Ramsay Hunt Syndrome
- Article Author:
- Andrew Crouch
- Article Editor:
- Claudio Andaloro
- Updated:
- 9/27/2020 9:16:41 AM
- For CME on this topic:
- Ramsay Hunt Syndrome CME
- PubMed Link:
- Ramsay Hunt Syndrome
Introduction
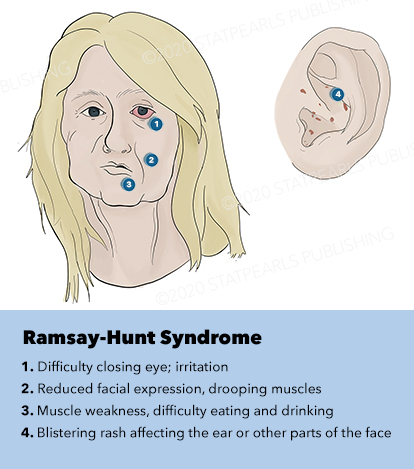
Ramsay Hunt syndrome, also known as herpes zoster oticus or geniculate zoster, is a rare condition that manifests as a complication of the Varicella zoster virus (VZV) that arises in the geniculate ganglion of cranial nerve CVII.[1] Early stages of the VZV infection cause fever and diffuse vesicular rash, a condition that is commonly referred to as chickenpox. After the initial infection, the virus will often remain dormant within various ganglion in the body. The zoster infection is caused by a reactivation of the virus. This can produce linear vesicular rashes along the nerve's distribution, typically involving a single dermatome. The distribution and associated symptoms depend on the nerve involved, and there are many different syndromes associated with this virus. Less than 1% of the cases of zoster involve the facial nerve and result in Ramsay Hunt syndrome.[2] The syndrome is characterized by a classic triad of ipsilateral facial paralysis, otalgia, and vesicles in the auditory canal.[3] Additional symptoms include changes in taste along the anterior two-thirds of the tongue, dry eye, hearing loss, tinnitus, and/or vertigo can be seen with the involvement of the vestibulocochlear nerve. Vesicles often develop after the onset of neurologic symptoms. Vesicles typically appear near the ear but can be seen along the affected side of the face, hard palate, and tongue.
Etiology
Epidemiology
Ramsay Hunt syndrome is a complication of the Varicella zoster virus (VZV). It can affect both immunocompetent and immunocompromised patients. It has an incidence of 5 per 100,000, with females affected 20% more frequently than males. It is considered to account for 12% of all cases of facial nerve paralysis. Those who are immunocompromised have a much more severe disease process.[1] It can present in anyone, and there are cases ranging from 3 months of age to 82 years.[5] Factors that increase the incidence of zoster will increase the incidence of Ramsay Hunt syndrome. These include stress, chemotherapy, immune compromise, and infection.
Pathophysiology
Ramsay Hunt is a complication of the Varicella-zoster virus. The initial infection causes a disseminated vesicular rash with fever, known as Varicella or chickenpox. During this infection, the virus can be spread by respiratory droplets. After the initial state of illness, the virus can remain dormant in the various ganglia throughout the body. The reactivation of the virus, known as zoster or shingles can occur. During this infection, vesicular rashes tend to appear typically effecting a single dermatome. In Ramsay Hunt syndrome, the virus reactivates along the CN VII via the geniculate ganglion. Initial symptoms typically include pain along the ipsilateral side of the face and ear. This typically will present with facial paralysis. Other areas innervated by the nerve can also be affected. This includes the anterior two-thirds of the tongue, the stapedius, and digastric muscles.
The proximity of the infection to the vestibulocochlear nerve can result in hearing loss, tinnitus, and vertigo. The vesicular rash often appears 2 to 3 days after the initial neurologic symptoms. The rash is considered infectious, and the virus is shed from the rash. The virus can also be cultured from tears and saliva. The facial nerve supplies parasympathetic fibers via the chorda tympani to the sublingual and submandibular salivary glands. The facial nerve also supplies parasympathetic input to the lacrimal gland.
