Anatomy, Thorax, Heart Great Vessels
- Article Author:
- Omar Bamalan
- Article Editor:
- Michael Soos
- Updated:
- 8/15/2020 11:35:26 PM
- For CME on this topic:
- Anatomy, Thorax, Heart Great Vessels CME
- PubMed Link:
- Anatomy, Thorax, Heart Great Vessels
Introduction
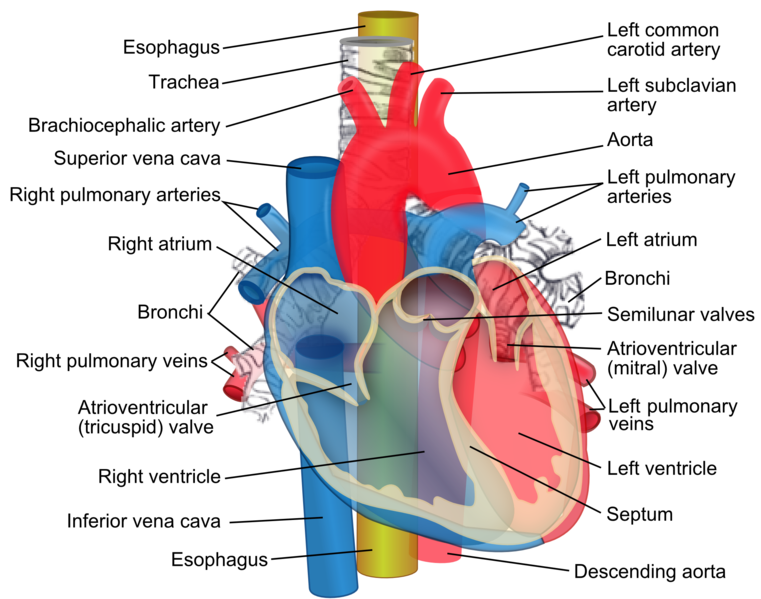
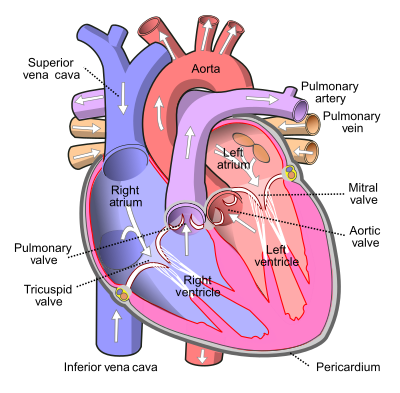
The heart is a vital organ that works in syncytium to pump, receive, and maintain constant blood flow throughout the body.[1] There are multiple major vessels connected directly to the heart, which are responsible for circulating oxygenated and the deoxygenated blood from and to the heart, respectively. The great vessels subdivide into the systemic and pulmonic circulation. The systemic circulation is responsible for the delivery of oxygenated blood to the body and deoxygenated blood to the right chambers of the heart. The great vessels involved in the systemic circulation include the Aorta (oxygenated blood), superior vena cava (SVC), and inferior vena cava (IVC) (deoxygenated blood). The pulmonary circulation made up of the vessels delivering deoxygenated blood to the lungs for gas exchange then deliver oxygenated blood from the lungs to the left chambers. The pulmonary circulation is made up of the right and left pulmonary arteries (deoxygenated blood) and the four pulmonary veins (oxygenated blood). These eight vessels are called the great heart/cardiac vessels. They have a relatively wider radius than other vessels to account for increased volume and pressure directed by the heart. The necessity of understanding the nature of their anatomy will lead us to understand the appropriate clinical approach that is necessary for different clinical pathologies.[2]
Structure and Function
The general anatomy of major vessels (arteries and veins) consists of three layers [3]:
- Tunica intima: The innermost layer of simple squamous epithelium
- Tunica media: The middle layer of connective tissue made up of elastin and smooth muscles
- Tunica adventitia: The outermost layer of thick collagenous tissue that maintains the structure of the great vessels.
The distinguishing features of the great heart vessels:
- The superior vena cava collects deoxygenated blood from the venous system associated with the upper limbs, head, neck, and thorax. The superior vena cava terminates in the right atrium providing deoxygenated blood to the pulmonary circulation. The tunica media of the superior vena cava has decreased levels of smooth muscles in comparison to similar vessels. Additionally, it has increased recoiling connective tissue that helps maintain the structure and efficiency of the vessel. The inferior vena cava is similar in structure to the superior vena cava. Both vessels lack the valvular characteristic of veins and have a wider radius to accommodate the increased circulating volume. Furthermore, both vessels directly connect to the right atrium, which has very low-pressure during the blood-filling time.
- The pulmonary arteries transport deoxygenated blood from the right ventricle to the lungs.
- The four pulmonary veins deliver the highly oxygenated blood from the lungs to the left atrium.
- The aorta is by far the thickest artery and is rich in elastin, collagen, and smooth muscle within both the tunica media and tunica adventitia due to the elevated pressures resulting from contraction of the left ventricle.
