Anatomy, Bony Pelvis and Lower Limb, Thigh Gracilis Muscle
- Article Author:
- Irfan Khan
- Article Author:
- Bruno Bordoni
- Article Editor:
- Matthew Varacallo
- Updated:
- 8/13/2020 7:26:00 PM
- For CME on this topic:
- Anatomy, Bony Pelvis and Lower Limb, Thigh Gracilis Muscle CME
- PubMed Link:
- Anatomy, Bony Pelvis and Lower Limb, Thigh Gracilis Muscle
Introduction
The gracilis is a spiral unipennate muscle in the medial thigh compartment, which is innervated by the anterior branch of the obturator nerve and receives its vascular supply from the medial circumflex femoral artery, superficial femoral artery, deep femoral artery, descending genicular artery, and the anterior branch of the obturator artery. The gracilis assists with hip adduction, knee flexion, and knee internal rotation. The gracilis may suffer strain injury when patients have an adductor strain, which makes up 46.5% of hip and groin injuries in collegiate men's soccer, and is also common in hockey, football, and basketball athletes. Surgeons commonly use the gracilis for breast, craniofacial, lower limb, perineal, and anterior cruciate ligament (ACL) reconstruction, as well as other reconstructive surgeries.[1][2][3][4][5][6]
Structure and Function
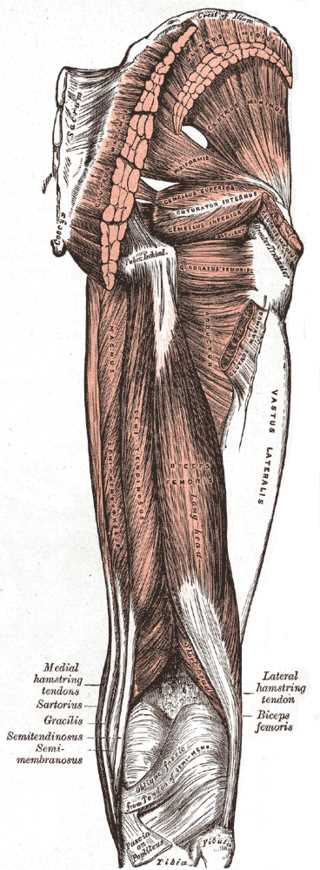
The gracilis is a long, thin muscle located in the medial compartment of the thigh. It originates on the medial aspect of the ischiopubic ramus and joins together with the sartorius and semitendinosus muscle tendons to form the pes anserine, which inserts on the superior medial tibia, medial to the tibial tuberosity. The gracilis has a spiral arrangement of muscle fiber bundles and the muscle fibers insert onto the anterior aspect of the gracilis tendon obliquely, making it a spiral unipennate muscle. There are 5 to 7 muscle fiber bundle compartments in the gracilis muscle, with nerve branches coursing along each compartment, which may indicate independent neuromuscular compartment functioning. Crossing both the hip and knee joints, the gracilis muscle performs hip adduction, hip flexion, hip internal rotation, knee flexion, and knee internal rotation.[1][4][3][7][8]
Embryology
The gracilis muscle derives from the mesoderm and can be found in the fetus starting from the eighteenth week. It is complete within the twenty-eighth week.
