Forced Expiratory Volume
- Article Author:
- Sharoon David
- Article Editor:
- Christopher Edwards
- Updated:
- 9/14/2020 1:27:02 PM
- For CME on this topic:
- Forced Expiratory Volume CME
- PubMed Link:
- Forced Expiratory Volume
Definition/Introduction
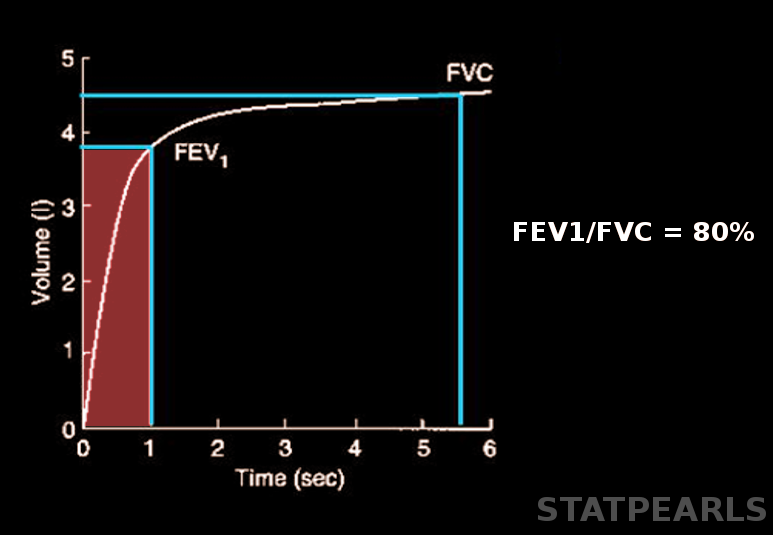
Forced expiratory volume (FEV) refers to the volume of air that an individual can exhale during a forced breath in t seconds.[1] Its usual representation as FEV, followed by a subscript that indicates the number of seconds of the measurement's duration. For instance, forced expiratory volume in 1 second (FEV1) is the maximum amount of air that the subject can forcibly expel during the first-second following maximal inhalation.[2] Similarly, forced expiratory volume in 6 seconds (FEV6) is the volume of forcibly exhaled air measured during 6 seconds.[3]
Issues of Concern
Spirometry is a test used to measure the ability of a person to inhale and exhale air respective to time. Forced expiratory volume (FEV) is one of the main results of spirometry.[1]
Age and gender are the major factors that affect the average values of FEV in healthy individuals. Height, weight, and ethnicity are some of the other influencing factors.[4][5] FEV values greater than 80% of the predicted average value are considered to be normal.[6] Other factors that can affect the results include decreased patient effort, poor inhalation, inability to follow directions, and some medical conditions prevent successful spirometry. A weak effort correlates with an overestimation of FEV1.[7]
Clinical Significance
Forced expiratory volume in the first second (FEV1) can be useful to categorize the severity of obstructive lung diseases, such as asthma and chronic obstructive pulmonary disease (COPD). Expressing FEV1 as a percentage of the predicted value in a patient is means by which to express this severity.[8][9][10]
FEV1 can also be helpful in the interpretation of the reversibility test, also known as the bronchodilator test. This test assesses the bronchodilator response in a patient with obstructive lung disease. It involves the administration of a bronchodilator, such as an anticholinergic agent or a short-acting beta-2 agonist. An increase in the FEV1 of greater than or equal to 12%, or greater than or equal to 200 mL, after bronchodilator use, is considered to be a positive bronchodilator response. A positive response typically presents in reversible airway obstruction, such as in asthma, whereas nonreversible obstruction, as seen in COPD, may not show a positive response to the administration of a bronchodilator.[8][10][11]
The ratio of FEV1 to FVC (FEV1/FVC, also known as FEV1%) can help distinguish obstructive and restrictive lung diseases. In obstructive diseases, FEV1 reduction is due to the increased airway resistance to expiratory flow. A reduction in the FVC may also present because of premature airway closure in expiration; however, it is not affected as much as FEV1 and, thus, is not decreased in the same proportion as FEV1, which can lead to a reduced value of FEV1/FVC, of less than 70%.[9] On the other hand, in restrictive lung diseases, such as chest wall deformities, and idiopathic pulmonary fibrosis, the FVC may be decreased more as compared to FEV1, thus giving an FEV1/FVC ratio of more than 70%.[12]
Forced expiratory volume in 6 seconds (FEV6) has been proposed as a valid alternative for forced vital capacity (FVC) in the diagnosis of airflow obstruction in elderly individuals.[3][13][14]