Head Trauma
- Article Author:
- Faizan Shaikh
- Article Editor:
- Muhammad Waseem
- Updated:
- 8/10/2020 9:29:10 PM
- For CME on this topic:
- Head Trauma CME
- PubMed Link:
- Head Trauma
Introduction
Traumatic brain injury (TBI) is a common presentation in emergency departments, which accounts for more than one million visits annually. It is a common cause of death and disability among children and adults.[1]
Based on the Glasgow Coma Scale (GCS) score, it is classified as:
- Mild = GCS 13 to 15, also called concussion
- Moderate = GCS 9 to 12
- Severe = GCS 3 to 8
Etiology
The leading causes of head trauma are (1) motor vehicle-related injuries, (2) falls, and (3) assaults.[2][3]
Based on the mechanism, head trauma is classified as (1) blunt (the most common mechanism), (2) penetrating (most fatal injuries), (3) blast.
Most severe TBIs result from motor vehicle collisions and falls.
Epidemiology
Pathophysiology
The following concepts are involved in the regulation of blood flow and should be considered.
1) Monroe-Kellie Doctrine
- Related to the understanding of intracranial pressure (ICP) dynamics.
- Any individual component of the intracranial vault may undergo alterations, but the total volume of intracranial contents remains constant since the space within the skull is fixed. In other words, the brain has a compensatory mechanism to maintain an equilibrium thereby maintaining normal intracranial pressure.
- According to this, the displacement of cerebrospinal fluid (CSF) or blood occurs to maintain normal ICP. A rise in ICP will occur when the compensatory mechanisms are exhausted.
2) Regulation of Cerebral Blood Flow (CBF) (Autoregulation)
- Under normal circumstances, the brain maintains CBF via auto-regulation which maintains equilibrium between oxygen delivery and metabolism.
- Autoregulation adjusts Cerebral perfusion pressure (CPP) from 50 to 150 mm Hg. Beyond this range, autoregulation is lost, and blood flow is only dependent on blood pressure.
- Severe brain injury may disrupt the autoregulation of CBF.
3) Cerebral Perfusion Pressure (CPP)
- The difference between the mean arterial pressure (MAP) and the ICP (CPP = MAP – ICP)
- Target CPP is 55 mm Hg to 60 mm Hg
- An increase in ICP can decrease the CPP
- A decrease in ICP may improve CPP
- Remember, lowering MAP in a hypotensive patient may lower CPP.
- A minimum CPP should be maintained to avoid cerebral insult. It is age-dependent and is as follows: Infants - 50 mm Hg, Children - 60 mm Hg, and Adults - 70 mm Hg.
- CBF is quite sensitive to oxygen and carbon dioxide.
- Hypoxia causes vasodilation and therefore increases CBF and may worsen ICP.
- Hypercarbia also results in vasodilation and can alter ICP via effects on cerebrospinal fluid (CSF) pH and increases CBF.
4) Mean arterial pressure (MAP)
- Maintain = 80 mm Hg
- 60 mm Hg = cerebral vessels maximally dilated
- < 60 mm Hg = cerebral ischemia
- > 150mmHg = increased ICP
5) Intracranial pressure (ICP)
- An increase in ICP can decrease CPP.
- ICP is dependent on the volume of the following compartments:
- Brain parenchyma (< 1300 mL)
- Cerebrospinal fluid (100 - 150 mL)
- Intravascular blood (100 - 150 mL)
- Cushing reflex (hypertension, bradycardia, and respiratory irregularity) due to an increase in ICP
- Normal ICP is age-dependent (adult younger than ten years old, child 3-7 years old, infant 1.5-6 years old)
- > 20 mm Hg= increased morbidity and mortality and should be treated. It is perhaps more important to maintain an adequate CPP.
TBI can be classified as primary injury and secondary injury:
Primary Injury
Primary injury includes injury upon the initial impact that causes displacement of the brain due to direct impact, rapid acceleration-deceleration, or penetration. These injuries may cause contusions, hematomas, or axonal injuries.
- Contusion (bruise on the brain parenchyma)
- Hematoma (subdural, epidural, intraparenchymal, intraventricular, and subarachnoid)
- Diffuse axonal injury (stress or damage to axons)
Secondary Injury/Secondary Neurotoxic Cascade
Secondary injury consists of the changes that occur after the initial insult. It can be due to:
- Systemic hypotension
- Hypoxia
- Increase in ICP
After a primary brain injury, a cascade of cellular and biochemical events occurs which include the release of glutamate into the presynaptic space resulting in activation of N-methyl-D-aspartate, a-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid, and other receptors. This ionic shift may activate cytoplasmic and nuclear enzymes, resulting in mitochondrial damage, and cell death and necrosis.
