
Anatomy, Bony Pelvis and Lower Limb, Gluteus Medius Muscle
- Article Author:
- Aashin Shah
- Article Editor:
- Bruno Bordoni
- Updated:
- 4/29/2020 10:20:08 AM
- For CME on this topic:
- Anatomy, Bony Pelvis and Lower Limb, Gluteus Medius Muscle CME
- PubMed Link:
- Anatomy, Bony Pelvis and Lower Limb, Gluteus Medius Muscle
Introduction
The three muscles that form the gluteal region are gluteus medius, gluteus maximus, and gluteus minimus. The gluteus medius is a muscle lying between the gluteus maximus and gluteus minimus. Its posterior third is covered by gluteus maximus while the anterior two-third is superficial, covered only by a strong layer of deep fascia. Gluteus medius lies on top of the gluteus minimus, covering the minimus muscle. It is a broad muscle covering the exterior surface of ilium between the anterior and posterior gluteal lines. The posterior fibers of gluteus medius converge to form a flat tendon slanting downward and forward towards the superoposterior facet of the greater trochanter of the femur. The anterolateral part runs posteriorly toward the lateral facet of the greater trochanter of the femur. Both the parts insert into the lateral surface of the greater trochanter of femur via fibrocartilage.[1]
Structure and Function
Gluteus medius is the primary hip abductor. Gluteus minimus and the tensor fascia latae also serve as additional hip abductors. Both gluteus medius and minimus act from the pelvis to abduct the thigh and rotate it internally. The anterior fibers help with internal rotation of the thigh while the posterior fibers help with lateral rotation when the knee is in extension. Gluteus medius acts from the femur to stabilize the pelvis and maintain the trunk upright when standing on one leg, during running, and while walking when one leg is off the ground. With one foot being off the ground, the bodyweight tends to make the pelvis sag downwards on the unsupported side. Gluteus medius and minimus of the supported side counteract this force by powerful traction on the hip bone. The pelvis is prevented from sagging downwards and may even be raised a little on the unsupported side. The force produced by hip abductor muscles to maintain stability during single-limb support accounts for most of the compressive force generated between the acetabulum and femoral head.[2]
It is a flat, triangular muscle, located under and in front of the gluteus maximus. It originates from that part of the external face of the hip bone placed between the anterior and posterior gluteal lines, from the external lip of the iliac crest, from the anterior superior iliac spine and the gluteal fascia. The muscle bundles fan-fold downwards, gathering in a tendon that inserts on the external face of the greater trochanter. The muscle is covered by a thick sheet of the gluteal fascia, by the great gluteus and by the tensor of the lata fascia; it is deeply related to the small gluteus and the hip bone.
The muscle-tendon varies its thickness; the anterior and lateral portion merges laterally to the greater trochanter and has a lesser thickness than the posterior portion, which merges on the super-posterior area of the greater trochanter. The tendon inserts with fibrocartilage histology.
