Surgical Management of Femoral Neck Fractures
- Article Author:
- Zara Hayat
- Article Editor:
- Matthew Varacallo
- Updated:
- 6/28/2020 2:28:00 PM
- For CME on this topic:
- Surgical Management of Femoral Neck Fractures CME
- PubMed Link:
- Surgical Management of Femoral Neck Fractures
Introduction
Femoral neck fractures (FNFs) are extremely common.
FNFs demonstrate a bimodal distribution pattern, occurring secondary to low energy falls in elderly patients, and higher energy traumatic mechanisms in younger patients. This article reviews the key operative techniques and surgical management options for managing FNFs in the elderly and young populations.
Anatomy and Physiology
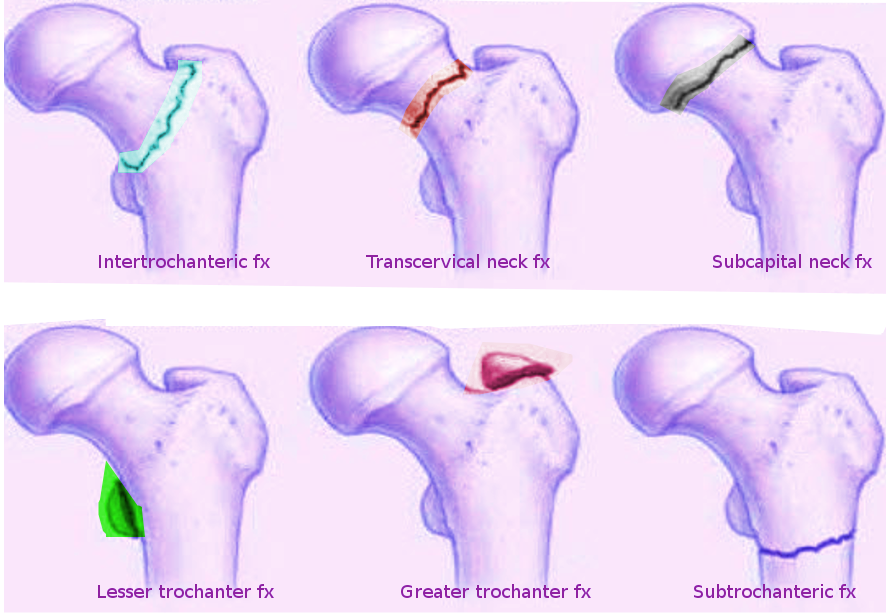
Intracapsular FNFs account for approximately 50% of all hip fractures. The majority of these fractures occur in elderly patients with underlying osteoporosis.[1][2][3][4]
FNFs are differentiated from extracapsular hip fracture patterns based on anatomic location. The distinction of these fracture patterns is critical because intracapsular fractures demonstrate limited healing potential secondary to the absence of the periosteal layer and the fracture is bathed in the surrounding synovial fluid. The hip joint capsule attaches to the intertrochanteric line anteriorly and the crest posteriorly.[5] There is a theoretical risk of compromised blood supply to the femoral head secondary to increased intra-articular pressures in the setting of an intracapsular FNF with preservation of the hip joint capsule. A tamponade effect that compromises femoral head perfusion has been demonstrated in previous studies.[6]
The arterial blood supply to the femoral head arises from three main sources:
- Profunda femoris artery
- Two major branches include the medial and lateral circumflex femoral arteries (MFCA, LFCA)
- The dominant contributing blood supply is from the MFCA by way of the lateral epiphyseal artery
- The LFCA supplies portions of the anterior and inferior femoral head
- Retinacular vessels branching from the circumflex arteries
- Two major branches include the medial and lateral circumflex femoral arteries (MFCA, LFCA)
- Ligamentum teres (predominant role in pediatric patients, minimal contribution in the adult patient)
- Minimal supply from the medullary canal and inferior gluteal artery
In addition to the tamponade effect as mentioned above and its potential compromise to femoral head blood flow, patients with FNFs are at risk of developing avascular necrosis (AVN) due to the retrograde blood supply and injury to the retinacular vessels.