Brain Herniation
Herniation occurs due to increased ICP. The following are the types of herniations.
1) Uncal transtentorial
- The uncus is the most medial portion of the hemisphere, and the first structure to shift below the tentorium.
- Compression of parasympathetic fibers running with the third cranial nerve
- Ipsilateral fixed and dilated pupil with contralateral hemiparesis
2) Central transtentorial
- Midline lesions, such as lesions of the frontal or occipital lobes or vertex
- Bilateral pinpoint pupils, bilateral Babinski signs, and increased muscle tone. Fixed midpoint pupils follow along with prolonged hyperventilation and decorticate posturing
3) Cerebellar tonsillar
- Cerebellar tonsils herniate in a downward direction through the foramen magnum
- Compression on the lower brainstem and upper cervical spinal cord
- Pinpoint pupils, flaccid paralysis, and sudden death
4) Upward posterior fossa/cerebellar herniation
- The cerebellum is displaced in an upward direction through the tentorial opening
- Conjugate downward gaze with an absence of vertical eye movements and pinpoint pupils
History and Physical
A good history concerning the mechanism of injury is important. Follow advanced trauma life support protocol and perform primary, secondary, and tertiary surveys. Once the patient is stabilized, a neurologic examination should be conducted. CT scan is the diagnostic modality of choice in the initial evaluation of patients with head trauma.
The GCS is used to describe the level of consciousness. Patients who are intubated are only evaluated for motor scores and eye-opening and the suffix T is added to the final score. The maximal GCS score is 10T and the lowest is 2T.
Classification of TBI is as follows:
Clouding of consciousness, where there is a mild deficit in processing by the brain. It may persist for many months and the patient may have a loss of recent memory, but long term memory remains intact.
Lethargy is a state of depressed alertness and can result in an inability to perform tasks that are usually done without any effort. The patient may be aroused by stimuli but then settles back into a state of inactivity. Awareness of the environment is present.
Obtundation is a state of decreased alertness and awareness. The patient will briefly respond to stimuli and only follow simple commands, but will not be aware of the surroundings.
Stupor is when the patient cannot communicate lucidly and requires painful stimuli to be aroused. Once the stimulation is withdrawn, the patient returns to the inactive state.
Coma is when the patient is not able to respond to any type of stimuli
Evaluation
CT scan is required in patients with head trauma
- Moderate (GCS score 9 to 12)
- Severe (GCS score < 8)
For patients who are at low risk for intracranial injuries, there are two externally validated rules for when to obtain a head CT scan after TBI.[7][8]
It is important to understand that no individual history and physical examination findings can eliminate the possibility of intracranial injury in head trauma patients.
Skull x-rays are only used to assess for foreign bodies, gunshots or stab wounds
New Orleans Criteria
- Headache
- Vomiting (any)
- Age > 60 years
- Drug or alcohol intoxication
- Seizure
- Trauma visible above clavicles
- Short-term memory deficits
Canadian CT Head Rule
- Dangerous mechanism of injury
- Vomiting = two times
- Age > 65 years
- GCS score < 15, 2-hours post-injury
- Any sign of basal skull fracture
- Possible open or depressed skull fracture
- Amnesia for events 30 minutes before injury
Level A Recommendation
With the loss of consciousness or posttraumatic amnesia only if one or more of the following symptoms are present:
- Headache
- Vomiting
- Age > 60 years
- Drug or alcohol intoxication
- Deficits in short-term memory
- Physical findings suggestive of trauma above the clavicle
- Posttraumatic seizure
- GCS score < 15
- Focal neurologic deficit
- Coagulopathy
Level B Recommendation
Without loss of consciousness or posttraumatic amnesia if one of the following specific symptoms presents:
- Focal neurologic deficit
- Vomiting
- Severe headache
- Age > 65 years
- Physical signs of a basilar skull fracture
- GCS score < 15
- Coagulopathy
- Dangerous mechanism of injury
- Ejection from a motor vehicle (such as Pedestrian struck or a fall from a height > three feet or five stairs)
The risk of intracranial injury when clinical decision rule results are negative is less than 1%.
For children, Pediatric Emergency Care Applied Research Network (PECARN) decision rules exist to rule out the presence of clinically important traumatic brain injuries. However, this rule applies only to children with GCS > 14.