Histopathology
Microscopic evaluation with the Tzanck smear can be performed on the fluid obtained from the vesicles. During VCV infections, the smear should find multinucleated giant cells using a Giemsa stain. The sensitivity of the test is very low but has high specificity. It is difficult to distinguish between the VZV and HSV on the stain.[6]
History and Physical
Diagnosis of Ramsay Hunt is a clinical diagnosis and often presents with the triad of ipsilateral facial paralysis, otalgia, and vesicles in the auditory canal. The erythematous vesicular rash formation can be seen over the face, ear, and auditory canal.[3] Often there is a prodrome with pain, fever, and fatigue for 1 to 3 days, followed by vesicles in the external auditory canal with or without tongue involvement. There is an active stage characterized as a rash that progresses from erythematous papules to vesicles. The vesicle will rupture and crust over within 1 to 7 days. The rash can persist for 2 to 3 weeks, leaving an erythematous macular scar. [5]
Due to the geniculate ganglion being close to cranial nerve 8, the vestibulocochlear nerve, patients will also often present with hearing loss, tinnitus, nystagmus, vertigo, nausea, and anesthesia of the anterior two-thirds of the tongue. The onset of vesicles sometimes makes it very hard to differentiate between Ramsay Hunt and Bell palsy. There was one prospective study done showing that 14% will develop vesicles in the auditory canal at a later time after facial paralysis.[5] While much less common, cranial nerves 5 through 12 can be affected as well.[3]
While taking a history, it is important to perform a complete review of symptoms to assess for associated symptoms. Care should be taken to evaluate for evaluation of the nose and eyes. The nose and eyes are not typically involved in Ramsay Hunt syndrome but can be seen in other forms of zoster. Vesicles near the tip of the nose, Hutchinson's sign, can be associated with ocular lesions, and the nose should be evaluated.
Evaluation
The diagnosis of RHS is considered to be a clinical one, and clinical testing is not indicated.[5] The presence of rash, pain, and facial droop is indicative of the condition. Diagnostic modalities such as labs and imaging have not shown to impact prognosis or patient outcomes positively. The Tzanck smear can be performed on fluid obtained from the vesicles. This may show multinucleated giant cells but has low sensitivity and is not routinely performed. PCR analysis of tears, saliva, or fluid from the vesicles has higher sensitivity, approximately 70%, but is not routinely available. Imaging with CT scan is not diagnostic of the condition. MRI may be useful in showing inflammation near the geniculate ganglion. After the diagnosis, audiometry, and otolaryngologist follow up are indicated.
Treatment / Management
VZV infections are generally self-limiting in nature. The main goal of treatment is decreasing the incidence of late complications including facial paralysis and postherpetic neuralgia duration. Multiple studies have shown a significant effect on long term complications with the use of antiviral therapy with steroids.[7] Less effect has been seen in decreasing the duration of infection. Antiviral treatment is recommended for both immunocompetent and immunocompromised patients. There are multiple treatment regimens including acyclovir, valacyclovir, and famciclovir. No definitive difference was seen between these medications. Acyclovir 500 milligrams five times a day is typically the initial choice as it usually the most affordable option. One can also use valacyclovir 1000 mg three times a day which is dosed easier and has been shown to be more effective. Another option is famciclovir 500 mg three times a day. Antiviral treatment is to be for seven to ten days. Some studies have shown a later degeneration of facial nerve up to 21 days and therefore some recommend continuing antivirals for up to 21 days.[1] Corticosteroids are often used. The combination of corticosteroids with antiviral medications has been shown to have improved outcomes compared to antiviral alone.[7] Corticosteroids have multiple side effects and consideration should be taken in each case.[8] Treatment should be started within 72 hours if possible.
