Fasciocutaneous Flaps
- Article Author:
- Jorge Boretto
- Article Editor:
- Franco De Cicco
- Updated:
- 8/20/2020 3:58:58 PM
- For CME on this topic:
- Fasciocutaneous Flaps CME
- PubMed Link:
- Fasciocutaneous Flaps
Introduction
Fasciocutaneous flaps originally called an axial flap, are tissue flaps that include skin, subcutaneous tissue, and deep fascia.
Including the underlying fascia with its prefascial and subfacial vascular plexus improves the vascularization of fasciocutaneous flaps. Also allowing us to have a greater length-to-width ratio compared with skin flaps.[1][2]
History of Fasciocutaneous Flaps:Pontén was the first to define the concept of a fasciocutaneous flap in the leg in 1981.[2] After that, fasciocutaneous flaps gained popularity as a reliable technique to cover bone and tendon in the lower leg and elsewhere. Pontén showed the importance of the deep fascia in the survival of a flap in the leg, but without demonstrating the kind of vascularization. Previously, skin flaps were based on the concept of random flaps with a limited length to width ratio (usually 1/1 of the lower limb). According to Pontén, the average ratio of fasciocutaneous flaps is from 2/1 to 3/1.[1] More than that may result in skin necrosis. In the years that followed, many authors detailed the clinical applications and the physiological bases of these flaps.
At that time, the advantages of the fasciocutaneous flaps had several aesthetic and functional advantages over both myocutaneous and muscle flaps. Haertsch and Barclay et al. established the anatomical bases when describing that the fact of including the fascia allows respecting the longitudinal anastomotic vascular networks, especially the suprafascial plexus, which is the most developed.[3][4] Acland et al. described in 1981 the saphenous flap on the medial aspect of the knee and applied it as a free flap.[5] Later on, Cormack and Lamberty classified the fascio-cutaneous flaps according to their patterns of vascularization.[6] The development of microsurgical techniques and perforating flaps was carried out at the expense of pedicle fasciocutaneous flaps, which still retain specific indications due to their ease and speed of execution.