Implications for Treatment
Displaced intracapsular FNFs in the elderly are typically managed with hip reconstruction procedures. The femoral head and neck are replaced with a reconstruction prosthesis. These procedures typically include hip hemiarthroplasty or total hip arthroplasty (THA) procedures. Nondisplaced fractures can be managed with fixation using cannulated screw fixation.
In contrast, extracapsular fractures rarely have a compromise to the arterial blood supply to the femoral head and neck, and thus, are commonly managed with various types of surgical fixation techniques.
Indications
General Concepts
The elderly population often presents with FNFs in the setting of multiple medical comorbidities. Thus, this patient population requires a comprehensive an interprofessional approach to address all comorbidities and all mental and physical impairments.[7]
Surgery is nearly always indicated for patients presenting with an FNF. The goals of surgery include:
- Pain control
- Restoration of mobility and function
- Achieve restoration of alignment and osseous healing (following surgical fixation techniques)
Nonoperative Management Considerations
In the setting of FNFs, nonoperative management is rarely indicated given the devastatingly highly-associated complication rates. Nonoperative management is reserved only for a select subgroup of nonambulatory patients with significant medical comorbidities.
Patients managed definitively with nonoperative treatment modalities are treated with pain control modalities. Patients often experience pain for several weeks indicating the formation of a functional girdle stone. The goal of care is always based on a delicate balance in weighing the overall risks and benefits of surgical versus nonoperative management. In select patients that are deemed critically ill and at significant risk for perioperative complications with surgical management, the phases of patient care include initial pain/symptomatic control followed by attempts at mobilization once some callous formation is noted after a few weeks.
The risks associated with nonoperative management include increased rates for associated complications, such as pulmonary dysfunction, pneumonia, urinary tract infections (UTIs), pressure sores (e.g, sacral decubitus ulcers), and venous thromboembolic events.
Indications for Specific Surgical Techniques
Hemiarthroplasty and THA
Replacement of the femoral head is indicated in displaced intracapsular FNFs, particularly in low-demand, elderly patients. In patients that present with these injuries in the setting of independent baseline ambulatory function, or in patients with prior evidence of hip pain and/or radiographic evidence of degenerative arthritis, a THA is recommended.
Cannulated Screws
Cannulated screw fixation is indicated in nondisplaced, intracapsular FNFs in elderly patients, and in displaced fractures in younger patients with ideal bone quality. The technique consists of inserting 3 or 4 cannulated screws in an inverted triangle or diamond configurations, respectively. While no difference in outcomes has been demonstrated comparing the utilization of three versus four screws, the literature notes superior results in surgical fixation configurations utilizing the inverted triangle placement compared to fractures fixed with only two cannulated screws.
Critical utilization of partially threaded (long or short thread options) screw options should be pre-operatively planned before the commencement of the procedure. The surgeon should plan on optimizing the "lag by design" technique.
Sliding Hip Screw (SHS)
The SHS fixation construct is comprised of a large, cancellous lag screw which passes from the lateral, proximal femur, across the fracture site and ending near the apex position of the femoral head. The lag screw dynamically slides inside an incorporated metal sleeve, with the latter being connected to a fixation plate that subsequently is secured with multiple screws to the proximal femur. The compression mechanism is amenable for utilization for the following types of injuries:
- Stable, intertrochanteric hip fractures
- Basicervical fracture patterns
- Vertical FNF patterns
- SHS fixation is superior to cannulated screw fixation in younger patients with vertical fracture patterns
The fracture is amenable to compression as the transfer of weight-bearing forces propagate from the appendicular skeleton, through the pelvis, and through the femoral head and neck before the forces transmit distally. Thus, the SHS fixation construct allows for longitudinal sliding and compression as the patient ambulates postoperatively. Thus, the fracture compresses down as the lag screw slides into the barrel and further promotes healing.
Intramedullary Nail (IMN)
Similar to the SHS in that one or multiple screw fixation elements extends from the lateral, proximal femur through the neck and ending near the apex of the femoral head. Depending on the specific implant type, there are options to promote varying degrees of dynamic compression versus fixed angle constructs that can be tailored to the specific type of fracture pattern.