Embryology
The lower limb bud forms at around four weeks, corresponding to embryonic stage 14. By stage 17, the lower limb has a flattened footplate with an identifiable hip joint but no true knee. During stages 20 to 23, the digits separate and toes are clearly defined by stage 23, which corresponds to the end of week eight. Gluteus medius, like other skeletal muscles, is formed by cells derived from somites present at the level of the lower limb bud. These cells demyelinate from the hypaxial edge of the dermomyotome. They subsequently migrate into the limb bud and proliferate there. With the expression of myogenic determination factors, they eventually differentiate into the gluteus medius muscle.[3]
Blood Supply and Lymphatics
Superior gluteal artery supplies the gluteus medius muscle. It is the largest branch of the internal iliac artery. The artery travels posteriorly between the first sacral ramus and the lumbosacral trunk. It exits the pelvis via the greater sciatic foramen superior to the piriformis and further divides into deep and superficial branches. The deep branch passes between the gluteus medius and the surface of the bone and divides into inferior and superior branches, the superior branch inserts into the gluteus medius via 4 to 7 perforators and 0 to 2 perforators to gluteus minimus.[4] It anastomoses with an ascending branch of the lateral circumflex femoral artery and the deep circumflex iliac artery. The inferior branch runs obliquely through gluteus medius and supplies it via 3 to 8 perforators and gluteus minimus via 1 to 3 perforators.[4] It anastomoses with the lateral circumflex femoral artery. The superior gluteal artery exits the pelvis at an acute angle, which increases its vulnerability to shearing forces. The sharp fascia of the piriformis may compromise the artery during displaced fractures. Surgical procedures such as acetabular fracture surgery place the superior gluteal vessels and nerve at risk of injury.[5] The superior gluteal artery rarely arises from the internal pudendal artery. It occasionally arises with the inferior gluteal artery directly from the internal iliac artery. Internal iliac nodes surround the branches of internal iliac vessels which receive the lymphatic drainage of the gluteal region. The common iliac nodes receive lymphatic drainage from the internal iliac nodes, which lie around the common iliac artery. The common iliac nodes empty into the lateral aortic nodes.
The superior gluteal vein (SGV) drains blood from the gluteal region through two branches: superficial branch and deep branch. SGV runs together with the upper gluteal artery, enters the pelvis through the large ischial foramen, in the supra-pyriform canal, and ends in the internal iliac vein. The SGV anastomoses with the inferior gluteal vein.
The inferior gluteal vein (IGV) drains the posterosuperior region of the thigh and buttock. It originates from double branches that converge in a single trunk that runs together with the lower gluteal artery. The IGV anastomoses with the medial circumflex veins of the femur and the superior perforating vein, which are tributaries of the deep femoral vein. IGV enters the pelvis through the lower part of the large ischial foramen and flows into the distal portion of the internal iliac vein.
Nerves
The gluteus medius receives nerve supply from the superior gluteal nerve. The superior gluteal nerve originates from the dorsal branches of the L4, L5, and S1 nerve roots of the sacral plexus.[6] The nerve exits the pelvis through the greater sciatic foramen above the piriformis muscle and splits into inferior and superior branches.[6] The superior branch accompanies the upper branch of the deep division of the superior gluteal artery to innervate the gluteus minimus and gluteus medius. The inferior branch travels with the lower ramus of the deep division of the superior gluteal artery to innervate the gluteus minimus and medius, terminating in the tensor fascia latae muscle.
Muscles
When the gluteus medius muscle is subject to a functional alteration for various causes (trauma, injuries, pathologies), the muscle volume becomes reduced. This degeneration happens because the muscle is not properly involved in its actions, loses coordination, and consequently, its contractile activity decreases, losing volume.
Physiologic Variants
Cases, where the muscle has physiological, anatomical variations, do not seem to be observed in the literature.
Surgical Considerations