Treatment / Management
The most important goal is to prevent secondary brain injuries. This can be achieved by the following:
- Maintain airway and ventilation
- Maintain cerebral perfusion pressure
- Prevent secondary injuries (by recognizing and treating hypoxia, hypercapnia, or hypoperfusion)
- Evaluate and manage for increased ICP
- Obtain urgent neurosurgical consultation for intracranial mass lesions
- Identify and treat other life-threatening injuries or conditions (if they exist)
A relatively higher systemic blood pressure is needed:
- Increase in intracranial pressure
- Loss of autoregulation of cerebral circulation
Priorities remain the same: the ABC also applies to TBI. The purpose is to optimize perfusion and oxygenation.[1][9][10]
Airway and Breathing
Identify any condition which might compromise the airway, such as pneumothorax.
For sedation, consider using short-acting agents having minimal effect on blood pressure or ICP:
- Induction agents: Etomidate or propofol
- Paralytic agents: Succinylcholine or Rocuronium
Consider endotracheal intubation in the following situations:
- Inadequate ventilation or gas exchange such as hypercarbia, hypoxia, or apnea
- Severe injury (GCS score of = 8)
- Inability to protect the airway
- Agitated patient
- Need for patient transport
The cervical spine should be maintained in-line during intubation.
Nasotracheal intubation should be avoided in patients with facial trauma or basilar skull fracture.
Targets:
- Oxygen saturation > 90
- PaO2 > 60
- PCO at 35 - 45
Circulation
Avoid hypotension. Normal blood pressure may not be adequate to maintain adequate flow and CPP if ICP is elevated.
Target
- Systolic blood pressure > 90 mm Hg
- MAP > 80 mm Hg
Isolated head trauma usually does not cause hypotension. Look for another cause if the patient is in shock.
Increased ICP
Increased ICP can occur in head trauma patients resulting in the mass occupying lesion. Utilize a team approach to manage impending herniation.
Signs and symptoms:
- Change in mental status
- Irregular pupils
- Focal neurologic finding
- Posturing: decerebrate or decorticate
- Papilledema (may not be apparent with a rapid elevation of ICP)
CT scan findings:
- Attenuation of sulci and gyri
- Poor gray/white matter demarcation
General Measures
Head Position: Raise the head of the bed and maintain the head in midline position at 30 degrees: potential to improve cerebral blood flow by improving cerebral venous drainage.
Lower cerebral blood volume (CBV) can lower ICP.
Temperature Control: Fever should be avoided as it increases cerebral metabolic demand and affects ICP.
Seizure prophylaxis: Seizures should be avoided as they can also worsen CNS injury by increasing the metabolic requirement and may potentially increase ICP. Consider administering fosphenytoin at a loading dose of 20mg/kg.
Only use an anticonvulsant when it is necessary, as it may inhibit brain recovery.
Fluid management: The goal is to achieve euvolemia. This will help to maintain adequate cerebral perfusion. Hypovolemia in head trauma patients is harmful. Isotonic fluid such as normal saline or Ringer Lactate should be used. Also, avoid hypotonic fluid.
Sedation: Consider sedation as agitation and muscular activity may increase ICP.
- Fentanyl: Safe in intubated patients
- Propofol: A short-acting agent with good sedative properties, the potential to lower ICP, possible risk of hypotension and fatal acidosis
- Versed: sedative, anxiolytic, possible hypotension
- Ketamine: Avoid as it may increase ICP.
- Muscle relaxants: Vecuronium or Rocuronium are the best options for intubation; Succinylcholine should not be used as ICP may rise with fasciculations.
ICP monitoring:
- Severe head injury
- Moderate head injury with increased risk factors such as abnormal CT scan finding
- Patients who cannot be evaluated with serial neurological examination
- ICP monitoring is often done in patients with severe trauma with a GCS of less than 9. The reference range for normal CIP is 2-15 mmHg. In addition, the waveform of the tracing is important.
Hyperventilation:
Normocarbia is desired in most head trauma patients. The goal is to maintain PaCO between 35-45 mmHg. Judicious hyperventilation helps to reduce PaCO2 and causes cerebral vasoconstriction. Beware that, if extreme, it may reduce CPP to the point that exacerbation of secondary brain injury may occur. Avoid hypercarbia: PaCO > 45 may cause vasodilatation and increases ICP.