Key differences in the indications for IMN versus SHS construct utilization includes a shorter lever arm generated by using the IMN constructs which are often favored in the setting of comminuted IT or subtrochanteric fracture patterns. Fractures involving the lateral wall of the proximal femur are, by definition, either reverse obliquity or transtrochanteric fracture patterns. These fracture patterns preclude the use of an SHS fixation device.[8]
Other potential benefits of IMN over SHS includes the possible use of a smaller incision (assuming an open incision is not required to achieve acceptable reduction of the fracture), and the maintenance of hip offset and lever arm as the IMN fixation results in a reduced sliding distance compared to the SHS.[9]
Cost comparison studies are controversial. A 2008 Level III study reported the overall adjusted cost estimates associated with the Diagnostic Related Group (DRG) categories and RVU compensation facet elements. Medicare beneficiary data was obtained for over 40,000 patients from 1999 through 2001. The authors reported, on average, $947 higher for the IMN-treated group compared to their SHS counterparts and attributed the increased costs to higher physician RVUs, a longer average length of stay (LOS), and a higher rate of revision surgery.[10]
Contraindications
SHS fixation constructs are contraindicated in the following (unstable) fracture patterns:
- Reverse obliquity
- Transtrochanteric
- Comminuted fracture patterns with a large posteromedial fragment; implies a loss of the medial calcar buttress
- Fracture patterns with subtrochanteric extension
Equipment
All require a standard orthopedic tray/set and should be carried out in an operating theatre equipped with laminar flow.
DHS/Cannulated Screws/IM Nails
Both require the necessary implants, a radiolucent traction table or a flat Jackson operating table, image intensifier, and radiographic technician
Hemiarthroplasty/THA
Standard operating table with necessary side supports, full set of implants, and, when applicable, the necessary instruments and materials allowing for incorporating cement fixation
Personnel
All operations require the following key personnel:
- Operating surgeon and assistant
- Anesthetist and ODP
- Scrub nurses
- Circulating staff
- Radiographer for SHS/cannulated screws/IM nail
Preparation
The patient should have had a full history and examination, as well as appropriate anteroposterior (AP) and lateral radiographs of the hip and pelvis. They should consent and be marked in preparation for surgery. These patients tend to be elderly with numerous co-morbidities. It is important that they are optimized pre-operatively. Healthcare profiders need to pay particular attention to whether these patients are on any anti-coagulants which may require reversal with Vitamin K and fresh frozen plasma (FFP in the case of warfarin). Available reversal agents vary by country and geographic region. Other possible reversal agents include:
- Four-factor prothrombin complex concentrate (PCC)
Routine pre-operative labs should be checked, including a complete blood count (CBC), a basic metabolic panel (BMP), a type and screen/cross-match. Pre-operative medical service co-management may include additional consultation services depending on the degree and severity of pertinent medical comorbidities.
Other routine pre-operative workup elements include:
- Chest radiograph
- Electrocardiogram (ECG)
Diabetic patients and patients present with a history of chronic obstructive pulmonary disease (COPD), cardiovascular disease, congestive heart failure (CHF), end-stage renal disease (ESRD).
Patients should undergo review by the anesthetist and consideration for spinal versus general anesthetic.
Once in theatre, WHO checklist should be completed, the patient positioned as detailed below, and appropriately prepped and draped.
Sliding Hip Screw/Cannulated Screws
The patient is placed supine on a radiolucent traction table. The foot on the side to be operated on is in a traction boot. The unaffected side is placed in the lithotomy position strapped in a leg holder and placed in a flexed, abducted, and externally rotated position to ensure the radiographic c-arm can access the fracture site appropriately. Gentle traction and internal rotation should be applied to reduce the fracture. Slight abduction may be needed to reduce any varus malalignment. Before prepping and draping, the fracture should be in near-anatomic alignment with radiographic confirmation. If closed reduction is not possible the open reduction may be necessary.
Correct lower extremity rotational alignment is imperative, and the patient should be positioned with the patella facing toward the ceiling.
Intramedullary Nail (IMN)
The positioning is the same as for DHS/cannulated screws, but it is important that the hip is in an adducted position. To achieve this, the torso can be pushed 10 to 15 degrees to the contralateral side. The reduction is as above with traction and internal rotation with the image intensifier. Care should be taken not to rotate the pelvis when applying traction.
