Gardnerella
- Article Author:
- Norah Kairys
- Article Editor:
- Manish Garg
- Updated:
- 8/15/2020 11:05:43 PM
- For CME on this topic:
- Gardnerella CME
- PubMed Link:
- Gardnerella
Introduction
Gardnerella vaginalis is an anaerobic bacterium that resides in the normal vaginal flora.[1] Normally, vaginal flora is predominated by the Lactobacilli species, but when organisms such as Gardnerella begin to overgrow and become the dominant species, this leads to bacterial vaginosis (BV).[1] Gardnerella was named after Hermann L. Gardner, who discovered the bacterium in 1955.[1] The bacteria are thought to be sexually transmitted between partners and can create a biofilm that progresses into BV.[1] BV is the most common cause of vaginal discharge.[1] Of clinical consequence, BV is associated with preterm birth and increased risk for acquisition of human immunodeficiency virus (HIV) and other sexually transmitted infections (STIs).[1]
Etiology
Although Gardnerella is not considered to be contagious, the role of transmissibility is yet to be completely understood.[2] The spread of this bacteria among individuals through sexual intercourse may alter the natural balance of bacteria within the vagina, and this imbalance can even lead to the development of BV.[2] Typically, BV is caused by a decrease in the number of normal hydrogen peroxide-producing Lactobacilli with an overgrowth of anaerobic bacteria such as G. vaginalis.[2]
Historically, bacterial vaginosis was called G. vaginitis because it was believed that this bacterium caused the condition.[1] However, the newer name helps to highlight the fact that a variety of bacteria that naturally live in the vaginal canal may grow in excess and it is specifically this imbalance that causes this condition.
Factors that may play a role in the development of bacterial vaginosis include frequent tub baths, douching, multiple sex partners, use of over the counter intravaginal hygiene products and increased frequency of sexual intercourse.
Epidemiology
Studies have detected G. vaginalis in up to 50% of women even without symptoms of BV.[3] Thus it has been presumed that Gardnerella may be part of the normal vaginal flora.[3] Additionally, BV is the most common vaginal infection found in women of reproductive age and is estimated to occur in 5% to 70% of women.[3][4] Gardnerella has consistently been isolated as a key pathogen in BV, suggesting a high overall prevalence of Gardnerella in this population.[3]
BV is most common in African American women compared to Caucasians. The condition rarely develops n males. BV is a condition seen in women of reproductive age.
Pathophysiology
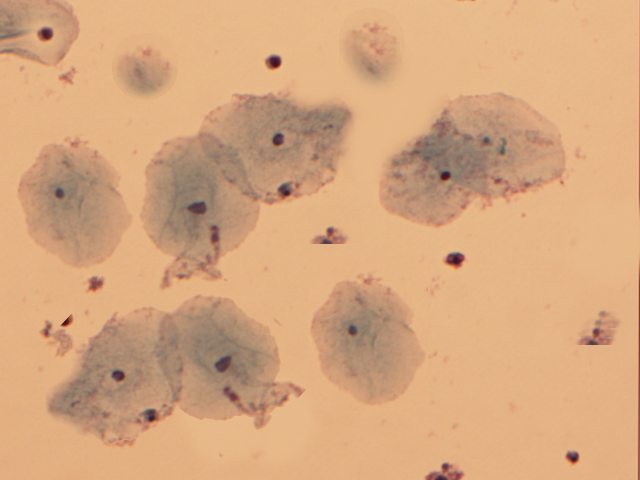
Although uncertain, it is thought that most BV infections start with a biofilm created by G. vaginalis which then allows other opportunistic bacteria to grow.[5] Bacterial vaginosis is characterized by the presence of clue cells, which are epithelial cells of the cervix that are covered with rod-shaped bacteria.[6]
G. vaginalis itself produces a pore-forming toxin, vaginolysin, that can only affect human cells.[6] Vaginolysin is a cholesterol-dependent cytolysin that initiates complex signaling cascades that induce target cell lysis and allow for Gardnerella’s virulence.[6] Additionally, protease and sialidase enzyme activities typically accompany this bacterium.[6] Gardnerella has the necessary virulence factors to adhere to host epithelia, which allows it to compete with Lactobacilli for dominance in the vaginal environment successfully.[6] The symptoms of BV are thought to be caused by an increase in normally dormant vaginal anaerobes that create symbiotic relationships with Gardnerella.[6]
Histopathology
Gardnerella is a non-spore-forming, non-motile Coccobacillus.[2] The bacterium can be grown to form small round gray colonies on both chocolate and Human Blood Tween agar.[7] A selective medium for Gardnerella is colistin-oxolinic acid blood sugar.[7] Gardnerella has a thin gram-positive cell wall but is considered to be gram-variable because it can appear either gram-positive or gram-negative under the microscope due to the varying visibility of this thin cell wall.[7]
History and Physical