Mannitol:
A potent osmotic diuretic with net intravascular volume loss
Reduces ICP and improves cerebral blood flow, CPP, and brain metabolism
Expands plasma volume and can improve oxygen-carrying capacity
The onset of action is within 30 minutes
Duration of action is from two to eight hours
Dose is 0.25-1 g/kg (maximum: 4 g/kg/day)
Avoid serum sodium > 145 m Eq/L
- Serum sodium > 145 m Eq/L
- Serum osmolality > 315 mOsm
Relative contraindication: hypotension does not lower ICP in hypovolemic patients.
Hypertonic saline:
May be used in hypotensive patients or patients who are not adequately resuscitated.
The dose is 250 mL over 30 minutes.
Serum osmolality and serum sodium should be monitored.
Hypothermia may be used to lower cerebral metabolism but it is important to be aware that hypothermia also makes the patient susceptible to infections and hypotension.
Mild Head Trauma
The majority of head trauma is mild. These patients can be discharged following a normal neurological examination as there is minimal risk of developing an intracranial lesion.
Consider observing at least 4 to 6 hours if no imaging was obtained.
Consider hospitalization if these other risk factors are present:
- Bleeding disorder
- Patient taking anticoagulation therapy or antiplatelet therapy
- Previous neurosurgical procedure
Provide strict return precautions for patients discharged without imaging.
Differential Diagnosis
- Anterior circulation stroke
- Brain metastasis
- Cerebral aneurysm
- Confusional states and acute memory disorders
- Emergent management of subarachnoid haemorrhage
- Epileptic and epileptiform encephalopathies
- Frontal lobe syndromes
- Generalised tonic-clonic seizures
- Hydrocephalus
- Prion-related diseases
- Psychiatric disorders associated with epilepsy
- Subdural empyema
- Temporal lobe epilepsy
Prognosis
The outcomes after head trauma depend on many factors. The initial GCS score does provide some information on the outcome; the motor score is most predictive of outcome. Patients with a GCS of less than 8 at presentation have high mortality. Advanced age, comorbidity, respiratory distress, and a comatose state are also associated with poor outcomes.
Complications
- Deep vein thrombosis rates are higher in head trauma patients
- Neurological deficits
- CSF leak
- Hydrocephalus
- Infections
- Seizures
- Cerebral edema
Pearls and Other Issues
Hyperglycemia may worsen the outcome.
An elevated temperature may increase ICP and worsen outcomes.
- Increase metabolic demand
- Increase glutamate release
A prolonged seizure may worsen secondary brain injuries.
Enhancing Healthcare Team Outcomes
Head trauma is a major public health problem accounting for thousands of admissions each year and costing the healthcare system billions of dollars. The majority of patients with head trauma are seen in the emergency department; the head injury is often associated with other organ injuries as well. The care of a patient with head trauma is by an interprofessional team that is dedicated to managing head trauma patients.
Most patients require admission and monitoring in an ICU setting. The outcome of these patients depends on the severity of the head trauma, initial GCS score, and any other organ injury. Data indicate that those patients with an initial GCS of 8 or less have a mortality rate of 30% within 2 weeks of the injury. Other negative prognostic factors include advanced age, elevated intracranial pressure, and the presence of a gross neurologic deficit on presentation. ICU nurses play a vital role in the managing of these patients; from providing basic medical care, monitoring, DVT and ulcer prophylaxis and monitoring the patient for complications and reporting concerns to the team. The dietitian manages the nutrition and physical therapists provide bedside exercises to prevent muscle wasting.
Patients with a GCS less than 9 often require mechanical ventilation, tracheostomy, and a feeding tube. With prolonged hospital stay, there are prone to pressure ulcers, aspiration, sepsis, failure to thrive and deep vein thrombus. Patients deemed to be brain dead are assessed by the entire team that includes specialists from the end of life care.
Recovery in most patients can take months or even years. Even those who are discharged often have residual deficits in executive function or neurological deficits. Some require speech, occupational and physical therapy for months. In addition, the social worker should assess the home environment to make sure it is safe and offers amenities for the disabled person. Only through such a team approach can the morbidity of head trauma be lowered.