Hemiarthroplasty/THA
The patient is positioned in a lateral decubitus position with supports over the anterior superior iliac spine and the sacrum. The pelvis should be at 90 degrees to the table. It is important to review the pre-operative radiographs and assess offset. This is the distance between the center of the femoral head and a line drawn down the middle of the femur. The femoral head size should also be checked and should match the patient's own as closely as possible.
Technique
SHS
Incision: A direct lateral approach is performed. The incision usually starts in line with the lesser trochanter, in line with the femur and extends distally. Next, a longitudinal incision through subcutaneous fat. The next layer is the fascia lata. This is incised in line with the skin incision to reveal vastus lateralis. The epimysium is incised. Vastus lateralis can be elevated off the lateral intermuscular septum but is more commonly split along its fibers.
Exposure of femur: A periosteal elevator (Bristow) is used to clear muscle from the bone, leaving a clear surface for the plate without soft tissue interposition. One or two self-retaining retractors may be helpful to gain adequate exposure for guidewire placement.
Guidewire: The kit typically includes a guidewire jig which is placed on the femoral shaft. It is important to make sure that the jig is placed centrally on the lateral shaft of the femur and can be checked by feeling how much bone there is anteriorly and posteriorly and adjusted accordingly. Regarding AP placement of the wire, it is necessary to visualize where the tip of the guidewire will end up in the femoral head. The lesser trochanter usually marks the level of entry for a 135-degree angle plate. The tip should be within the subchondral bone. The position should be continually assessed using image intensifier.
Measure: The included measuring device slides over the guidewire. It is important to ensure that it is sitting on the bone. Usually, 5 to 10 mm are deducted from the measurement.
Reaming: The guide wire is then over-drilled with a triple reamer. This creates a channel for both the lag screw and the barrel of the plate. Reaming is to the depth chosen for the screw. It is important to check on the radiograph that the third part of the reamer has engaged with the cortex of the bone and to ensure that the guide wire is not advancing into the pelvis.
Tap: In young patients or those with strong bone, it is beneficial to tap the bone.
Insert lag screw: The lag screw is then applied over the wire and screwed in using the handle attached. The final position of the handle should be parallel to the femur. This ensures the lag screw will slot into the plating barrel.
Apply plate and screws: The plate is then slid over the lag screw. The plate temper may be needed to ensure it is fully advanced. The guidewire can now be removed. The plate can be secured to the femur using a clamp. The screws are inserted next. The most distal one is conventionally done first. The 3.5-mm drill is used with the neutral drill guide to make the screw holes, drilling through both cortices. These are then measured using the depth gauge and the appropriate screw inserted.
Closure: Final AP and lateral radiographs should be obtained. The wound is washed and closure is in layers.
Cannulated Screws
Reduction: Reduction is usually not needed for these as screws are typically used for non displaced fractures.
Incision: Similar to the DHS, a direct lateral approach is taken with a longitudinal incision made at the level of the lesser trochanter. This, however, is much smaller, usually around 5 cm.
Guidewire: The next step is to insert the three guidewires. This can be done using a guide or freehand depending on surgeon preference and experience. The typical formation is an inverted triangle with one screw distally and two proximally. The entry point for the first guidewire should be no lower than the lesser trochanter, otherwise, there is the risk of causing a stress riser which may trigger a comminuted subtrochanteric fracture. Ideally, it should sit just above the calcar (on the AP view) and go up to subchondral bone in the femoral head. The second guidewire is placed superiorly and posteriorly to the first one. On the lateral view, it should lie next to the posterior cortex. The third wire is placed superiorly and anteriorly to the first wire. Ideally, it should sit parallel to the second guidewire on the AP view. All three should be within 5 mm of the subchondral bone.
Measure and screw insertion: The measure is then used to ascertain which screw length is to be used. Next, a cannulated drill is used to ream over the guidewires. This is usually from 5 to 10-mm short of the measured distance. Three partially threaded screws are then inserted before a wire driver is used to remove the guide wires. The screw measurement is usually the same as the original measurement of the guidewire. The threads of the screw should be beyond the fracture site to ensure that adequate compression takes place. The screws should be tightened together so as to ensure uniform compression. Depending on surgeon preference, washers may be used to further increase compression.
Closure: Final AP and lateral images should be taken and the wound washed with normal saline. It should then be closed in layers.