Women colonized with G. vaginalis are typically asymptomatic unless they have bacterial vaginosis.[8] Most women with BV present with a complaint of malodorous vaginal discharge, which often becomes more pronounced after sexual intercourse. A diagnosis of BV is suggested by a higher than normal vaginal pH (greater than 4.5), the presence of clue cells on a wet-mount slide, and a positive whiff test.[8] A drop of sodium chloride solution is placed on the wet-mount slide containing some of the swab specimens, and the slide is examined under the microscope for visualization of the characteristic clue cells.[9] The whiff test is performed by adding a small amount of potassium hydroxide (KOH) to the microscopic slide containing the vaginal discharge and is considered to be positive if a characteristic fishy-scent is revealed.[9] Typically, two of these positive tests, as well as the presence of the characteristic discharge, is enough to confirm the diagnosis of BV.[8] If no discharge is present, then all of these criteria are needed to make the diagnosis.[8]
Evaluation
Before the identification of the rapid identification method, the only way to isolate Gardnerella was by growing cultures on selective agar medium.[10] With the advent of the rapid identification method in 1982 (a micro-method based on starch and raffinose fermentation and hippurate hydrolysis), 91.4% of the strains of Gardnerella were able to be isolated without the need for culture and Gram stain.[10]
Occasionally a Gram stain of the vaginal fluid is still done to examine the predominant strain of bacteria to make a microbiological diagnosis of BV. This technique, referred to as Nugent criteria, has a sensitivity and specificity of 89% and 83%, respectively.[10]
Treatment / Management
Asymptomatic Gardnerella colonization does not need to be treated. It has even been reported that up to 30% of cases of BV may even resolve on its own without treatment.[1] However, if a patient is bothered by the symptoms of BV, or is pregnant, it should be treated with either oral or vaginal clindamycin or metronidazole.[1][11]Unfortunately, it has been shown that recurrence may occur in up to 80% of women after treatment.[1][12] If a patient presents with recurrent symptoms, a second course of antibiotics is typically prescribed.[1] A 2009 Cochrane review found tentative but insufficient evidence to support the use of probiotics as treatment or prevention of BV.[13]
Differential Diagnosis
A proper pelvic exam can help to narrow down the differntial diagnosis and exclude other similarly presenting diseases such as herpes simplex virus.[1] Speculum exam can look for cervicitis and a wet mount of the vaginal discharge can determine if there is candidiasis or trichomoniasis.[1] Additional cervical swab cultures can be sent for chlamydia and gonorrhea.[14]
Prognosis
Most uncomplicated cases of bacterial vaginosis resolve with treatment. However, recurrences are not uncommon. Over time, BV is a risk factor for acquiring HIV. Over the past decade, there have been multiple reports of resistant strains that do not resolve with conventional treatment.
Complications
BV can lead to the following:
- Increased risk for endometritis and salpingitis
- Increased risk of post-surgery infections
- Adverse outcomes in pregnancy including premature labor, premature rupture of membranes and postpartum endometritis.
- Pelvic inflammatory disease
- Neonatal meningitis
Pearls and Other Issues
Untreated BV can lead to increased risk of pregnancy complications and STIs, including HIV.[14] Data also suggest an association between BV and both tubal factor infertility and pelvic inflammatory disease.[15] During pregnancy, BV has been associated with an increased risk of premature birth and miscarriage.[15] It also has been shown to increase the risk of chorioamnionitis, premature rupture of membranes and postpartum endometritis.[15]
Enhancing Healthcare Team Outcomes
Gardnerella is a common genital infection that is often encountered by the emergency department physician, nurse practitioner, internist, and the gynecologist. Asymptomatic Gardnerella colonization does not need to be treated as nearly 30% of cases resolve spontaneously. All symptomatic patients need treatment but despite treatment, recurrences are common.
Untreated BV can lead to increased risk of pregnancy complications and STIs, including HIV.[14] Data also suggest an association between BV and both tubal factor infertility and pelvic inflammatory disease.[15]
These patients need to be followed by the nurse practitioner until all symptoms have disappeared.
Even though BV is not a sexually transmitted infection, the nurse practitioner should educate the patient on the importance of safe sex measures, avoidance of multiple sex partners and use of barrier protection.