Blood Supply and Lymphatics
The gracilis obtains its vascular supply from the medial circumflex femoral artery, superficial femoral artery, deep femoral artery, descending genicular artery, and the anterior branch of the obturator artery. The anterior division of the internal iliac artery, the inferior epigastric artery, or the external iliac artery can give off the obturator artery, which traverses the ilioischial line, enters the obturator foramen, and splits into the anterior and posterior branch of the obturator nerve as it exits the obturator foramen. The external iliac artery turns into the common femoral artery as it passes the inguinal ligament. The common femoral artery splits into the superficial and deep femoral artery. The deep femoral artery then gives rise to the medial and lateral circumflex femoral arteries, while the superficial femoral artery gives rise to the descending genicular artery near its terminal end.[3][5][9][10]
When describing the neurovascular supply of the gracilis muscles, the terms major and minor pedicles are utilized. Major pedicles are areas where one artery (the major artery), two veins (venae comitantes), and the anterior branch of the obturator nerve enter the muscle, while minor pedicles are where one artery and two vena comitantes enter the muscle. The medial circumflex femoral artery, deep femoral artery, and the anterior branch of the obturator artery are the major arteries which may be present in major pedicles. Patients usually have one major pedicle going into the proximal anterior aspect of the gracilis; however, some patients may have two major pedicles. Once the major pedicle artery goes into the gracilis, it assumes one of three intramuscular distribution patterns:
- Type I (Dichotomous): The major artery splits into a proximal and distal branch. The proximal branch runs proximally from the pedicle insertion and ramifies to supply the proximal gracilis. The distal branch starts running distally in the muscle, and branches into two branches, each of which branch into an additional two branches.
- Type II (Array): The major artery enters the gracilis, and it runs diagonally (slightly towards the distal end) in an anterior-to-posterior direction, from which arrays of ascending and descending branches arise and supply the gracilis.
- Type III (Dual Pedicle): In patients with two major pedicles, both of the pedicles are present on the proximal anterior aspect of the gracilis. However, they do not have any connections between the major arteries or their branches. One pedicle major artery and its branches supply the proximal gracilis, and one pedicle major artery and its branches supply the distal gracilis.
The major artery typically supplies the posterior (deep) portion of the muscle, while the other branches of the major artery supply the anterior (superficial) portions of the gracilis.
The minor pedicle artery can be the superior femoral artery, deep femoral artery, or the descending genicular artery. Most of the minor pedicles are distal to the major pedicle(s). The artery of minor pedicles enter the gracilis anteriorly, and within the muscle, divides into ascending and descending branches. The ascending and descending branches form anastomoses with adjacent vessels, especially along the anterior aspect of the gracilis.
In the major and minor pedicles, each artery has two venae comitantes running alongside them, with one vein distal and anterior to the artery, and one vein proximal and posterior to the artery. Each vein has a distinct draining region. Veins only anastomose with minor pedicle arteries outside of the muscle, not within the muscle. When patients had two major pedicles, each major artery only had one vena comitante.[5][3]
Nerves
The obturator nerve originates from the L2 to L4 spinal nerve roots, and it traverses along the iliopectineal line, enters the obturator canal, and exits from the obturator forearm and splits into the anterior and posterior branches. The gracilis muscle receives innervation from the anterior branch of the obturator nerve. The major pedicle(s) contain the anterior branch of the obturator nerve, and typically the anterior branch of the obturator nerve forms two divisions, one which goes superficial to the pedicle, and one deep to the pedicle. From there, the nerve divides into two to six descending branches, which distally traverse the length of the muscle. From the main branch of the obturator nerve that entered the muscle, one or two branches go proximally and supply the proximal gracilis. There are variations with the paths of the vasculature (arteries and vena comitantes) and the nerves; they usually follow each other intramuscularly, but not always.[2][3]
Muscles
Female sex is more prone to ACL injury due to different knee muscle morphology than the male sex. This proclivity calculation was from the muscular relationship between extensor muscles and knee flexors.
In women, the muscular volume of the medial vastus is greater than in men, while the volume of the gracilis muscle (and the sartorius muscle) is smaller.