Anatomy and Physiology
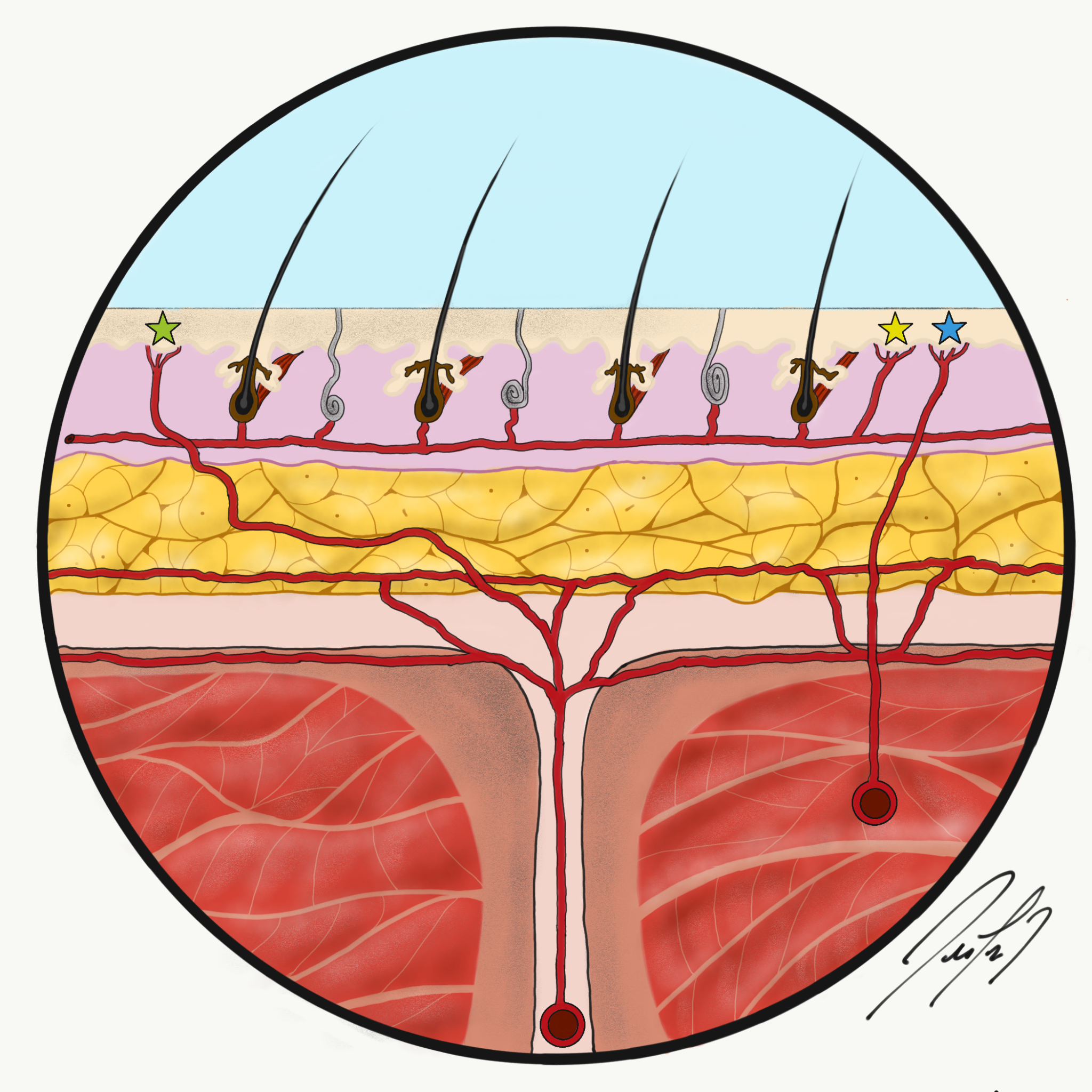
The anatomical basis of the fasciocutaneous flap is based on the fasciocutaneous perforators which reach the skin to supply it. At the level of the fascia, there are prefascial and subfascial plexuses and, more superficially, the subdermal and subcutaneous plexuses. These plexuses are supplied by arteries that enter the deep fascia through an underlying muscle (musculocutaneous perforators), through the septum between muscles (septocutaneous branches), or a direct cutaneous branch (Figure 1), between the subfascial and suprafascial plexus, the later one is the most developed. On the contrary, the vessels of the suprafascial plexus have a close relationship with the collagen fibers of the fascia. According to this, the dissection of the subfascial plane to the muscle is more accessible than a dissection of the suprafascial plane.[7][8]
The fasciocutaneous system is not homogeny, but it varies according to the anatomical area of the body. Anatomical research by Cormack and Lamberty, as well as the clinical application of Pontén and Tolhurst et al., have demonstrated that the septocutaneous vessels have a central role in the suprafascial plexus at the level of the extremities, while at the level of the trunk the musculocutaneous perforators are the main source.[6][2][9]
Classifications
Cormack and Lamberty have classified fasciocutaneous flaps into four types based on vascular anatomy.[6]
Type A: Multiple fasciocutaneous perforators entering at the base of the flap supplied the flap. The flap can be placed proximally or distally.
Type B: A single fasciocutaneous perforator supplied the flap. This flap may be isolated as an island flap or used as a free flap.
Type C: Multiple small perforators from the main artery reach the skin through a fascial septum. The main artery is included with the flap. It can be based proximally, distally, or as a free flap.
Type D: A compound flap, similar to type C but including a portion of adjacent muscle and bone.
Indications
The harvesting of fasciocutaneous flaps is quick and easy with enough practice. The indications are based on its advantages.
