Physiology, Gag Reflex
- Article Author:
- Shruthi Sivakumar
- Article Editor:
- Aparna Prabhu
- Updated:
- 5/5/2020 10:24:20 AM
- For CME on this topic:
- Physiology, Gag Reflex CME
- PubMed Link:
- Physiology, Gag Reflex
Introduction
The gag reflex, also known as the pharyngeal reflex, is a reflex contraction of the muscles of the posterior pharynx after stimulation of the posterior pharyngeal wall, tonsillar area, or base of the tongue. The gag reflex is believed to be an evolutionary reflex that developed as a method to prevent the aspiration of solid food particles. It is an essential component of evaluating the medullary brainstem and plays a role in the declaration of brain death. [1]
Mechanism
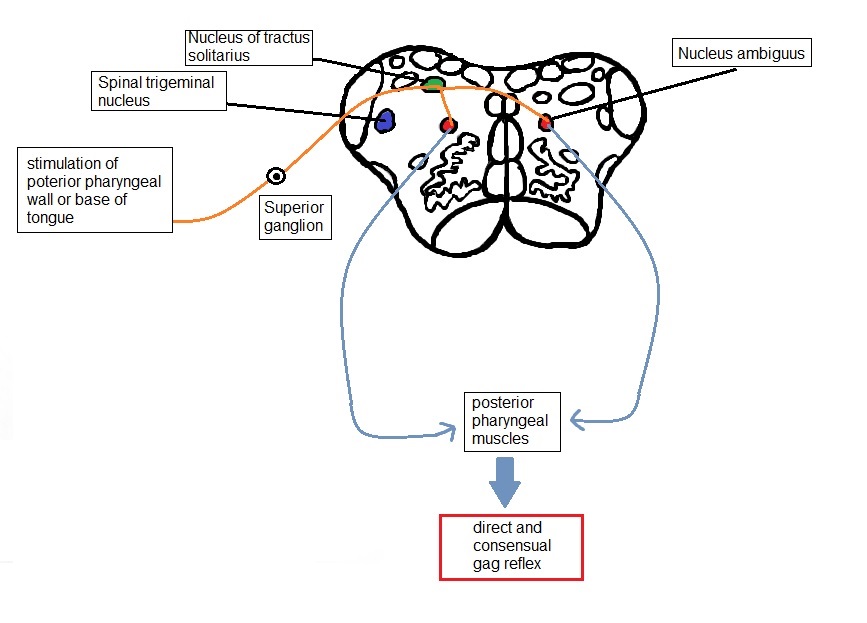
Control of the gag reflex is by both the glossopharyngeal (IX) and vagus (X) nerves, which serve as the afferent and the efferent limbs for the reflex arc, respectively. The nerve roots of cranial nerves IX and X exit the medulla through the jugular foramen and descend on either side of the pharynx to finally innervate the posterior pharynx, posterior one-third of the tongue, soft palate, and the stylopharyngeus muscle. [2]
The stimulus is provided by sensation to the posterior pharyngeal wall, the tonsillar pillars, or the base of the tongue. These sensations are carried by CN IX, which acts as the afferent limb of the reflex to the ipsilateral nucleus solitarius (also referred to as the gustatory nucleus) after synapsing at the superior ganglion located in the jugular foramen. These nuclei, in turn, send fibers to the nucleus ambiguus, which is a motor nucleus present in the rostral medulla. Efferent nerve fibers to the pharyngeal musculature traverse from the nucleus ambiguus through the CN X. This ultimately results in the bilateral contraction of the posterior pharyngeal muscles.
Contraction of the pharyngeal musculature ipsilateral to the side of the stimulus is known as the direct gag reflex, and contraction of the musculature on the contralateral side is known as the consensual gag reflex.
Testing the gag reflex can also help to assess damage to CN IX and CN X. Damage to CN IX leads to the absence of the gag reflex on the ipsilateral side. Damage to the CN X, however, leads to preserved gag reflex on the unaffected side with a lack of response on the affected side. This presentation is because the sensory afferent is intact, regardless of which side is stimulated. If both the X and IX nerves suffer damage on one side, there would be no consensual reflex on the affected side.
Stimulation of the soft palate can also elicit the gag reflex; however, the sensory limb, in this case, is the trigeminal nerve (CN V). Here, sensory stimulation of the soft palate travels through the nucleus of the spinal tract of the trigeminal nerve.
Related Testing
Equipment: The gag reflex can be elicited using a tongue blade or soft cotton applicator. In an intubated patient, a suction device may be most convenient to use for testing.
Technique: The examiner stimulates the posterior pharynx using a tongue blade or cotton applicator. After doing so, the patient will produce a gagging reaction, which may lead to vomiting in some patients. Additionally, the elevation of the bilateral posterior pharyngeal muscles requires examination. In a study among 104 medical students assessing the gag reflex, researchers noticed that stimulation of the posterior pharynx was more likely to elicit a gag reflex as compared to stimulation of the posterior tongue.[3]
An asymmetric response or absence of response when stimulating one side indicates the presence of pathology and warrants further assessment.
- Alternatives: The soft palatal reflex can help to assess the function of CN IX and X, as this reflex may be intact in the absence of gag reflex. The voice is evaluated by looking for hoarseness and dysphonia to determine CN X pathology. Research has also found that the cough reflex was better reproduced in intubated patients than the gag reflex to test for brainstem function.[4]
- Embracing health care team options: As there are a variety of techniques used to assess the gag reflex, there is poor inter-observer agreement. Hence, a standard method of examining patients for specific determined clinical scenarios is warranted. The gag reflex, however, remains imperative in assessing brainstem function, especially in the setting of brain death.
Contraindications:
During the assessment of the airway for intubation in an obtunded patient, the gag reflex should not be performed due to the risk of vomiting and subsequent aspiration.[5]
It may be difficult to assess the oral cavity in patients with a hypersensitive gag reflex. These patients may benefit from intravenous sedation during prosthodontic treatment.[6]
Clinical Significance
The gag reflex once served as a method to detect dysphagia in the setting of acute stroke. In one study comparing gag reflex to bedside swallowing assessment in 242 patients, the researchers found that the absence of gag reflex was specific for and consistent with the inability to swallow as assessed at the bedside but not sensitive in stroke patients. The study showed that the specificity of the gag reflex in detecting dysphagia was 96%, and sensitivity was to be 39%. However, an intact gag reflex does indicate the presence of protection against long term swallowing issues and predicts a decreased requirement for enteral feeding in the future.[7]
research has found that the posterior pharyngeal muscles that control the gag reflex are independent of the muscles responsible for swallowing. Therefore, clinicians should not rely upon an absent gag reflex as a predictor for aspiration in stroke patients. Indirect laryngoscopy has demonstrated to be a better alternative to performing the gag reflex to assess airway safety. Researchers have also noted that one out of three people may lack a gag reflex, through habituation, or influenced by emotions through higher centers. Pharyngeal sensation, in contrast, is rarely absent and is thus used as an alternative to gag reflex testing and could prove better at predicting future problems with swallowing.[3][7][8]
Before intubating a patient, deep sedation is necessary to confirm the absence of the gag reflex, which is in contrast to when patients receive only minimal and moderate sedation, where the presence of the gag reflex should be confirmed so that the airway is protected.[9]
Finally, performing the gag reflex is a must when assessing brainstem function as part of determining brain death. Confirmation of brain death is done in part by absent brainstem reflexes, which includes absent gag reflex.[10]