
Anatomy, Bony Pelvis and Lower Limb, Gluteus Minimus Muscle
- Article Author:
- Anthony Greco
- Article Editor:
- Renato Vilella
- Updated:
- 7/27/2020 9:18:28 PM
- For CME on this topic:
- Anatomy, Bony Pelvis and Lower Limb, Gluteus Minimus Muscle CME
- PubMed Link:
- Anatomy, Bony Pelvis and Lower Limb, Gluteus Minimus Muscle
Introduction
Gluteus minimus is the smallest muscle of the glutei. It shares many similar features that of the gluteus medius, including structure and function, blood supply, and innervation. It is located just beneath the gluteus medius muscle. Gluteus minimus predominantly acts as a hip stabilizer and abductor of the hip. The muscle’s blood supply and innervation are from the superior gluteal artery and superior gluteal nerve, respectively. Damage to the nerve or muscle may result in sagging of the pelvis, also known as Trendelenburg sign. A total hip arthroplasty (THA) may indirectly or directly affect the gluteus minimus by damage to the superior gluteal nerve or by heterotopic ossification (HO). Other clinical significance includes greater trochanteric pain syndrome (GTPS) characterized by tendinopathy of the gluteus minimus. Patients will usually present with tenderness along the greater trochanter on the affected side.
Structure and Function
The proximal attachment of gluteus minimus is on the external surface of the ilium. This attachment lies between the anterior and inferior gluteal lines. The anterior gluteal line begins near the iliac crest taking a curved path posteriorly and inferior towards the greater sciatic notch. The inferior gluteal line follows a similar path but is shorter and less curved. The gluteus minimus is fan-shaped and is attached distally to the femur at the anterior border of the greater trochanter.[1]
The gluteus minimus is predominantly a hip stabilizer. Its main action is to abduct the hip. It starts to work when the individual is standing on one limb and works in conjunction with the gluteus medius and tensor fascia lata. The gluteus minimus is engaged on the supported side, which allows the pelvis to remain level during the swing phase of gait. The anterior portion of gluteus minimus also acts as a medial rotator of the thigh.[2][3][4]
Embryology
Gluteus minimus, like other limb muscles, arises from myoblasts that surround the developing bone. The myoblasts are formed due to tissues nearby that release molecular signals that allow somites to differentiate into myoblasts.[5] Myoblasts then coalesce together to form myotubes characterized by their long, tubular, and multinucleated structure. As the myotubes develop, they begin to form layers that will separate the muscle from neighboring connective tissue.[6] The lower limb buds start to form around the end of the fourth week, slightly delayed when compared to the upper limb buds. Additionally, the lower limb will rotate medially as the upper limb rotates laterally.
Blood Supply and Lymphatics
The blood supply to the gluteus minimus is supplied by the superior gluteal artery, which arises from the posterior division of the internal iliac artery. As the superior gluteal artery leaves the pelvis through the greater sciatic foramen above the piriformis, it passes posteriorly between the S1 nerve and lumbosacral trunk dividing into the superficial and deep branches. The deep branch of the superior gluteal artery supplies the gluteus minimus. Following the superior gluteal artery to its most distal point, it then anastomoses with the medial circumflex femoral arteries.[7]
Nerves
The superior gluteal nerve innervates the gluteus minimus. It is a branch of the lumbosacral plexus with nerve root origins of L4, L5, and S1. The nerve runs between gluteus minimus and medius alongside the superior gluteal artery’s deep branch. It then splits off into a superior branch and inferior branch. It is the inferior branch that supplies the gluteus minimus.[8][9] Injury to this nerve results in weakness with hip abduction and may result in a Trendelenburg gait.[10]