These flaps are reliable, thin, and easily mobilized, coming from many potential donor sites. Most of them preserve the main arterial axis. Unlike muscle flaps, the functional sequelae of the donor site are minimal. Although the fasciocutaneous flaps were considered to be not as resistant to infection as muscle flaps because fat and fascia are less vascularized than muscle, several studies concluded that fasciocutaneous flaps offer a comparable efficacy to the muscle flaps for infection treatment.[10][11][12] Moreover, fasciocutaneous flaps enable revision for orthopedic procedures and limit the need for secondary skin grafting. Fasciocutaneous flaps are preferred in reconstructing areas in which the skin or mucosa at the wound is thin; for example, the lower leg, dorsum of the hand, nasal lining, and oropharynx. Similar to muscle flaps, fasciocutaneous flaps provide large blocks of tissue for defect reconstruction without the need for the prior delay but are limited by the arc of rotation of the vascular pedicle, unless transferred as a free flap. They are not recommended in case of a deep cavity where muscle flap has an indication.
Fasciocutaneous flaps can be harvested in four different variants according to the tissue included:
- Peninsular Fasciocutaneous Flap: The adipofascialcutaneous unit is harvested, leaving the base of the flap as a hinge where it will be rotated. The peninsular flap is utilized as a rotation flap, and its possibilities of coverage are limited. Moreover, rotation at its base produces bulkiness or a dog-hear deformity, which sometimes need a secondary procedure to correct it.
- Island Fasciocutaneous Flap with an Adipofascial Pedicle: This variant is characterized by a vascular pedicle whose length confers to the flap, an arc of rotation that defines its possibilities. The fasciocutaneous unit is harvested according to the size of the defect to be covered. The pedicle is formed by an adipofascial strip or by an identifiable vascular pedicle.
- Adipofascial Flap: This variant includes the fascial plane along with a hypodermic layer.
- Fascial Flap: Its main indication is related to coverage of tendons to provide a gliding surface.
Fasciocutaneous Flap of the Legs
The leg was the first region in which the fasciocutaneous flap proved of great value. Several fasciocutaneous flaps have been applied to reconstruct a coverage deficit of the leg. However, preoperative planning is crucial since the stiffness of the fascia can difficult the insetting of the flap on the defect.
Flaps can be harvested at the posterior, lateral, or medial aspect of the leg and designed as proximally or distally based according to the point of the pivot, in the case of distally based flaps, a higher risk of venous congestion exits. This latter complication can be overcome by making anastomosis of the superficial vein of the flap to a superficial vein in the recipient site.[13]
Vascularization
Cutaneous and neurocutaneous branches are few in numbers. At the posterior aspect of the leg, in the midline, the sural artery after been in the suprafascial plane vascularized the skin. Musculocutaneous perforants are more numerous at the proximal third of the leg, going through the medial and lateral gastrocnemius muscles.
On the other hand, septocutaneous arteries are found mainly in the middle and distal third of the leg. They come from one of the three main arterial axes of the leg (anterior or posterior tibial artery and peroneal artery).
The venous return goes directly for the accompanying veins of the arterial supply.
Fasciocutaneous Flaps Proximally Based
The base of the flap should provide enough blood flow to allow to survive the flap. The base of the flap is not designed according to a length/width ratio; instead is designed to a defined pedicle. Based on this, the pedicle can be narrowed at the base until a true island flap can be harvested.
- Saphenous Flap
Acland et al.[5] described saphenous flap; this flap is based on the saphenous artery, which pierces the aponeurosis roof of the adductor canal within 2 cm of its origin and then runs down between the sartorius and vastus medialis muscles and the adductor tendon for a distance of 12 to 15 cm. It then gives off one to four important cutaneous branches to supply a large area of skin medially above the knee. The terminal (distal) saphenous artery passes between the sartorius and gracilis tendons and is distributed to the skin of the upper and medial portions of the leg below the knee.
The flap dimensions can achieve 8 to 10 cm in width and 30 cm in length (10 cm above and 20 cm below the knee). The proximal third of the tibia can be covered with the distal part of the flap. However, in case of knee deficit coverage, the flap has to be harvested more proximally, and the sartorius has to be divided between raising the flap.