Hemiarthroplasty
Approach: There are numerous approaches to this operation.[13] One common approach is the anterolateral approach, also known as the modified Hardinge approach. A longitudinal incision centered over the greater trochanter is made. This is usually around 20-cm in length, curving posteriorly proximally. The layers encountered are subcutaneous fat, fascia lata, bursa and then gluteus medius. The fascia lata is incised in line with the femur, following the line of the original incision, curving posteriorly. This is usually with a small incision centrally with a scalpel and then, using scissors, the fascia lata is cut distally and then proximally. The fascia is then retracted using either a couple of self retainers or a Charnley retractor. If the latter is used, the D shape created should point towards the knee. The trochanteric bursa is excised using forceps and scissors. Following which the greater trochanter and attached muscles should be clearly visible, with gluteus medius proximally and vastus lateralis distally.
The assistant should then externally rotate the leg to put gluteus medius on the stretch. The tip of the greater trochanter should be identified and the gluteus medius fibers split. Be aware that the superior gluteal nerve is approximately 5-cm proximal to the tip of the greater trochanter.
The abductors (gluteus medius superficially and gluteus minimus underneath)are then detached from the greater trochanter using diathermy. This is typically done in an "s" or "omega" shape, leaving a sufficient cuff for repair at the end. It is sometimes necessary to split some of the vastus lateralis fibers as well.
Adequate dissection should reveal the capsule. A T-shaped incision is made in the capsule, staying close to the bone at the base of the femoral neck.
Dislocate hip: It is then necessary to dislocate the hip by externally rotating it. This should reveal the fractured neck as the leg is placed into the leg bag to enhance exposure.
Neck osteotomy: The next step is to make the neck cut. This is done with an oscillating saw at a 45-degree angle. The neck cut is typically measured from a line running between the superior aspect of the neck to 1cm proximal to the lesser trochanter but depends on the prosthesis to be used; particularly whether it has a collar or not.
Femoral head removal: This is done using the corkscrew which is placed centrally in the head and then twisted in. The head is spun to detach it from the acetabulum and then can be removed. It may be necessary to use a mallet to help engage the corkscrew with the bone. If it is difficult to remove the femoral head, check the capsule cut is sufficient.
Femoral head measurement: This is done using the guide. If between sizes, most surgeons advise erring on the smaller side to minimize the risk of dislocation.
Prepare acetabulum : Ensure all soft tissue is removed; a bone nibbler can be used to remove any remaining soft tissue.
Femoral canal preparation: A Hohmann retractor is then used to expose the femoral calcar. The femur is prepared using a box chisel. This is typically placed as posterolaterally as possible and opens the femoral canal. A T-handled reamer is then inserted into the canal. While doing this, it can be helpful to place your other hand on the patient's knee to ensure it follows the anatomical axis. Reamers of increasing size are used until rotational movement is resisted. The femoral canal is then rasped. Particular attention is given to rasping the lateral side.
Trial: Trial the head and reduce the hip to assess size and stability with internal and external rotation with the hip flexed and extended. Assess for equal leg length. This is not always performed due to its intrinsic stability. If the hip is difficult to reduce, it may be because the stem is too proud, the offset is too great, or there is soft tissue obstruction. Dislocate the trial.
Cementing: Insert a cement restrictor (this may need to be sized depending on kit used; typically 2 cm more than the length of the stem. The femoral canal is then washed using copious pulse lavage. Ribbon gauze is then inserted into the femoral canal alongside a clean suction catheter. This will ensure the canal is dry and free from fat and blood to allow the cement to interdigitate with the bone for solid fixation. At this point, the cement is prepared. The gauze is removed and the cement is inserted into the canal using the cement gun. The nozzle should be inserted fully into the canal and by allowing the pressure of the cement to push the gun up proximally. Surgeon preference dictates whether the cement is pressurized.
Stem insertion and head attachment: The selected femoral stem is then inserted into the femoral canal. Be sure to remove all excess cement. It should ideally have 10 to 15 degrees of anteversion. Once the stem is in situ at the appropriate depth, avoid altering the degree of anteversion as this can result in a varus stem which will compromise outcome. The femoral head is then attached to the trunion and the hip reduced. This is done with gentle traction and a small degree of internal rotation. Stability should be assessed.