Outcomes
Unfortunately, despite the education of the public, many young people still lead a lifestyle that predisposes them to head injury. Young people still drink and drive, text while driving, abuse alcohol and illicit drugs, and are often involved in high-risk sporting activities, which makes them susceptible to head trauma.[11][12]
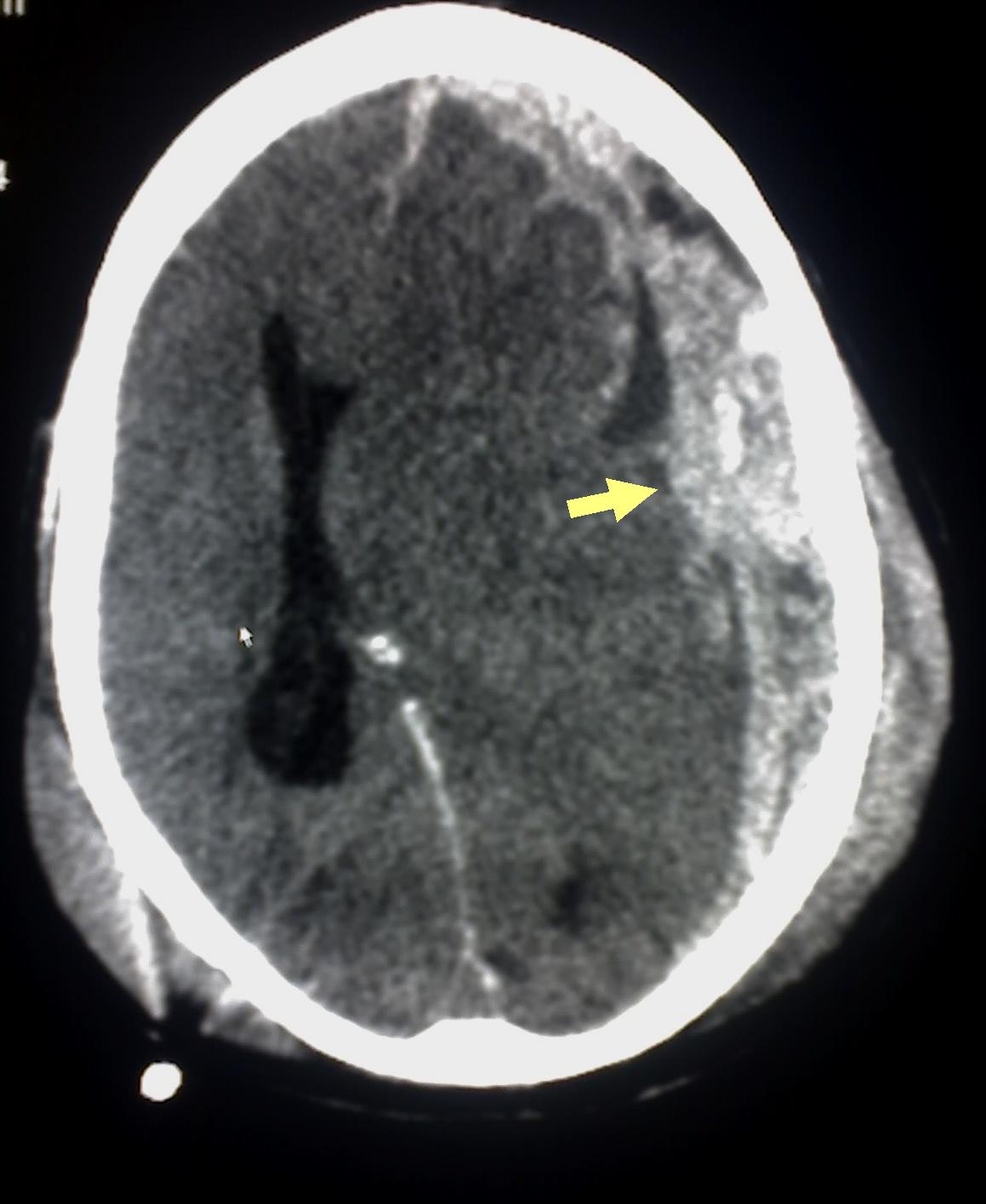
(Click Image to Enlarge)
(Click Image to Enlarge)

Original description: Figure 2. CT and enhanced gradient echo T2 star-weighted angiography (ESWAN) images of the brain of a 54-year-old man who experienced a traumatic brain injury. An axial head CT image displays right frontotemporal SAH (Fisher grade 4) with bilateral frontal contusions and intracerebral hematoma (A). A follow-up CT image 26 weeks after the brain injury indicates that the hemorrhages were completely resolved and the lateral ventricles were mildly enlarged (B). A follow-up MRI (1.5T) image was obtained 26 weeks following the head injury (C,D). The axial ESWAN image displays a rim of hypointensity (arrowheads), with hemosiderin deposits forming along the cerebral convexity (C, D).
Contributed by Hongwei Zhao, Jin Wang, Zhonglie Lu, Qingjie Wu, Haijuan Lv, Hu Liu, Xiangyang Gong
Contributed bu Meltem Özdemir, MD