- Medial fasciocutaneous Flap
The flap is nourished by the musculocutaneous perforators of the head of the medial gastrocnemius. The anterior border of the flap is a line posterior to the medial edge of the tibia; the distal limit should not extend from a line that is located 5 cm proximal to the medial malleolus and posteriorly the flap should be designed at the posteromedial line.
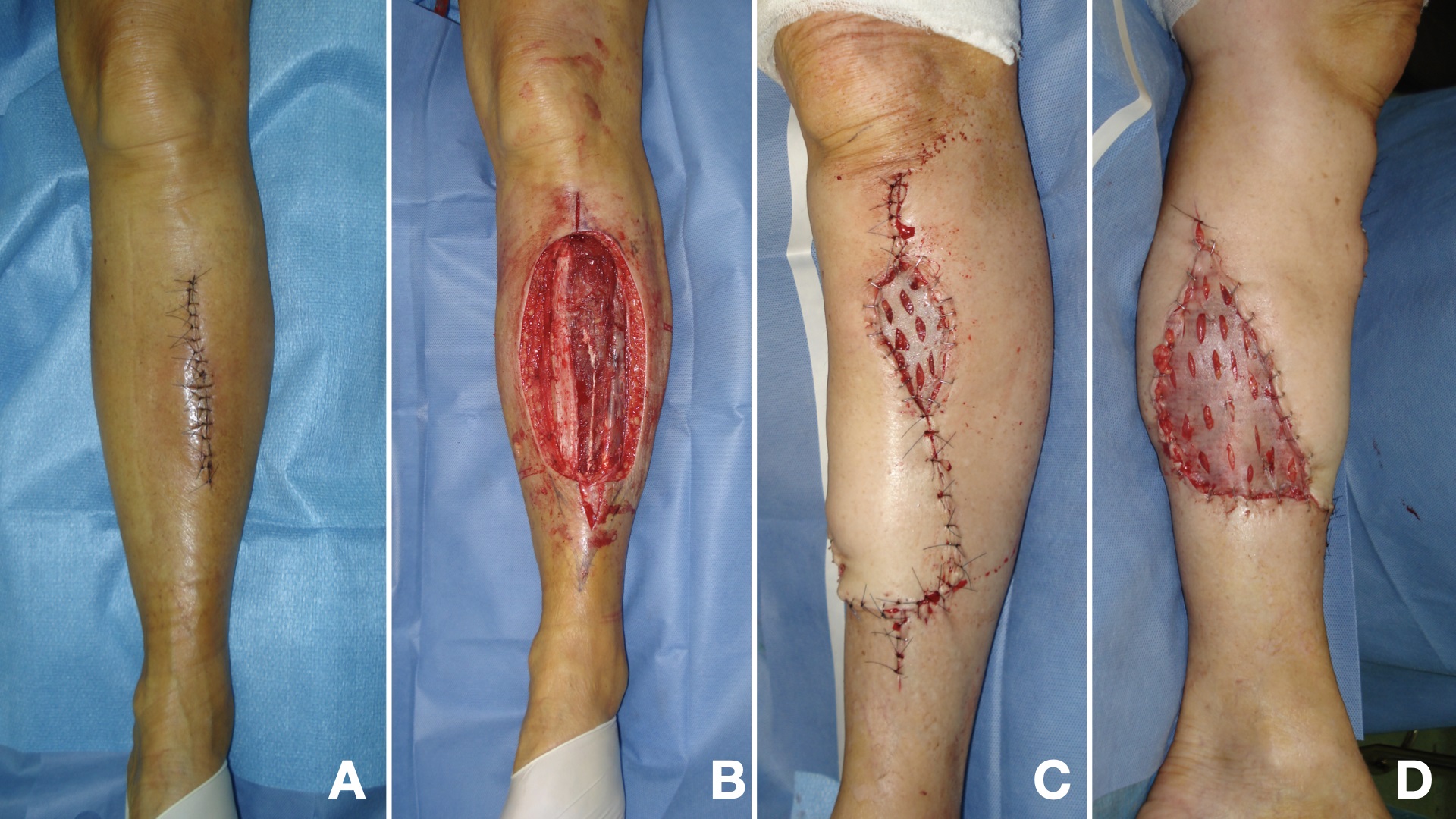
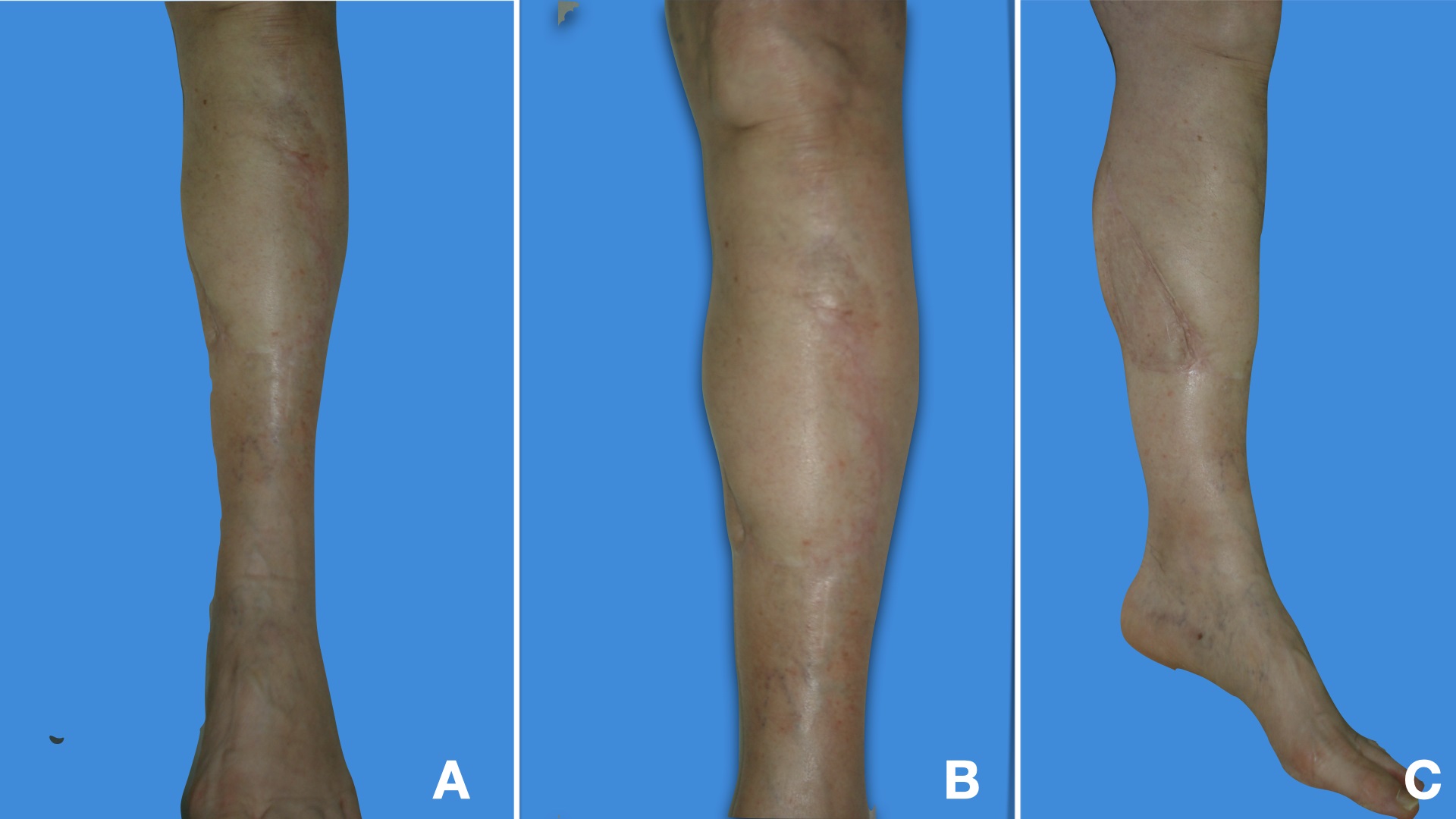
The flap is useful to cover the anterior aspect of the knee, and the proximal and middle third of the leg (Figure 2, 3).
