorbital regions superior to a ptotic cheek can recreate the appearance of a centrally full cheek. Two incisions are often required, including one lateral to the mid-nasolabial fold and another lateral to the zygomatic arch. NOTE: Always mark out the location of the infraorbital nerve, approx 1 cm below the orbital rim in the mid-pupillary line to avoid direct nerve injury. Also, consider filling the area anterior to the ear (lateral cheek compartment) to avoid the face from appearing too full.
- Nasolabial fold: This area is accessed via the lateral chin or near the commissure. NOTE: Grafting can be performed both deep (periosteal) and superficial (subcutaneous), but should remain medial to the nasolabial fold to avoid trauma to the facial artery as well as to avoid deepening of the nasolabial fold.
- Mandible and chin: Fat grafting to this region can be used to address a weak chin, jows, or poor jawline definition. To gain access to this area, the incisions can be made perpendicular to the mandible, submental area, and pre-jowl sulcus. After that, the fat is placed fanning laterally and inferiorly, taking care to avoid damage to the facial artery crossing over the mandible, anterior to the masseter, at the facial notch.
Complications
Despite the most meticulous harvesting, processing, and grafting techniques, there exist several complications associated with fat grafting:
- Bruising, edema, and ecchymosis are the most common sequelae.
- Overcorrection: Due to the transfer of excess fat tissue
- Undercorrection: Due to the transfer of inadequate fat tissue or excessive resorption of grafted fat
- Pyogenic granulomas, cellulitis: Secondary to infection and/or prolonged inflammation
- Blistering
- Scarring
- Tissue bunching, palpable deformities: Often from too superficial an injection
- Contour irregularity
- Pain at the donor site: Due to inadequate anesthesia
- Deformity at the donor site: due to excessive and unequal fat harvesting, or violation of a zone of adherence (ZOA).
- Blindness: Occlusion of the ophthalmic artery
- Stroke: Occlusion of the internal carotid artery
- Fat embolism
The graft loss and bruising can be minimized by maintaining adequate atraumatic technique to ensure improved viability of graft and minimal hematoma formation. Cold compress is considered to be helpful in the first 3 days for post-operative ecchymosis, but too much icing could lead to vasoconstriction and risk graft loss. Vigorous activity should be avoided for 2 to 3 weeks after the procedure.[17]
Blindness is a rare complication of fat grafting. High-pressure injection into the supratrochlear artery causes the fat to reach the ophthalmic artery. Once the pressure is released, the fat embolizes in an anterograde direction and eventual occlusion of the retinal artery can cause blindness. The blindness that is caused by fat grafting may require urgent intervention. The patient should be transferred to the hospital immediately. The physician, at first contact, should make efforts to reduce the intraocular pressure. Timolol 0.5% drops, aspirin 325 mg, and acetazolamide 500 mg could be given to the patient while awaiting the transfer to the hospital.
Fat embolism can also cause a stroke. The signs of stroke must be observed for patients undergoing fat grafting.
Facial swelling and bruises are quite common after fat grafting. It is important to distinguish it from cellulitis that may present with fever, warmth, erythema, and tenderness. The symptoms are self-resolving but often are prolonged. The high vascularity of the face is responsible for swelling and bruising. The swelling is treated with facial lymphatic massage, therapeutic ultrasound, explaining the patient about the prolonged nature of symptoms, and offering reassurance.
Clinical Significance
While the face defines a person's identity, nevertheless, an attractive face promotes self-esteem, trust, approachability, and success. Autologous fat grafting for facial rejuvenation represents a powerful tool in the plastic surgeon's armamentarium when creating a youthful and attractive appearance of the face. In addition to its volumizing effects and skin benefits, autologous facial fat grafting remains an ideal filler choice for facial rejuvenation due to its longevity, cost-effectiveness, biocompatibility, risk profile, and satisfaction rates compared to other dermal fillers.[18][19][20]
Enhancing Healthcare Team Outcomes
The procedures include the evaluation of recipient and donor areas, as well as fat harvesting, processing, and reinjection. Inappropriate treatment at any of the steps in this link may affect the final outcome. The surgery has certain unique requirements like cannula specific to the area of interest, disposal of unused fat and equipment for harvesting, processing, and transfer. These requirements need to be communicated by the surgeon to the operative team prior to the surgery. Any instructions about the need for additional personnel or expertise has to be conveyed beforehand. Nurses and other team personnel should be able to effectively communicate with the patient to inquire about the expectations for the surgery and the patient's understanding of the outcome and possible complications. Facial rejuvenation is often a delicate issue for the patient as it is associated with the identity of a person. Any misconceptions and queries of the patient have to be resolved beforehand.[21]
The imaging of the patient, if obtained, should be discussed with the radiologist in order to gain further insight into the facial anatomy of the patient. Such radio-conference sessions are especially necessary when operating on a case with a history of remote facial trauma or pathology. In the case where fat grafting is a part of complex surgery like facial reconstruction, collaboration with maxillofacial surgeon, orthopedic surgeon, orthodontic surgeon, and interventional radiologists may be necessary. Cases with comorbidities have to be given attention as they may have unintended consequences from the surgery. Patients with cardiovascular comorbidities may require cardiology consultation and, in certain cases, require to see a cardiac anesthesiologist. [Level 5]
Nursing, Allied Health, and Interprofessional Team Interventions
- The use of the compression garment of the patient is essential as the increased mobility of the fat graft may cause graft loss.
- It is extremely important to make sure the patient avoids deep massage to the area as that can actually shift the position of the graft.
- The area of fat transfer must not be treated with a hot compress. Although a cold compress is allowed, there is little evidence for its utility and should not be excessively performed.
- Warning signs of complications like blindness, fat embolism, infection, and keloid formation should be explained to the patient to allow for early intervention.
(Click Image to Enlarge)