Ghon Complex
- Article Author:
- Benjamin Delgado
- Article Editor:
- Tushar Bajaj
- Updated:
- 9/21/2020 9:19:44 AM
- For CME on this topic:
- Ghon Complex CME
- PubMed Link:
- Ghon Complex
Definition/Introduction
The first report of the Ghon complex was by Anton Ghon (1866-1936), an Austrian pathologist who described primary tuberculosis to have the findings of a pulmonary lesion with regional lymph involvement caused by Mycobacterium tuberculosis. Primary pulmonary tuberculosis (TB) infection on chest radiography commonly presents with either one of the following four presentations: parenchymal disease, lymphadenopathy, pleural effusions, miliary tuberculosis, and the possibility of any combination of these. Specifically, in parenchymal disease, primary TB is hallmarked with a pulmonary lesion (also known as a Ghon lesion or Ghon focus) and affected draining lymph node adenopathy forming the Ghon's complex.[1]
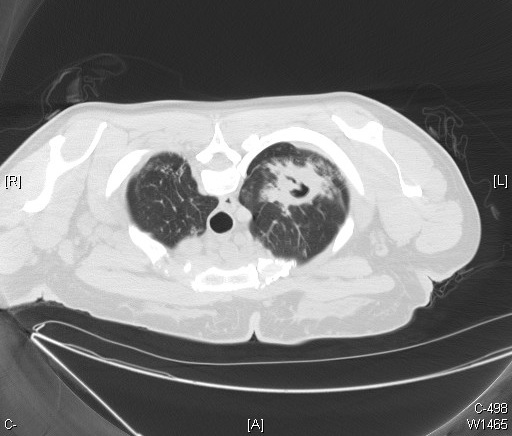
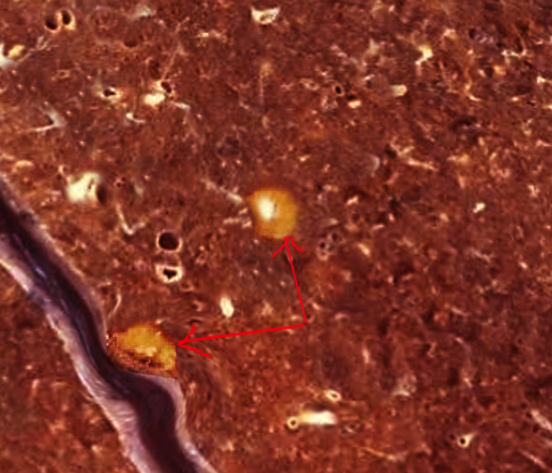
The Ghon complex is a non-pathognomonic radiographic finding on a chest x-ray that is significant for pulmonary infection of tuberculosis. The location of the Ghon's focus is usually subpleural and predominantly in the upper part of the lower lobe and lower part of the middle or upper lobe. The predilection for this area is because the ventilation is best in this region, and the most frequently encountered route of infection is through the respiratory tract. Radiographic findings of the Ghon focus may include parenchymal scarring of the lung tissue, lesion cavitation, or lobar consolidation, as seen in Figures 1, Figure 2, and Figure 3. The Ghon complex should not be confused with the Ranke complex. The Ghon complex precedes the development of a Ranke complex, in that a Ghon complex is seen in untreated primary pulmonary tuberculosis infection with Ghon lesion fibrosis while the Ranke complex is a result of the healing of a primary tuberculosis Ghon complex characterized by a calcified Ghon lesion and calcified mediastinal lymph nodes.[2]
Issues of Concern
In 2016, it estimates were that TB was responsible for the cause of 1.3 million deaths among human immunodeficiency virus (HIV)-negative individuals and remained globally, one of the leading infectious disease causes of death.[3] There is a higher prevalence of pulmonary TB among individuals of the eastern hemisphere found in third world countries due to disparities in access to healthcare for diagnostic evaluation and treatment with medications. Although less common in the western hemisphere, pulmonary TB continues to affect individuals of developed countries, specifically patients who have human immunodeficiency virus and acquired immune deficiency syndrome (HIV/AIDS) as an opportunistic infection, chronic renal failure, exposure to silica dust without silicosis, treatment with immunosuppressive medications (such as tumor necrosis factor-alpha inhibitors), and patients with substance use disorder of either tobacco, alcohol, or drug abuse.[3]
Estimates are that 1.7 billion people have TB infection, but only 5% to 15% of these individuals may develop TB disease.[3][4] The World Health Organization (WHO) in 2015 has set out to end the global burden of TB related deaths worldwide. In doing so, the WHO’s “End TB Strategy” has the goal of reducing both the incidence and death rate caused by TB by 90% and 95%, respectively. This plan aligns with intending to reduce the global burden of TB to be similar to the burden of incidence in developed countries today by the year 2035.[5]
Clinical Significance
The diagnosis of primary tuberculosis heavily relies on confirmatory specimen culture for M.tuberculosis from either sputum, nasopharyngeal aspirate, gastric aspirate, or pleural fluid. Nucleic acid amplification tests (such as the Xpert MTB/RIF assay), serological test, and chest radiography support the diagnosis of pulmonary TB.[6] The Ghon complex is not always present in a patient with primary TB infections. Researchers estimate that in about 15% of cases of primary TB, a Ghon focus may develop, while 9% of cases of primary TB may develop tuberculomas (Figure 4), and lymphadenopathy presents in children and adults only 96% and 43% of cases respectively.[7]