Surgical Considerations
Surgeons may use the gracilis tendon in reconstruction surgery of the ACL. The gracilis muscle has surgical use in patients who have lost muscular functioning of their digits, patients with facial palsy, or in patients with brachial plexus injuries. Since the gracilis can be split into independent neuromuscular compartments, utilizing a muscle transfer technique that applies multiple functioning compartments can achieve good functional outcomes. Additionally, the gracilis muscle may be used as a free tissue flap because it has predictable neurovascular pedicles, which can be used to repair large pelvic and perineal wounds, temporoparietal defects, anovaginal and rectovaginal fistulas.[4][3]
The gracilis muscle is part of the medial hamstrings group, which provides rotational, valgus, and anterior translation stability to the knee. When the gracilis is harvested to use as a graft for surgeries such as an ulnar collateral ligament reconstruction, external rotation of the knee is increased slightly, with no difference seen in anterior translation. When harvesting only the semitendinosus muscle, there is an increase in external rotation and anterior translation of the knee. When harvesting both the gracilis muscle and the semitendinosus for ACL reconstruction, a significant increase in external rotation, and anterior translation occurs. Additionally, when knees were ACL-deficient, and the semitendinosus and gracilis were both harvested, a significant increase in external rotation and anterior translation occurred, indicating the importance of the medial hamstrings group in stabilizing the knee in patients who are ACL-deficient, and further providing evidence for pre-ACL reconstruction hamstring strengthening. In patients who are high-performing athletes, altering knee dynamics may be detrimental to performance. Therefore, it is recommended to evaluate factors such as sport-specific demands in high-performing athletes when determining what ACL reconstruction graft to use, as well as when considering the use of a gracilis harvesting procedure to repair other conditions such as ulnar collateral ligament rupture.[7]
When harvesting the gracilis and semitendinosus tendons for a hamstring autograft ACL reconstruction, open or arthroscopic techniques can be utilized to harvest the tendons. When utilizing those techniques, it is important to be aware of the structures that possess associations with the tendons. The gracilis and semitendinosus tendons connect via intertendinous bands, they are both surrounded by a dense fascia that connects them to surrounding soft tissue, and each tendon may have accessory bands which connect them to each other or to structures such as the sartorius, gastrocnemius, or crural fascia. To facilitate a smooth harvest, it is important to dissect the intertendinous bands and make sure that the dense fascia around each tendon, or accessory bands, are not preventing the closed tendon stripper from harvesting the tendons.[11][12][13][1]
When selecting what tendon to use for a ligament reconstruction surgery, biomechanical properties such as elastic modulus should be accounted for to see if the graft tissue will be able to simulate the function of the original tissue it is replacing. The gracilis and semitendinosus tendons have a statistically significant higher elastic modulus (ability to resist elastic deformation) when compared to the patellar tendon, quadriceps tendon, and the iliotibial band (ITB). Additionally, there is a statistically significant lower strain in the gracilis and semitendinosus tendons when compared to the patellar tendon and ITB. Therefore, the hamstring tendons are stronger as ACL reconstruction grafts, when compared to the patellar tendon, quadriceps tendon, and ITB grafts. However, many factors exist, such as surgical technique and pre- and post-operative rehabilitation, which can play a role in graft success or failure and should be accounted for before selecting a graft for ACL reconstruction. Additionally, patient goals must be considered when selecting which graft is most appropriate for patients.[14]
Clinical Significance
Soccer, hockey, football, basketball, tennis, baseball, figure skating, baseball, and softball are all sports which have a high incidence of hip adductor muscle strains, especially in men’s collegiate soccer, in which 46.5% of all hip and groin injuries were adductor muscle strains. Since it is a common injury, and the gracilis muscle is part of the adductor group, it is vital for athletes to incorporate adductor muscle strengthening into their training, and to correct conditions such as over-pronation, which may predispose athletes to adductor strains.[6][8]
When patients present with atrophy of the gracilis muscle, along with atrophy of the adductor longus and adductor brevis, the inclusion of possible injury to the anterior branch of the obturator nerve should be in the differential diagnosis. Causes may include nerve impingement caused by a ganglionic cyst that emerges from the transverse acetabular ligament, neoplasm, or hematoma, or iatrogenic nerve injury caused by hip surgeries such as total hip replacements.[2]
When patients have pain along the distal portion of their gracilis tendon, where it becomes the pes anserine, there should be a high suspicion of pes anserine bursitis, especially if there is edema present. Pes anserine bursitis is commonly seen in patients who have obese, have osteoarthritis, and female.[15]