Closure: The wound is then washed and closed in layers (capsule, the abductors can be closed en masse, fascia lata, fat, skin). A double-layered closure of interrupted and then continuous sutures of the abductors may be of benefit to ensure a secure repair.
IM nail
Incision: A small (3 to 5 cm) lateral longitudinal incision is made proximal to the tip of the greater trochanter. This should be in line with the femoral shaft.
Entry point and guidewire: The entry point for the guidewire depends on the nail. Most use the tip of the trochanter (cephalomedullary nails) or the piriformis fossa (straight nails) as landmarks. Guidewire position should be checked using image intensifier; ideal position is central within the shaft on the AP view and in line with the middle of the femoral neck in the lateral view. It is important to avoid a too lateral entry point as this will cause varus malalignment which will predispose the implant to early failure.
Ream: Usually a protection sleeve goes over the guidewire, which should sit flush with the greater trochanter. The femur should be renamed; it is suggested that this is done by hand in elderly patients with osteoporotic bone but can be done on power in younger patients.
Nail insertion: The nail is typically attached to a jig and is inserted manually over the wire. The depth of the nail as its inserted should be checked on image intensifier. It is important that the lag screw should sit in the middle of the femoral neck with the tip in the center of the femoral head on AP and lateral views.
Lag screw guidewire: The guidewire is mounted on the jig. A small skin incision is then made. The drill sleeve should sit on the lateral cortex of the femur. The positioning of the screw is similar to that of the DHS; in line with the neck of the femur in the AP view with a slightly inferior position and centrally placed in the lateral view. It should go up to the subchondral bone. The tip apex distance should be less than 25 mm. The guidewire is then measured. The final measurement should be 5 to 10 mm less. The lateral cortex is then reamed. It is then locked using the jig.
Distal locking screw: Depending on the jig and whether it is a long or short nail, the distal locking screws may need to be done freehand using the 'perfect circles' technique. For short nails, it is usually possible to use the selected hole on the jig. A stab incision is made in the skin and both cortices are drilled using the drill bit and the protective sleeve. It is then measured and a screw inserted.
Closure: Final AP and lateral images are checked and the wounds washed. The closure is often surgeon-specific and can consist of multiple different suture options. The decision to repair the capsule and/or other periarticular tendinous structures is surgeon-dependent based on the preferred technique and the approach utilized. In general, strong suture options can be used in an interrupted or running-style closure. Once the deep layers are closed, 2-0 synthetic absorbable sterile surgical suture composed of a copolymer can be used in an interrupted and buried stitch technique. Finally, the skin is closed utilizing staples, nylon, or running synthetic, absorbable suture. Augmentation skin closure options include various types of skin glue or steri-strips. A sterile bandage is then applied.
Postoperative Plan
- Routine labs including complete blodd count (CBC) and BMP are checked at various intervals following surgery and the frequency will depend on the patient's overall condition and
- Formal radiographs depending on surgeon preference (essential post hemiarthroplasty to ensure the joint is reduced and in an ideal position
- Postoperative antibiotics as per hospital protocol
- Venous thromboembolism prophylaxis as per hospital protocol
- Mobilize full weight bearing as pain allows with physiotherapists (partial or touch weight bearing for cannulated screws and for comminuted fractures managed with an IM Nail)
- Follow up depending on surgeon preference
Complications
General Surgical Risks
- Infection (antibiotics are usually given at induction with two postoperative doses)
- Bleeding
- Neurovascular injury
- DVT/PE
- Anesthetic risks
- MI/Stroke/Death
Specific Risks
Infection
Sepsis can occur in up to 20% of cases and can result from superficial or deep infection. HEalthcare professionals believe the presence of hematoma increases this risk.[14]
Fixation Failure
This is more likely to occur in patients with pathological bone, for example as a result of rheumatoid arthritis or osteoporosis. It can occur as a result of technical errors while operating. Loosening or dislocation can occur following a hemiarthroplasty.
Fracture
It is estimated that there is a 4.5% risk of fracture in hemiarthroplasty procedures. They are most likely to occur on reduction of the hip and commonly affect the neck or greater trochanter.
VTE/DVT/Blood clots
Fat Embolism
As discussed, this is a potential complication of pressurizing cemented stems and nailing. Hypoxia may be noted during pressurization or on the reduction of the hip. The risk can be minimized by adequate lavage and drying of the femoral canal.