Muscles
Physiologic Variants
In some people, the gluteus minimus may have two divisions, the anterior and posterior segments. It may also send muscle fibers to the superior gemellus and/or the piriformis.[2]
Surgical Considerations
Nerve injury may occur in one to two percent of cases of a total hip arthroplasty (THA). Injury to the superior gluteal nerve may result in weakness with hip abduction and a Trendelenburg gait. Surgical exploration is indicated if the damage is due to compression of a large hematoma or direct laceration of the nerve.[11]
Another potential complication to consider following a THA is heterotopic ossification (HO) of gluteus minimus. HO characteristically demonstrates ectopic bone forming in extraskeletal tissues. Patients typically present with stiffness and pain of the hip approximately a few months following the surgery. Surgical resection is the recommended treatment if there is a severe loss of range of motion.[12]
Clinical Significance
Damage to gluteus minimus or the superior gluteal nerve may result in a Trendelenburg gait (gluteal gait). A positive Trendelenburg sign demonstrates pelvic sagging on an unsupported side when asked to stand on one leg; this indicates that the abductor muscles on the ipsilateral (supported) side are weak or non-functional. The gait presents as an individual leaning towards the supported side during the swing phase of the gait, to compensate for an appeared longer lower extremity due to the pelvis sagging on the unsupported side. Fractures to the greater trochanter may result in a Trendelenburg gait due to the location of the distal attachments of gluteus minimus.[10]
Tendinopathy of the gluteus minimus results in a condition known as Greater Trochanteric Pain Syndrome (GTPS). GTPS is characterized by lateral hip pain. It is often confused with trochanteric bursitis, which is a misleading term due to the direct involvement of the bursae and its very rare occurrence. GTPS resembles similarity to tendinopathy of the rotator cuff muscles in which the disorder occurs at the trochanteric enthesis. A physical examination will reveal tenderness to palpation of the greater trochanter and observation of a Trendelenburg gait.[13] Patients with suspected GTPS should have a standing anteroposterior radiograph of the pelvis to differentiate between hip osteoarthritis. Additionally, an ultrasound of the hip can help identify the offending lesion of the muscle.[14] The treatment for GTPS is supportive (nonsteroidal anti-inflammatory drugs and/or glucocorticoid injection) and activity modification targeted at relieving the stress of the gluteus minimus tendon.[15] Patients with persistent pain for two to three months should have a magnetic resonance imaging of the hip to rule out a partial or complete tear and referred to surgery for evaluation.[14]
Other Issues
The gluteus minimus muscle can be affected by trigger points. The most common characteristic of the gluteus minimus trigger point is a referred pain starting at the end of the lumbar spine and ending at the ankle (it is similar to the sciatic pain but without the symptoms of weakness, numbness).
(Click Image to Enlarge)
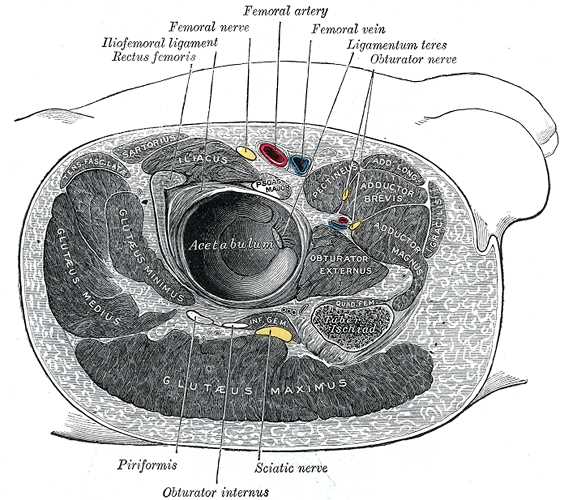
Structures Surrounding Right Hip-Joint, Iliofemoral ligament, Rectus Femoris, Femoral Nerve, Femoral Artery, Femoral Vein, Ligamentum Teres, Obturator nerve, Piriformis, Obturator Internus, Sciatic Nerve, Gluteus Maximus, Gluteus Medius, Gluteus Minimus, Acetabulum, Obturator Externus, Iliacus, Pectineus, Adductor Brevis, Adductor Magnus
Contributed by Gray's Anatomy Plates