Symptomatic management is also important. Analgesia is often needed with Ramsay Hunt syndrome. Acetaminophen or ibuprofen, long-acting opioids can all be used. Tricyclic antidepressants and gabapentin have been shown to effective in the treatment of neuropathic pain and post-herpetic neuralgia. Meclizine and benzodiazepines can be effective in the treatment of vertigo associated with the condition. Artificial tears and eye patches should be used on the affected eye to prevent corneal abrasions and ulcers. Audiometry and otolaryngologist follow up should be included if the patient has hearing changes. Medications have not shown to have any effect on hearing loss.
Differential Diagnosis
Differential diagnosis includes primary varicella, bell palsy, stroke, poison ivy, cellulitis, herpes simplex virus, trigeminal neuralgia, vertigo, HSV keratitis. It is crucial to be able to distinguish between the peripheral cause for facial paralysis for Ramsay Hunt and Bell Palsy versus a central cause such as a stroke.[5]
Prognosis
Reports on recovery show significant variance. Full recovery of facial paralysis can vary from 27.3% to 70% if proper treatment has been started within 72 hours of symptom onset. If treatment has not been started within 72 hours, full recovery chances decrease to 50%. The main factor that affects prognosis is the severity of symptoms at onset.[3][7] The prognosis of Bell palsy is considered to be better than Ramsay Hunt syndrome. Age has been associated with a poorer prognosis for Ramsay Hunt syndrome.[8] Greater than half of the patients reported developing postherpetic neuralgia.
Complications
Complications include permanent facial paralysis, corneal abrasions, corneal ulcers, postherpetic neuralgia, hearing loss, tinnitus. Sometimes, it has been documented that the virus can spread to other nerves and cause motor weakness and neuropathic pain. Postherpetic neuralgia is pain that persists at the site and can occur for greater than 3 months even after the lesions have completely healed. Cranial nerves that most often become affected besides the seventh cranial nerve are cranial nerves five, nine, and ten. The most common nerve distributions can occur in the thoracic, lumbar followed by trigeminal and cervical nerves.[3]
Consultations
Ramsay Hunt syndrome is typically managed as an outpatient with close follow up with their primary care provider. Outpatient otolaryngology consultation can be considered. Pregnant women can be managed as an outpatient but should follow closely with their obstetrics provider. For those who are severely immunocompromised or who need to be in isolation, then admission to the hospital is warranted.
Deterrence and Patient Education
For patient's education, it is essential to advise them on the use of artificial tears and possibly an eye cover at night to avoid corneal ulcers or abrasions since they cannot close their eyes and have decreased ability to lubricate their eyes. Always counsel patient's on postherpetic neuralgia as it can be very severe and painful and can often last longer than 3 months even after all the lesions have healed. They will need long term analgesia and often referral to a pain specialist if it continues to be painful. For patients early on in the clinical phase, avoid contact with people who are pregnant or immunocompromised until the lesions are healed and crusted over. It is important to advise patients over 60 years old to obtain the VZV vaccine unless they are immunocompromised. Follow up with their primary care provider is imperative to assess progress and continue to provide supportive care.
Pearls and Other Issues
It is crucial to expose the skin of the patient to see which dermatomes are involved. It is also important to look in the ears to assess for the vesicles; otherwise, this diagnosis can be easily missed. Do not forget to advise patients of all complications, including facial paralysis and postherpetic neuralgia.
Enhancing Healthcare Team Outcomes
Ramsay Hunt syndrome is associated with multiple long-term complications, including hearing loss, persistent facial droop, and chronic pain. Early identification can be difficult due to the fact that the neurologic symptoms often precede the rash. Due to this fact, the condition can be mistaken for Bell palsy and other syndromes that cause facial paralysis. In the early stages, the sensory symptoms and pain can help differentiate Ramsay Hunt syndrome from Bell palsy. Radiology and viral cultures have not been shown significantly to be necessary for the diagnosis.
Early identification and treatment are key, as intervention can lead to improved outcomes. Multiple studies have shown decreased rates of long-term complications such as pain and facial paralysis if treatment is instituted early in the disease course. With the best outcomes seen in groups using both acyclovir and steroids, versus either drug alone.[7] [Level 1]
(Click Image to Enlarge)
(Click Image to Enlarge)
(Click Image to Enlarge)