Embryology
The superior vena cava is formed mainly from the proximal right anterior cardinal veins and right common cardinal vein. The inferior vena cava forms from the fusion of the remaining cardinal veins, the subcardinal veins, and later the supracardinal veins. The separation between the subcardinal vein and the right posterior cardinal vein joins with the hepatic vein forming the inferior vena cava, which delivers deoxygenated blood from the lower limbs and abdominal viscera to the right atrium.
The formation of the aorta and the pulmonary trunk is dependent upon the truncus arteriosus. During development, the right and left conotruncal ridges to grow in a spiral, twisted fashion forming the great vessels.[4] This formation of the ridges is under the guidance of the combination of the mesenchymal cells that are going to create the semilunar valves (aortic and pulmonary semilunar valves) and the endocardial cells that are anteriorly and posteriorly conjoining to separate the ventricles. Eventually, from the fifth through eight weeks, an aorticopulmonary septum will result in the separation of the Aorta and pulmonary trunk.
The pulmonary veins become incorporated into the left atrium through the dorsal mesocardiac and mesenchymal guidance of the pulmonary venous plexus. The sinus venosus is responsible for the formation of the crista terminalis. Some of these physiological changes take place as the hypoxic pulmonary vasoconstriction effect on the cardiac right side won't keep the fossa ovale patent, and the left atrial pressure will cause its closure alongside the degradation of the ductus arteriosus between the pulmonary trunk and aortic arch.[5] Therefore, it results in a full separation of the four atrioventricular chambers, forming the fetal heart and great vessels.
Blood Supply and Lymphatics
The great vessels supply blood within a closed system of the systemic circulation and pulmonary circulation. The arteries and veins themselves receive vascular supply from a network of microcirculatory vessels supplying the aorta. This network is known as the vasa vasorum, which can originate internally from the arterial lumen, vasa vasorum internae, or externally by networks of vessels upon the tunica adventitia, known as the vasa vasorum externae.[6][3][7][8] The great vessels also have extensive microvascular networks known as the venous vasa vasorae originating from the mainly the tunica adventitia.
Nerves
The innervation of vessels derives from a network of interconnected plexuses of neuronal fibers that are called the nervi vasorum, which rest upon the tunica adventitia alongside the vasa vasorum externae. The primary innervation of the great vessels is the sympathetic chain, which utilizes adrenergic receptors to modulate vasoconstriction.[9] The parasympathetic system also has a partial stimulatory effect on endothelial cells, which antagonize the adrenergic receptors and result in vasodilation. Within the aortic arch, baro/chemoreceptor plexuses are derived from the vagus nerve and connect to the vasomotor nuclei located in the medulla oblongata, which helps to regulate response to changes in oxygen concentration and blood pressure. Veins are not strongly affected by sympathetic and parasympathetic systems due to the lack of muscle within the tunica media.[10] This lack of vasoconstriction within the venous system leads to an increased venous return via the great vessels to the right atrium.[11]
Muscles
The muscles within the tunica media of the great arteries play a significant role in efficiently meeting the physiological needs to propagate blood. When it comes to the venous system, vessels contain a thin layer of smooth muscles such that external factors must influence blood return. Changes in intrathoracic/intraabdominal pressure during respiration can affect the superior vena cava, inferior vena cava, and pulmonary veins' ability to deliver blood, in by creating pressure gradients.[12] Additionally, skeletal muscle contraction will also act to create a pressure gradient and as a peripheral venous pump.[13]
Surgical Considerations
Injury to any of the great vessels during any surgical intervention should be considered a major complication and carries a high risk of ischemia, necrosis, and possibly paralysis.[14][15][16] Due to the diameter of the great vessels, they are prone to injury and hemorrhage.[17] The great vessels are at increased risk for damage in patients with aneurysmal disease requiring surgical intervention.[18][19]
Clinical Significance
Understanding the anatomy and function of the great vessels is an essential consideration to many pathological and physiological phenomenon. On physical exam, there are various sites for the assessment of the integrity of the great vessels and their associated components.
- Aortic valve auscultation takes place at the right, second intercostal space.
- At the level of (T8), the inferior vena cava passes to the abdominal cavity through a diaphragmic foramen [20].
- Pulmonic valve auscultation is performed at the left, second intercostal space.
- Pulmonary veins are posterior to the heart and slightly inferior to the atria. Thus they are difficult to assess on physical exams.
Several congenital anomalies affect these great vessels. One example is transposition of the great vessels, where the aorta originates from the right ventricle and the pulmonary trunk from the left. Transposition correlates with other cardiac defects include ventricular septal defect and patent ductus arteriosus. The pathogenesis of this anomaly is not in the purview of this review. Other congenital anomalies include aortic valvular atresia, double superior vena cava or inferior vena cava, absent superior vena cava or inferior vena cava, aortic coarctation, pulmonic valvular stenosis. The clinician must understand the normal anatomical morphology and physiology of the great vessels to understand the significant variety of congenital abnormalities potentially encountered in clinical practice.[21][22][23][24]
(Click Image to Enlarge)