- Lateral Fasciocutaneous Flap
As its medial counterpart, the lateral flap is nourished by the musculocutaneous perforators of the head of the lateral gastrocnemius. The anterior limit of the flap is 2 cm posterior to the posterior edge of the fibula, the posterior limit is the medial line, and the distal limit should not exceed the 10 cm proximal to the lateral malleolus tip.
- Anterolateral Fasciocutaneous Flap
This flap is nourished by the musculocutaneous perforators of the tibial anterior and peroneal arteries. It should be designed with an anterior limit 2 cm posterior to the tibial crest, the posterior limit is posterior to the fibula, and the distal limit is located 5 cm proximal to the tip of the lateral malleolus.
- Posterior Fasciocutaneous Flap
Described by Walton and Bunkis as a new cutaneous free flap, the blood supply to the skin of the posterior leg is derived from two sources: 1) perforating arteries that arise from the popliteal and posterior tibial arteries and 2) axial arteries originating from the popliteal, sural, and geniculate arteries that course either above or below the deep fascia.[14] The flap can be raised from the popliteal fold proximally until the union between the middle and distal third of the leg distally, and the medial-lateral limits could reach the axial medial or lateral midline.
Fasciocutaneous Flaps Distally Based
This kind of flap is vascularized by the septocutanous perforators located at the medial and lateral borders of the Aquiles tendon. These perforators come from the posterior tibial and the peroneal arteries.
The flap can be raised from the popliteal fossa proximally, and distally based can be designed in three different ways: 1) based on the perforators of the posterior tibial artery leaving 3 to 4 cm width base. The distal dissection should not exceed the 10 cm proximal to the tip of the malleolus medial. 2) based on the perforators of the perineal artery, with a pedicle of 3-4 cm width base. The distal limit of the dissection should not exceed beyond the 13 cm proximal to the tip of the lateral malleolus. Finally, it could be raised 3) based on both pedicles for which it should have a broad base to include them.
- Sural Fasciocutaneous Flap
This is a variant of the distally based fasciocutaneous flaps. This flap is based on the vascularization provided by the artery that runs along with the sural nerve.
Contraindications
Smoking has a considerable negative repercussion on the microcirculation.[15] It is considered a relative contraindication to this procedure. If smoking cessation cannot be obtained, a better vascular flap (muscle flap) should be considered. In all cases, patients must be informed of the risks involved.
In the case of diabetes or poor vascular status, the risk of failure is also higher. Preoperative evaluation can also detect soft tissue lesions or insufficiency of vascularization: sequelae of previous trauma, scars, concomitant traumatic injuries, poor vascular state. A computed tomography angiography is useful in cases of major trauma and arterial disease, to explore the vessels supplying the fascia and to evaluate the recipient site of a possible free flap.
They may not be used in places where deep defects are found. In this case, bulky flaps as muscle flaps are preferred. Sometimes there are size limitations, and donor sites may require skin graft closure.
Equipment
No special surgical equipment is required for performing fasciocutaneous flaps. This procedure can be done with a standard, minor operations surgical set.