Gluteus medius and its supplying artery and nerve suffer damage due to hip fracture, hip dislocation, and hip arthroplasty. In a direct lateral approach during hip arthroplasty, the gluteus medius is surgically divided to gain access to the hip joint, and thus, this approach has the highest chance of nerve damage.[7] During the percutaneous placement of iliosacral screws, which is a popular technique employed to treat complicated injuries of the pelvis, the deep superior branch of the superior gluteal nerve and vessels are at significant risk even when utilizing soft tissue protecting cannulas, and the screws are appropriately placed.[8] Gluteus medius tear can present as chronic trochanteric bursitis resistant to medical treatment and requires surgical management.[9]
Clinical Significance
The gluteus medius and minimus can be tested together in a clinical setting by internal rotation of the thigh against resistance, with the hip and knee flexed while in a supine position. The gluteus medius and minimus along with the tensor fascia latae can be tested clinically by the abduction of the thigh against resistance with the knee extended while in a supine position. Both the gluteus medius and minimus act together to support the pelvis. The gluteus medius and minimus should be functioning adequately, and their innervation must be intact, the neck of the femur must be unbroken with its usual angulation to the shaft, and the constituents of the hip joint must be normal for the supportive effect of gluteus medius and minimus on the pelvis when raising the contralateral foot. When either of these conditions is affected, the pelvis sinks downwards on the unsupported side when the patient stands on the affected limb; this is known as the Trendelenburg sign. In cases of gluteus medius and minimus paralysis, patients will have a characteristic lurching gait, also known as Trendelenburg gait. If these two muscles and their innervations are intact, paralysis of other muscles acting on the hip joint will have little impact on walking or running. Greater trochanteric pain syndrome (GTPS) is attributable to tendinopathy of the gluteus medius and/or minimus with or without coexisting bursal pathology.[10] Patients commonly complain of lateral hip pain, localized to the greater trochanter, which increases with side-lying at night and weight-bearing activities.[10] It is diagnosed clinically by lateral hip pain with point tenderness at the greater trochanteric region. The pain increases with prolonged repetitive activity involving the gluteus medius such as walking, running, standing on one leg, or climbing stairs. The superior gluteal nerve can incur damage during an intramuscular injection in the gluteal region. It is advisable to administer injections in the upper lateral quadrant to avoid injuring the superior gluteal and sciatic nerve, the latter of which is usually found in the lower quadrants of the gluteal region.[6]
Other Issues
The gluteus medius muscle can cause compression of the vascular system (compartment syndrome); it can happen after trauma with the formation of a hematoma or a constant compression of the area due to loss of consciousness.[11]
Gluteus medius syndrome (GMS) is one of the causes that lead to back pain or leg pain and is similar but not equal to the greater trochanteric pain syndrome. GMS is associated with degeneration of the lumbar vertebrae, osteoarthritis at the level of the hips, and/or the knee; it can correlate with failed back surgery syndrome.[12]
A differential diagnosis to detect the presence of gluteus medius tears is to perform an internal counter-resistance rotation test.[13]
Calcification of the tendon of the gluteus medius muscle can mimic the presence of lumbar radiculopathy (lumbar hernia); an x-ray makes the diagnostic difference.[14]
The presence of pyomyositis in the gluteus medius muscle can give different clinical signs, such as pain in the path, pain in the hip, with fever, and high inflammatory indexes. The most suitable diagnostic difference is magnetic resonance imaging, which highlights the presence of inflammatory edema.[15]
An alteration of the function and/or structure of the gluteus medius muscle-tendon can cause snapping hip syndrome; the use of ultrasound imaging is the fastest tool for differential diagnosis.[16]
(Click Image to Enlarge)
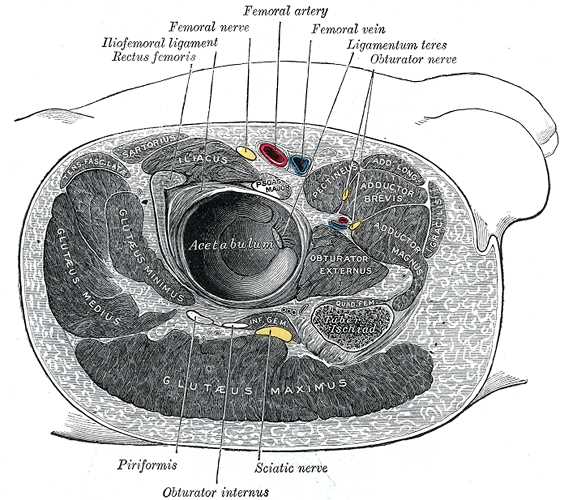
Structures Surrounding Right Hip-Joint, Iliofemoral ligament, Rectus Femoris, Femoral Nerve, Femoral Artery, Femoral Vein, Ligamentum Teres, Obturator nerve, Piriformis, Obturator Internus, Sciatic Nerve, Gluteus Maximus, Gluteus Medius, Gluteus Minimus, Acetabulum, Obturator Externus, Iliacus, Pectineus, Adductor Brevis, Adductor Magnus
Contributed by Gray's Anatomy Plates