Leg Length Discrepancy
This can occur with any of the procedures. A small difference can usually be managed with a shoe lift if problematic.
Non-Union (DHS/IM nail)
Patients may re-present with groin or buttock pain approximately 12 months following fixation. Pain is worse on hip extension or with weight bearing. It is thought to affect up to 25% of displaced fractures and 5% of undisplaced fractures. Management is either with total hip replacement in the elderly or consideration for proximal femoral osteotomy in the young.
Dislocation
This is a specific complication of hemiarthroplasty. In general, THA for the treatment of FNF demonstrates a higher relative postoperative dislocation rate compared to the patients undergoing an elective, primary THA procedure.
Avascular Necrosis
This can occur in up to 10% of undisplaced fractures and 30% to 45% of displaced fractures. Patients typically present with groin pain; there may be signs of sclerosis on radiographs. Management typically involves conversion to a total hip replacement, but alternatives such as osteotomy or core decompression may be considered in younger patients.
Malunion or Nonunion
There is an incidence of 5% to 30%. Varus malreduction following cannulated screw fixation correlates with fixation failure.
Fixation Failure Rates
- High early failure rates in the surgical fixation groups
- Rates stabilize by 2 years postoperative
- Two-year follow-up (elderly population older than 70 years) with displaced femoral neck fractures
- Forty-six percent following surgical fixation versus 8% following reconstruction techniques (THA or hemiarthroplasty)
- Two- to 10-year follow-up
- Failure rate approximately 2% to 4%, respectively
- Overall failure rates still higher in arthroplasty at 10-year follow-up
Death
Mortality is approximately 30% in the elderly in the first year following a fractured neck of the femur.
Clinical Significance
These are commonly performed procedures, and it is important to understand and recognize that different fracture types and patient groups are better suited to the specific type of fixation/arthroplasty. There are some areas of debate on the finer points of the surgery, and these will be briefly considered.
Bipolar versus Unipolar Hemiarthroplasty[15]
There is debate over the use of bipolar or unipolar implants. In bipolar implants, the femoral head is surrounded by a polyethylene liner within an acetabular shell within which it can move. Although a more expensive implant, studies suggest it confers benefits of reduced pain, less acetabular wear and lower dislocation rates. It is also easier to convert to a total hip replacement should that be indicated in the future. Unipolar implants are simpler and less expensive. There is some evidence to suggest that over time the bipolar implant also loses movement at the inner bearing and eventually resembles a unipolar implant.
Cemented versus Uncemented Hemiarthroplasty[16]
Cemented implants give better functional and mobility related outcomes. It also confers greater stability but does carry an increased risk of fat embolism which can cause hypoxemia. Despite this, research suggests that cemented stems carry a higher overall survival rate. The cement acts as a grout, creating an interface to distribute load between the smooth surface of the femoral stem and the irregularities of the bone surface.
Uncemented implants carry a higher risk of periprosthetic fracture post and intra-operatively.[17] Stability is conferred from impaction of the uncemented stem in the cancellous bone but if the bone quality is poor, then impaction will be impaired and stability reduced.
SHS Lag Screw Positioning
Tip apex distance is the sum of the distance from the tip of the screw to the apex of the femoral head on the AP views and the lateral views. Baumgaertner et al.[18] found that a tip apex distance of less than 20mm resulted in no occurrences of screw cut out. The aim is for a tip apex distance of less than 25 mm to minimize the risk of failure. On AP views the law screw should be slightly inferior, and slightly posterior on the lateral view. Eccentric placement is likely to cause a rotational failure of the construct.[19] The anterosuperior region is where bone quality is poorest.
Enhancing Healthcare Team Outcomes
Medical optimization of these patients pre-operatively and management of their medical co-morbidities postoperatively is vital for a good outcome, and this could not be achieved without input from the orthogeriatric/medical teams. Physiotherapists and occupational therapists are also vital to safely mobilize these patients and ensure a safe discharge from the hospital. With proper physical therapy, most patients can regain function and muscle strength, but failure to comply with physical therapy can lead to disuse and numerous other complications. These patients must be continually followed by the primary care provider and nurse practitioner to ensure that they are ambulating without pain and not developing post-surgical complications. (Level I to III or IV)