An estimated two-thirds of cases of primary TB, a parenchymal focus, resolves on its own, and overall, about 15% of patients with primary TB may present with normal chest radiography.[7][8] Due to the nature of M.tuberculosis's ability to spread from the respiratory tract to distant parts of the body by lymphatic and hematogenous routes, untreated primary pulmonary tuberculosis can result in latent disease and extrapulmonary TB of the pericardium and myocardium, central nervous system, head, and neck, musculoskeletal variants of arthritis, spondylitis, and osteomyelitis, either abdominal organs or gastrointestinal tract, and the genitourinary tract. Pulmonary tuberculosis is a curable disease that requires extended use of antibiotics. It appears in the literature that there is multiple drug-resistant (MDR) or extensively drug-resistant (XDR) tuberculosis, which requires clinicians to monitor a patient's response to tuberculosis treatment carefully.[9][10]
Nursing, Allied Health, and Interprofessional Team Interventions
Healthcare workers are at a higher risk of becoming infected by M.tuberculosis when compared to the general population.[11] Respiratory droplets transmit pulmonary TB from an infected host with primary TB. M.Tuberculosis may aerosolize into the air when an infected patients cough or sneeze, and the suspicions are that these aerosolized particles remain suspended in the air for an extended period. It is imperative that clinicians, nurses, and auxiliary staff practice with the necessary precautions when caring and treating patients with pulmonary TB. In the acute care setting, nurses tend to spend more time interacting with patients infected with primary TB when compared to other clinicians.
Nurses should first know the signs and symptoms of primary TB to minimize their possible risk of exposure to infected patients. Briefly, the signs and symptoms of primary TB include but are not limited to a patient with the following: chronic cough, hemoptysis, unintentional weight loss, fever and chills, night sweats, loss of appetite, and recent travel to endemic areas or contact with a person with TB, and fatigue.[12] After identifying a patient to have primary TB, possibly, nurses and healthcare workers should follow their healthcare facilities protocols for minimizing their occupational exposure to TB. In the middle to high-income resource areas, healthcare facilities may provide personal protective equipment such as respiratory masks, gloves, and disposable gowns for airborne precautions. In addition to minimizing the healthcare workers risk of exposure to TB, the patient population within the hospital risk of TB exposure is also minimized by the use of contact isolation rooms equipped with negative pressure air circulation to prevent airborne TB room air from contaminating room air outside of the patient isolation area. Often when a patient gets admitted to the hospital for treatment of primary TB, nurses play a vital role in the care of the patient. Qualitative studies have described that nursing interventions enhance patient adherence to treatment and community-based treatment of MDR TB.[13][14]
Nursing, Allied Health, and Interprofessional Team Monitoring
Once there is a diagnosis of tuberculosis, patients need long term follow-up. An infectious disease nurse should monitor these patients for medication compliance and clinical improvement. The treatment is often for 6 to 9 months, and the radiological improvements often lag behind the clinical symptoms. The patient should be encouraged to stop smoking, eat healthily, and avoid living in crowded environments.
(Click Image to Enlarge)

An anteroposterior X-ray of a patient diagnosed with advanced bilateral pulmonary tuberculosis. This AP X-ray of the chest reveals the presence of bilateral pulmonary infiltrate (white triangles), and „caving formation“ (black arrows) present in the right apical region. The diagnosis is far-advanced tuberculosis.
Contributed by The Centers for Disease Control and Prevention (PD-USGov-HHS-CDC)
(Click Image to Enlarge)