Equipment needed is as follows:
Preoperatively
- Alcohol solution or pad
- Surgical marker
- Local anesthesia
- Topical antiseptics, such as broad-spectrum chlorhexidine or povidone-iodine
- Surgical drape
Intraoperatively
- Scalpel (#15 blade)
- Forceps (with teeth)
- Shea scissors (or other dissecting scissors)
- Iris scissors, preferably serrated
- Gauze
- Electrocoagulation/electrocautery device
- Skin hooks
- Needle driver
- Normal saline (keep tissue clean and moist)
- Suture (absorbable and nonabsorbable)
Postoperatively
- Petrolatum
- Non-stick dressing material
- Gauze
- Surgical tape
Personnel
Plastic surgeons most commonly undertake the fasciocutaneous flap. Currently, with the advent of "orthoplastic" surgery, some orthopedic trauma surgeons can perform these flaps.[16]
The surgery can be performed by one provider with one surgical assistant, primarily to help manage intraoperative bleeding, cut suture, and place a postoperative dressing. A scrub nurse and a theatre runner are also essential members of the team.
Preparation
Patient Counseling:
Patient education before surgery is mandatory. Counseling about the procedure and postoperative complications related to vascular compromise are priorities to understand the commitment of the postoperative measures and indications to avoid them. Typical advice for infection and scar formation is necessary. Besides, patients should be educated upon wound care for the donor site and pedicle, to avoid smoking, follow-up appointments, goals of reconstruction, and expectations of the surgeon and patient. Informed consent is taken as in any other procedure.
Pre-Operative Preparation:
Design the flap according to the defect. Lenght of the flap should be higher to avoid tension or lack of coverage after insetting.
The surgical site is cleansed; a sterile field is created.
A tourniquet is tied on the arm or thigh when the flap is performed either in upper or lower extremity respectively, to provide a bloodless field for surgery.
Technique
The design of the flap depends on the location of the tissue defect and the donor site. It is necessary to anticipate the location of the pivot point and the required length of the flap pedicle. The flap surface should generally be larger than the tissue defect to avoid tension and necrosis of the distal end of the flap.
The incision is carried right through the skin, subcutaneous tissue, and fascia. The dissection of the subfascial plane to the muscle is more accessible than a dissection of the suprafascial planes, which should be protected to avoid damage of the perforating vessels running to the skin. It is not necessary to identify the perforating vessels to raise the flap. The retrograde dissection is done according to the length needed from the pedicle.[17]
The skin surrounding the defect is excised, and tile edges of the wound undermined. The fasciocutaneous flap is then rotated or placed into position, and the fascia is sutured beneath the undermined skin. Only a few tacking sutures are needed to keep the flap in place: fine sutures are used to coapt the skin edges. When rotating huge flaps, a "dog's ear" is unavoidable and should be left for correction later. The secondary defect can be covered immediately with a split skin graft. However, the surface is usually irregular, and it's preferable to wait for granulation tissue. The area is bandaged with moderate pressure, and if possible, the distal part of the flap is left open for inspection. If bleeding is troublesome continuous suction drainage can be used for 24 hours or more.[2]
Complications
Vascular complications, either arterial or venous, are complications related to the flaps surgery, and it should be minimized by a proper preoperative planning and a careful surgical technique. Any technical mistake in flap design, harvest, or insetting can yield to either partial or complete flap necrosis. Infections can also occur, either superficial or deep. Donor site morbidity related to aesthetics can be significant, especially with larger flaps.[18]
Clinical Significance
The fasciocutaneous flaps include the deep fascia and the perifascial vascular network, which improves their vascularization compared to skin flaps in specific anatomical regions, especially the legs. Raising of fasciocutaneous flaps is quick and straightforward. These flaps are reliable, thin, and readily mobilized. They are particularly beneficial in the case of resurfacing areas of cutaneous mobility and coverage of tissues such as tendons, bone, and joints. The development of microsurgical techniques and perforating flaps was done at the expense of pedicled fasciocutaneous flaps, which nevertheless keep indications given their simplicity of realization.
Enhancing Healthcare Team Outcomes
An interprofessional team of an operative provider and an assistant nurse should perform the surgery. Follow up with a provider and a nurse experienced in wound management should be done to identify and minimize possible complications.
(Click Image to Enlarge)
(Click Image to Enlarge)